Thoracic outlet syndrome
| Thoracic outlet syndrome | |
|---|---|
 | |
| The right brachial plexus, viewed from in front. | |
| Specialty | Vascular surgery, thoracic surgery |
| Symptoms | Pain, weakness, loss of muscle at the base of the thumb, swelling, paleness, bluish coloration[1][2] |
| Usual onset | 20 to 50 years of age[1] |
| Types | Neurogenic, venous, arterial[1] |
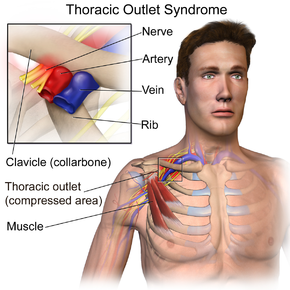
| Causes | Compression of the nerves, arteries, or veins in the passageway from the lower neck to the armpit[1] |
| Risk factors | Trauma, repetitive arm movements, tumors, pregnancy, cervical rib[1] |
| Diagnostic method | Nerve conduction studies, medical imaging[1] |
| Differential diagnosis | Rotator cuff tear, cervical disc disorders, fibromyalgia, multiple sclerosis, complex regional pain syndrome[1] |
| Treatment | Pain medication, surgery[1][2] |
| Frequency | ~1%[3] |
Thoracic outlet syndrome (TOS) is a condition in which there is compression of the nerves, arteries, or veins in the passageway from the lower neck to the armpit.[1] There are three main types: neurogenic, venous, and arterial.[1] The neurogenic type is the most common and presents with pain, weakness, and occasionally loss of muscle at the base of the thumb.[1][2] The venous type results in swelling, pain, and possibly a bluish coloration of the arm.[2] The arterial type results in pain, coldness, and paleness of the arm.[2]
TOS may result from trauma, repetitive arm movements, tumors, pregnancy, or anatomical variations such as a cervical rib.[1] The diagnosis may be supported by nerve conduction studies and medical imaging.[1] Other conditions that can produce similar symptoms include rotator cuff tear, cervical disc disorders, fibromyalgia, multiple sclerosis, and complex regional pain syndrome.[1]
Initial treatment for the neurogenic type is with exercises to strengthen the chest muscles and improve posture.[1] NSAIDs such as naproxen may be used for pain.[1] Surgery is typically done for the arterial and venous types and for the neurogenic type if it does not improve with other treatments.[1][2] Blood thinners may be used to treat or prevent blood clots.[1] The condition affects about 1% of the population.[3] It is more common in women than men and it occurs most commonly between 20 and 50 years of age.[1] The condition was first described in 1818 and the current term "thoracic outlet syndrome" first used in 1956.[2][4]
Signs and symptoms
TOS affects mainly the upper limbs, with signs and symptoms manifesting in the shoulders, neck, arms and hands. Pain can be present on an intermittent or permanent basis. It can be sharp/stabbing, burning, or aching. TOS can involve only part of the hand (as in the pinky and adjacent half of the ring finger), all of the hand, or the inner aspect of the forearm and upper arm. Pain can also be in the side of the neck, the pectoral area below the clavicle, the armpit/axillary area, and the upper back (i.e., the trapezius and rhomboid area). Discoloration of the hands, one hand colder than the other hand, weakness of the hand and arm muscles, and tingling are commonly present.[citation needed]
TOS is often the underlying cause of refractory upper limb conditions like frozen shoulder and carpal tunnel syndrome that frequently defy standard treatment protocols[citation needed]. TOS can be related to forward head posture[citation needed].
A painful, swollen and blue arm, particularly when occurring after strenuous physical activity, could be the first sign of a subclavian vein compression related with an unknown TOS and complicated by thrombosis (blood clots), the so-called Paget–Schroetter syndrome or effort-induced thrombosis.
TOS can be related to cerebrovascular arterial insufficiency when affecting the subclavian artery.[5] It also can affect the vertebral artery, in which case it could produce vision disturbances, including transient blindness,[6] and embolic cerebral infarction.[7]
TOS can also lead to eye problems and vision loss as a circumstance of vertebral artery compression. Although very rare, if compression of the brain stem is also involved in an individual presentation of TOS, transient blindness may occur while the head is held in certain positions.[8] If left untreated, TOS can lead to neurological deficits as a result of the hypoperfusion and hypometabolism of certain areas of the brain and cerebellum.[9]
Causes
TOS can be attributed to one or more of the following factors:[10]
- Congenital abnormalities are frequently found in persons with TOS. These include cervical rib, prolonged transverse process, and muscular abnormalities (e.g., in the scalenus anterior muscle, a sickle-shaped scalenus medius) or fibrous connective tissue anomalies.[10]
- Trauma (e.g., whiplash injuries) or repetitive strain is frequently implicated.[10]
- Rarer acquired causes include tumors (especially pancoast tumor), hyperostosis, and osteomyelitis[10]
Diagnosis
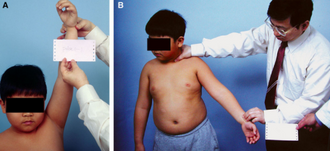
Adson's sign and the costoclavicular maneuver lack specificity and sensitivity and should comprise only a small part of the mandatory comprehensive history and physical examination undertaken with a patient suspected of having TOS. There is currently no single clinical sign that makes the diagnosis of TOS with any degree of certainty.
Additional maneuvers that may be abnormal in TOS include Wright's Test, which involves hyperabducting the arms over the head with some extension and evaluating for loss of radial pulses or signs of blanching of the skin in the hands indicating a decrease in blood flow with the maneuver. The "compression test" is also used, exerting pressure between the clavicle and medial humeral head causes radiation of pain and/or numbness into the affected arm.[11]
Doppler arteriography, with probes at the fingertips and arms, tests the force and "smoothness" of the blood flow through the radial arteries, with and without having the patient perform various arm maneuvers (which causes compression of the subclavian artery at the thoracic outlet). The movements can elicit symptoms of pain and numbness and produce graphs with diminished arterial blood flow to the fingertips, providing strong evidence of impingement of the subclavian artery at the thoracic outlet.[12] Doppler arteriography does not utilize probes at the fingertips and arms, and in this case is likely being confused with plethysmography, which is a different method that utilizes ultrasound without direct visualization of the affected vessels. Doppler ultrasound (not really 'arteriography') would not be used at the radial artery in order to make the diagnosis of TOS. Finally, even if a Doppler study of the appropriate artery were to be positive, it would not diagnose neurogenic TOS, by far the most common subtype of TOS. There is plenty of evidence in the medical literature to show that arterial compression does not equate to brachial plexus compression, although they may occur together, in varying degrees. Additionally, arterial compression by itself does not make the diagnosis of arterial TOS (the rarest form of TOS). Lesser degrees of arterial compression have been shown in normal individuals in various arm positions and are thought to be of little significance without the other criteria for arterial TOS.
Classification
By structures affected and symptomatology
There are three main types of TOS, named according to the cause of the symptoms; however, these three classifications have been coming into disfavor because TOS can involve all three types of compression to various degrees. The compression can occur in three anatomical structures (arteries, veins and nerves), it can be isolated, or, more commonly, two or three of the structures are compressed to greater or lesser degrees. In addition, the compressive forces can be of different magnitude in each affected structure. Therefore, symptoms can be variable.[13]
- Neurogenic TOS includes disorders produced by compression of components of the brachial plexus nerves. The neurogenic form of TOS accounts for 95% of all cases of TOS.[14]
- Arterial TOS is due to compression of the subclavian artery.[14] This is less than one percent of cases.[2]
- Venous TOS is due to compression of the subclavian vein.[14] This makes up about 4% of cases.[2]
By event
There are many causes of TOS. The most frequent cause is trauma, either sudden (as in a clavicle fracture caused by a car accident), or repetitive (as in a legal secretary who works with his/her hands, wrists, and arms at a fast paced desk station with non-ergonomic posture for many years)[citation needed]. TOS is also found in certain occupations involving lots of lifting of the arms and repetitive use of the wrists and arms[citation needed].
One cause of arterial compression is trauma, and a recent case involving fracture of the clavicle has been reported.[15]
The two groups of people most likely to develop TOS are those suffering from neck injuries due to traffic accidents and those who use computers in non-ergonomic postures for extended periods of time.[citation needed] TOS is frequently a repetitive stress injury (RSI) caused by certain types of work environments[citation needed]. Other groups which may develop TOS are athletes who frequently raise their arms above the head (such as swimmers, volleyball players, dancers, badminton players, baseball pitchers, and weightlifters), rock climbers, electricians who work long hours with their hands above their heads, and some musicians[citation needed].
By structure causing constriction
It is also possible to classify TOS by the location of the obstruction:
- Anterior scalene syndrome (compression on brachial plexus and/or subclavian artery caused by muscle growth).
- Cervical rib syndrome (compression on brachial plexus and/or subclavian artery caused by bone growth).
- Costoclavicular syndrome (narrowing between the clavicle and the first rib) – diagnosed with the costoclavicular maneuver.
Some people are born with an extra incomplete and very small rib above their first rib, which protrudes out into the superior thoracic outlet space. This rudimentary rib causes fibrous changes around the brachial plexus nerves, inducing compression and causing the symptoms and signs of TOS. This is called a "cervical rib" because of its attachment to C-7 (the 7th cervical vertebra), and its surgical removal is almost always recommended. The symptoms of TOS can first appear in the early teen years as a child is becoming more athletic.
Treatment
Evidence for the treatment of thoracic outlet syndrome as of 2014 is poor.[16]
Physical measures
Stretching, occupational and physical therapy are common non-invasive approaches used in the treatment of TOS. The goal of stretching is to relieve compression in the thoracic cavity, reduce blood vessel and nerve impingement, and realign the bones, muscles, ligaments, or tendons that are causing the problem.
- One commonly prescribed set of stretches includes moving the shoulders anteriorly (forward – called "hunching"), then back to a neutral position, then extending them posteriorly (backward, called "arching"), then back to neutral, followed by lifting the shoulders up as high as possible, and then back down to neutral, repeated in cycles as tolerated.
- Another set of stretches involves tilting and extending the neck opposite to the side of the injury while keeping the injured arm down or wrapped around the back.
- Occupational or Physical therapy can include passive or active range of motion exercises, working up to weighted or restricted sets (as tolerated).
TOS is rapidly aggravated by poor posture.[citation needed] Active breathing exercises and ergonomic desk setup and motion practices can help maintain active posture.[citation needed] Often the muscles in the back become weak due to prolonged (years of) "hunching" and other poor postures.[citation needed]
Ice can be used to decrease inflammation of sore or injured muscles. Heat can also aid in relieving sore muscles by improving blood circulation to them. While the whole arm generally feels painful in TOS, some relief can be seen when ice or heat is intermittently applied to the thoracic region (collar bone, armpit, or shoulder blades).
Medications
In a review, botox was compared to a placebo injected into the scalene muscles. No effect in terms of pain relief or improved movement was noted. However in a six-months follow-up, paresthesia (abnormal sensations such as in pins and needles) was seen to be significantly improved.[16]
Surgery
Surgical approaches have also been used successfully in TOS. Microsurgery can be used approaching the area from above the collar bone (supraclavicular) followed by neurolysis of the brachial plexus, removal of the scalene muscle (scalenectomy), and the release of the underlying (subclavicular) blood vessels. This approach avoids the use of resection, and has been found to be an effective treatment.[17] In cases where the first rib (or a fibrous band extending from the first rib) is compressing a vein, artery, or the nerve bundle, part of the first rib and any compressive fibrous tissue, can be removed in a first rib resection and thoracic outlet decompression surgical procedure; scalene muscles may also need to be removed (scalenectomy). This allows increased blood flow and the reduction of nerve compression.[18] In some cases there may be a rudimentary rib or a cervical rib that can be causing the compression, which can be removed using the same technique.
Physical therapy is often used before and after the operation to improve recovery time and outcomes. Potential complications include pneumothorax, infection, loss of sensation, motor problems, subclavian vessel damage, and, as in all surgeries, a very small risk of permanent serious injury or death.
Notable cases
- Sports
Several Major League Baseball players, especially pitchers, have been diagnosed with thoracic outlet syndrome, including Matt Harvey,[19] Chris Carpenter,[20] Jaime Garcia,[21] Shaun Marcum,[22] Matt Harrison,[23] Clayton Richard,[24] and Noah Lowry.[25] Starting pitcher Chris Young, who previously struggled with shoulder problems, underwent surgery for TOS in 2013 and felt "completely different" post-recovery.[26] Young exceeded expectations on his return to the major leagues at age 35, becoming a valuable member of the 2014 Seattle Mariners' starting rotation.[27]
NHL defenseman Adam McQuaid was diagnosed with TOS in September 2012, and as a result was nominated for the Bill Masterton Memorial Trophy.[28] Forward Chris Kreider was diagnosed with a malformed rib in 2017. Kreider dealt with multiple symptoms prior to the diagnosis, such as shortness of breath on the ice, swelling/numbness in his right arm, coughing up blood and a blod clot in his right arm. Kreider underwent successful surgery to resect a rib in January 2018 (the same surgery as TOS) and has performed well since returning to the Rangers.[29]
NBA guard Markelle Fultz was diagnosed with TOS in December 2018.[30][31]
UFC fighter Matt Serra had a rib removed to alleviate TOS.[32]
- Music
Musician Isaac Hanson had a pulmonary embolism as a consequence of thoracic outlet syndrome.[33]
The Japanese band Maria disbanded in 2010 due to drummer Tattsu's TOS which made it impossible for her to continue playing.[34]
In 2015, singer Tamar Braxton had to leave Dancing With The Stars due to TOS.[35]
See also
- May–Thurner syndrome – a similar compressive pathology involving the left common iliac vein
- Backpack palsy – a similar compressive pathology involving the long thoracic nerve, or adjacent brachial plexis nerves
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 1.18 "NINDS Thoracic Outlet Syndrome Information Page". NINDS. December 28, 2011. Archived from the original on July 27, 2016. Retrieved August 19, 2016.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 2.8 Kuhn, JE; Lebus V, GF; Bible, JE (April 2015). "Thoracic outlet syndrome". The Journal of the American Academy of Orthopaedic Surgeons. 23 (4): 222–32. doi:10.5435/jaaos-d-13-00215. PMID 25808686.
- ↑ 3.0 3.1 Moore, Wesley S. (2012). Vascular and Endovascular Surgery: A Comprehensive Review (8 ed.). Elsevier Health Sciences. p. 524. ISBN 978-1455753864. Archived from the original on June 21, 2020. Retrieved September 16, 2017.
- ↑ Illig, Karl A.; Thompson, Robert W.; Freischlag, Julie Ann; Donahue, Dean M.; Jordan, Sheldon E.; Edgelow, Peter I. (2014). Thoracic Outlet Syndrome. Springer Science & Business Media. p. 25. ISBN 9781447143666. Archived from the original on June 21, 2020. Retrieved September 16, 2017.
- ↑ Thetter, O; Van Dongen, RJ; Barwegen, MG (1985). "The thoracic outlet compression syndrome and its vascular complications". Zentralblatt für Chirurgie. 110 (8): 449–56. PMID 4002908.
- ↑ Sell, James J.; Rael, Jesse R.; Orrison, William W. (1994). "Rotational vertebrobasilar insufficiency as a component of thoracic outlet syndrome resulting in transient blindness". Journal of Neurosurgery. 81 (4): 617–9. doi:10.3171/jns.1994.81.4.0617. PMID 7931599.
- ↑ Nishibe, T; Kunihara, T; Kudo, FA; Adachi, A; Shiiya, N; Murashita, T; Matusi, Y; Yasuda, K (2000). "Arterial thoracic outlet syndrome with embolic cerebral infarction. Report of a case". Panminerva Medica. 42 (4): 295–7. PMID 11294095.
- ↑ Sell JJ, Rael JR, Orrison WW (October 1994). "Rotational vertebrobasilar insufficiency as a component of thoracic outlet syndrome resulting in transient blindness. Case report". J. Neurosurg. 81: 617–9. doi:10.3171/jns.1994.81.4.0617. PMID 7931599.
- ↑ Fernandez Noda, MD, Esteban. "Neck and brain transitory vascular compression causing neurological complications. Results of surgical treatment on 1,300 patients". Neck and Brain Vascular Compression Causing Neurological Complications.
- ↑ 10.0 10.1 10.2 10.3 Laulan J, Fouquet B, Rodaix C, Jauffret P, Roquelaure Y, Descatha A (September 2011). "Thoracic outlet syndrome: definition, aetiological factors, diagnosis, management and occupational impact". J Occup Rehabil. 21 (3): 366–73. doi:10.1007/s10926-010-9278-9. PMC 3526474. PMID 21193950. Archived from the original on July 19, 2018. Retrieved November 4, 2018.
- ↑ [1] Archived May 17, 2013, at the Wayback Machine
- ↑ Thoracic outlet syndrome Archived December 9, 2008, at the Wayback Machine Mount Sinai Hospital, New York
- ↑ Ambrad-Chalela, Esteban; Thomas, George I.; Johansen, Kaj H. (2004). "Recurrent neurogenic thoracic outlet syndrome". The American Journal of Surgery. 187 (4): 505–10. doi:10.1016/j.amjsurg.2003.12.050. PMID 15041500.
- ↑ 14.0 14.1 14.2 Fugate, Mark W.; Rotellini-Coltvet, Lisa; Freischlag, Julie A. (2009). "Current management of thoracic outlet syndrome". Current Treatment Options in Cardiovascular Medicine. 11 (2): 176–83. doi:10.1007/s11936-009-0018-4. PMID 19289030.
- ↑ Burnand, K. M.; Lagocki, S.; Lahiri, R. P.; Tang, T. Y.; Patel, A. D.; Clarke, J. M. F. (2010). "Persistent subclavian artery stenosis following surgical repair of non-union of a fractured clavicle" (PDF). Grand Rounds. 10: 55–8. doi:10.1102/1470-5206.2010.0012 (inactive January 22, 2020). Archived from the original (PDF) on July 11, 2011.
{{cite journal}}: CS1 maint: DOI inactive as of January 2020 (link) - ↑ 16.0 16.1 Povlsen, B; Hansson, T; Povlsen, SD (November 26, 2014). "Treatment for thoracic outlet syndrome". The Cochrane Database of Systematic Reviews. 11 (11): CD007218. doi:10.1002/14651858.CD007218.pub3. PMID 25427003.
- ↑ Rochkind, S; Shemesh, M; Patish, H; Graif, M; Segev, Y; Salame, K; Shifrin, E; Alon, M (2007). Thoracic outlet syndrome: a multidisciplinary problem with a perspective for microsurgical management without rib resection. Acta Neurochirurgica Supplement. Acta Neurochirurgica Supplementum. Vol. 100. pp. 145–7. doi:10.1007/978-3-211-72958-8_31. ISBN 978-3-211-72955-7. PMID 17985565.
- ↑ Köknel Talu, G (April 2005). "Thoracic outlet syndrome". Agri : Agri (Algoloji) Dernegi'nin Yayin Organidir = the Journal of the Turkish Society of Algology. 17 (2): 5–9. PMID 15977087.
- ↑ "Harvey determined to regain dominant form". February 13, 2017. Archived from the original on July 24, 2019. Retrieved May 13, 2019.
- ↑ Carpenter's throwing session canceled Archived October 29, 2013, at the Wayback Machine, MLB.com (July 2, 2012)
- ↑ Garcia to have season-ending surgery for nerve issue Archived July 14, 2014, at the Wayback Machine, MLB.com (July 5, 2014)
- ↑ Marcum needs thoracic outlet syndrome surgery Archived July 12, 2013, at the Wayback Machine, Rotoworld.com (July 9, 2013)
- ↑ Fort Worth Star-Telegram (September 7, 2013). "Foul Territory: Rangers' Matt Harrison facing surgery for thoracic outlet syndrome on right shoulder". Sportsblogs.star-telegram.com. Archived from the original on October 29, 2013. Retrieved October 26, 2013.
- ↑ "Clayton Richard's Story". Center for Thoracic Outlet Syndrome. Washington University School of Medicine in St Louis. Archived from the original on April 16, 2016. Retrieved April 9, 2016.
- ↑ John Shea; Henry Schulman (May 20, 2009). "San Francisco Chronicle: Lowry's agent lashes out". Sfgate.com. Archived from the original on May 23, 2009. Retrieved October 26, 2013.
- ↑ Wagner, James (March 12, 2014). "Nationals Journal: Back from injury, Chris Young hopes to be part of the Nationals". The Washington Post. Archived from the original on October 27, 2014. Retrieved October 19, 2014.
- ↑ Stecker, Brent (August 18, 2014). "Mariners' Chris Young has strong case for Comeback award". 710Sports.com. Archived from the original on August 22, 2014. Retrieved October 19, 2014.
- ↑ Marrapese-Burrell, Nancy. "McQuaid a Masterton Trophy Finalist". Boston Globe. Archived from the original on June 8, 2013. Retrieved June 8, 2013.
- ↑ "Inside Chris Kreider's journey back to the ice". August 2, 2018. Archived from the original on November 2, 2019. Retrieved December 4, 2018.
- ↑ "Markelle Fultz diagnosed with nerve condition". Archived from the original on March 28, 2019. Retrieved December 4, 2018.
- ↑ Wojnarowski, Adrian. "76ers' Markelle Fultz expected to miss 3-6 weeks for shoulder rehabilitation". ESPN. Archived from the original on October 30, 2019. Retrieved December 4, 2018.
- ↑ "Health scare leads to former UFC champion Matt Serra probably walking away from MMA". Bloody Elbow. May 22, 2013. Archived from the original on October 29, 2013. Retrieved October 26, 2013.
- ↑ "People Magazine". Archived from the original on October 18, 2007. Retrieved January 1, 2008.
- ↑ "MARIA今後の活動に関するお知らせ" (in Japanese). MARIA6. Archived from the original on February 11, 2010. Retrieved February 16, 2010.
{{cite web}}: CS1 maint: unrecognized language (link) - ↑ "Tamar Braxton Opens up About Health Crisis, Rib Removal". December 17, 2015. Archived from the original on May 16, 2019. Retrieved December 5, 2018.
External links
| Classification | |
|---|---|
| External resources |
- Pages with script errors
- Webarchive template wayback links
- CS1 maint: DOI inactive as of January 2020
- CS1 maint: unrecognized language
- Articles with hatnote templates targeting a nonexistent page
- Use mdy dates from July 2014
- Articles with invalid date parameter in template
- All articles with unsourced statements
- Articles with unsourced statements from May 2018
- Articles with unsourced statements from February 2018
- Articles with unsourced statements from April 2018
- Articles with unsourced statements from October 2012
- Peripheral nervous system disorders
- Syndromes
- RTT
- RTTEM