Third-degree atrioventricular block
| Third-degree atrioventricular block | |
|---|---|
| Other names: Complete heart block, third degree heart block[1] | |
 | |
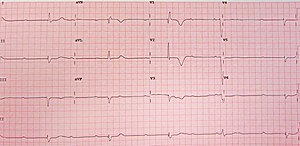
| Rhythm strip showing third-degree AV block | |
| Specialty | Cardiology |
| Symptoms | Tiredness, shortness of breath, chest pain, syncope[1] |
| Complications | Sudden cardiac death[1] |
| Causes | Unclear, ischemic heart disease, certain medications, electrolyte abnormalities, Lyme disease, lupus, following heart surgery[1] |
| Diagnostic method | Electrocardiogram (ECG)[1] |
| Differential diagnosis | Idioventricular rhythms, second-degree AV block[1] |
| Treatment | Dopamine, epinephrine, pacemaker[1] |
| Frequency | 3 per 10,000 people per year[1] |
Third-degree atrioventricular block (third-degree AV block) is were the electrical signal from the upper chambers of the heart is unable to make it to the lower chambers.[1] Symptoms may include tiredness, shortness of breath, chest pain, and syncope.[1] Complications may include sudden cardiac death.[1]
Causes may include ischemic heart disease, certain medications, electrolyte abnormalities, Lyme disease, lupus, and following heart surgery.[1] Medications that may be involved include antiarrhythmics and digoxin.[1] In some cases the cause is unclear.[1] Diagnosis is by electrocardiogram (ECG), which typically shows a ventricular rate of less than 50 BPM and independent but faster atrial activity.[1] The QRS complex can be narrow or wide.[1] It is a type of atrioventricular block.[2]
The heartrate may be raised with a dopamine or epinephrine infusion.[1] This may be followed by transcutaneous or transvenous pacing and eventually a permanent pacemaker.[1] While recommended, atropine is generally not effective.[1] Third-degree AV block is rare, newly affecting about 3 in 10,000 people per year.[1] The condition was first identified in an animal model in 1852 by Hermann Stannius.[3][4]
Signs and symptoms
People with third-degree AV block typically experience severe bradycardia (an abnormally low measured heart rate), hypotension, and at times, hemodynamic instability.[5]
Cause
Many conditions can cause third-degree heart block, but the most common cause is coronary ischemia. Progressive degeneration of the electrical conduction system of the heart can lead to third-degree heart block. This may be preceded by first-degree AV block, second-degree AV block, bundle branch block, or bifascicular block. In addition, acute myocardial infarction may present with third-degree AV block.
An inferior wall myocardial infarction may cause damage to the AV node, causing third-degree heart block. In this case, the damage is usually transitory. Studies have shown that third-degree heart block in the setting of an inferior wall myocardial infarction typically resolves within 2 weeks.[6] The escape rhythm typically originates in the AV junction, producing a narrow complex escape rhythm.
An anterior wall myocardial infarction may damage the distal conduction system of the heart, causing third-degree heart block. This is typically extensive, permanent damage to the conduction system, necessitating a permanent pacemaker to be placed.[7] The escape rhythm typically originates in the ventricles, producing a wide complex escape rhythm.
Third-degree heart block may also be congenital and has been linked to the presence of lupus in the mother.[8] It is thought that maternal antibodies may cross the placenta and attack the heart tissue during gestation. The cause of congenital third-degree heart block in many people is unknown.
Hyperkalemia in those with previous cardiac disease[9] and Lyme disease can also result in third-degree heart block.[10]
Diagnosis
Diagnosis is by an electrocardiogram (ECG)
- The P waves with a regular P-to-P interval (in other words, a sinus rhythm) represent the first rhythm.
- The QRS complexes with a regular R-to-R interval represent the second rhythm. The PR interval will be variable, as the hallmark of complete heart block is lack of any apparent relationship between P waves and QRS complexes.
-
12-lead ECG showing complete heart block
-
Atrial tachycardia with complete A-V block and resulting junctional escape
Treatment
Medications
Atropine is often used as a first line treatment of a third-degree heart block in the presence of a narrow QRS which indicates a nodal block, but, may have little to no effect in an infra-nodal block.[11][12] Atropine works by reducing vagal stimulation through the AV node but will not be effective in those who have had a previous heart transplant.[13] Other drugs may be utilized such as epinephrine or dopamine which have positive chronotropic effects and may increase the heart rate.[14]
Pacemaker
Treatment in emergency situations can involve electrical transcutaneous pacing in those who are acutely hemodynamically unstable and can be used regardless of the persons level of consciousness.[15] Sedative agents such as a benzodiazapine or opiate may be used in conjunction with transcutaneous pacing to reduce the pain caused by the intervention.[14][15]
Third-degree AV block can be treated more permanently with the use of a dual-chamber artificial pacemaker.[16] This type of device typically listens for a pulse from the SA node via lead in the right atrium and sends a pulse via a lead to the right ventricle at an appropriate delay, driving both the right and left ventricles. Pacemakers in this role are usually programmed to enforce a minimum heart rate and to record instances of atrial flutter and atrial fibrillation, two common secondary conditions that can accompany third-degree AV block. Since pacemaker correction of third-degree block requires full-time pacing of the ventricles, a potential side effect is pacemaker syndrome, and may necessitate use of a biventricular pacemaker, which has an additional 3rd lead placed in a vein in the left ventricle, providing a more coordinated pacing of both ventricles.
Other
As with other forms of heart block, secondary prevention may also include medicines to control blood pressure and atrial fibrillation, as well as lifestyle and dietary changes to reduce risk factors associated with heart attack and stroke.
In cases of suspected beta-blocker overdose, the heart-block may be treated with pharmacological agents to reverse the underlying cause with the use of glucagon. In the case of a calcium channel blocker overdose treated with calcium chloride and digitalis toxicity may be treated with the digoxin immune Fab.[17]
Prognosis
The prognosis of people with complete heart block is generally poor without therapy.[18]
Epidemiology
Third-degree AV block is rare, newly affecting about 3 in 10,000 people per year.[1] Congenital third-degree heart block occurs in about 1 in 20,000 live births.[19]
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 1.18 1.19 1.20 Knabben, V; Chhabra, L; Slane, M (January 2020). "Third-Degree Atrioventricular Block". PMID 31424783.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ Kashou, AH; Goyal, A; Nguyen, T; Chhabra, L (January 2020). "Atrioventricular Block". PMID 29083636.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ Saksena, Sanjeev; Camm, A. John (2011). Electrophysiological Disorders of the Heart E-Book: Expert Consult. Elsevier Health Sciences. p. 521. ISBN 978-1-4377-0971-1. Archived from the original on 2021-08-28. Retrieved 2020-12-29.
- ↑ Valentinuzzi, ME (November 2017). "Sinoatrial and Atrioventricular Blocks: Who First Described Them and How? [Retrospectroscope]". IEEE pulse. 8 (6): 62–66. doi:10.1109/MPUL.2017.2750859. PMID 29155381.
- ↑ "Heart Block". NHS Choices. National Health Service (UK). Archived from the original on 3 October 2017. Retrieved 25 August 2015.
- ↑ Sclarovsky, S; Strasberg, B; Hirshberg, A; Arditi, A; Lewin, RF; Agmon, J (July 1984). "Advanced early and late atrioventricular block in acute inferior wall myocardial infarction". American Heart Journal. 108 (1): 19–24. doi:10.1016/0002-8703(84)90539-8. PMID 6731277.
- ↑ Dorney, E (September 1981). "The role of pacemaker therapy in acute myocardial infarction". Primary Care. 8 (3): 509–17. PMID 7031733.
- ↑ Brucato, A; Previtali, E; Ramoni, V; Ghidoni, S (September 2010). "Arrhythmias presenting in neonatal lupus" (PDF). Scandinavian Journal of Immunology. 72 (3): 198–204. doi:10.1111/j.1365-3083.2010.02441.x. hdl:2434/635678. PMID 20696016. Archived (PDF) from the original on 2020-06-02. Retrieved 2019-09-02.
- ↑ Sohoni A, Perez B, Singh A (2010). "Wenckebach Block due to Hyperkalemia: A Case Report". Emerg Med Int. 2010: 879751. doi:10.1155/2010/879751. PMC 3200192. PMID 22046534.
- ↑ Forrester, JD; Mead, P (October 2014). "Third-degree heart block associated with lyme carditis: review of published cases". Clinical Infectious Diseases. 59 (7): 996–1000. doi:10.1093/cid/ciu411. PMID 24879781.
- ↑ Tintinalli's emergency medicine : a comprehensive study guide. Tintinalli, Judith E.,, Stapczynski, J. Stephan,, Ma, O. John,, Yealy, Donald M.,, Meckler, Garth D.,, Cline, David, 1956- (Eighth ed.). New York. 2015-11-10. p. 123. ISBN 9780071794763. OCLC 915775025.
{{cite book}}: CS1 maint: others (link) - ↑ "Peri-arrest arrhythmias". Resuscitation guidelines. Resuscitation Council UK. Retrieved 25 August 2015.
{{cite web}}: CS1 maint: url-status (link) - ↑ "Third-Degree Atrioventricular Block (Complete Heart Block) Treatment & Management: Approach Considerations, Initial Management Considerations, Atropine and Transcutaneous/Transvenous Pacing". 2018-07-05. Archived from the original on 2018-07-23. Retrieved 2018-07-23.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ 14.0 14.1 Oxford textbook of critical care. Webb, Andrew R. (Andrew Roy),, Angus, D. C. (Derek C.), 1962-, Finfer, Simon,, Gattinoni, Luciano,, Singer, Mervyn (Second ed.). Oxford. 2016-05-26. pp. 730–735. ISBN 9780199600830. OCLC 954059445.
{{cite book}}: CS1 maint: others (link) - ↑ 15.0 15.1 Rosen's emergency medicine : concepts and clinical practice. Walls, Ron M.,, Hockberger, Robert S.,, Gausche-Hill, Marianne (Ninth ed.). Philadelphia, PA. 2017-03-09. p. 959. ISBN 9780323390163. OCLC 989157341.
{{cite book}}: CS1 maint: others (link) - ↑ Dretzke, J.; et al. "Compared to single chamber ventricular pacemakers, dual chamber pacemakers may reduce the incidence of complications in people with sick sinus syndrome and atrioventricular block". Cochrane reviews. Archived from the original on 23 September 2015. Retrieved 25 August 2015.
- ↑ "Atrioventricular block, Treatment Options". BMJ Best Practice. BMJ (British Medical Journal). Archived from the original on 2 June 2020. Retrieved 25 August 2015.
- ↑ Edhag O, Swahn A (1976). "Prognosis of patients with complete heart block or arrhythmic syncope who were not treated with artificial pacemakers. A long-term follow-up study of 101 patients". Acta Med Scand. 200 (6): 457–63. doi:10.1111/j.0954-6820.1976.tb08264.x. PMID 1015354.
- ↑ Saksena, Sanjeev; Camm, A. John (2011). Electrophysiological Disorders of the Heart E-Book: Expert Consult. Elsevier Health Sciences. p. 521. ISBN 978-1-4377-0971-1. Archived from the original on 2021-08-28. Retrieved 2020-12-29.
External links
| Classification | |
|---|---|
| External resources |