Systemic vasculitis
| Systemic vasculitus | |
|---|---|
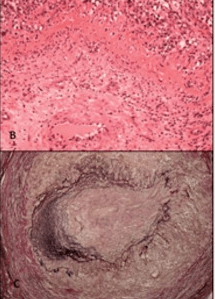 | |
| b,c) Giant-cell arteritis | |
Systemic vasculitis, also called systemic necrotizing vasculitus,[1] is a category of vasculitis,[2] comprising vasculitides that present with necrosis.[3]
Examples include giant cell arteritis,[4] microscopic polyangiitis, and granulomatosis with polyangiitis.
ICD-10 uses the variant "necrotizing vasculopathy". ICD-9, while classifying these conditions together, does not use a dedicated phrase, instead calling them "polyarteritis nodosa and allied conditions".
When using the influential classification known as the "Chapel Hill Consensus Conference", the terms "systemic vasculitis" or "primary systemic vasculitides" are commonly used.[5][6][7] Although the word necrotizing is omitted, the conditions described are largely the same.
Classification
Large vessel vasculitis
Giant-cell arteritis and Takayasu's arteritis have much in common,[8] but usually affect patients of different ages,[9] with Takayasu's arteritis affecting younger people, and giant-cell arteritis having a later age of onset.
Aortitis can also be considered a large-vessel disease.[10]
Takayasu arteritis. Primarily affects the aorta and its main branches. At least three out of six criteria yields sensitivity and specificity of 90.5 and 97.8%:
- Onset < 40 years affects young and middle -aged women (ages 15–45)
- Claudication of extremities
- Decreased pulsation of one or both brachial arteries
- At least 10 mmHg systolic difference in both arms
- Bruit over one or both carotid arteries or abdominal aorta
- Arteriographic narrowing of aorta, its primary branches, or large arteries in upper or lower extremities
- Ocular manifestation
- Visual loss or field defects
- Retinal hemorrhages
- Neurological abnormalities
- Treatment: steroids
Giant cell (temporal) arteritis. Chronic vasculitis of both large and medium vessels, primarily affecting cranial branches of the arteries arising from the aortic arch. At least three out of five criteria yields sensitivity and specificity of 95 and 91%:
- Age at onset ≥ 50 years
- New onset headache with localized tenderness
- Temporal artery tenderness or decreased pulsation
- Elevated ESR ≥ 50 mm/hour Westergren
- Temporal artery biopsy showing vasculitis with mononuclear cell infiltrate or granulomatous inflammation, usually with multinucleated giant cells
Medium vessel vasculitis
These conditions are sometimes considered together with the small vessel vasculitides.[11]
Polyarteritis nodosa (PAN). Systemic necrotizing vasculitis and aneurysm formation affecting both medium and small arteries. If only small vessels are affected, it is called microscopic polyangiitis, although it is more associated with granulomatosis with polyangiitis than to classic PAN. At least 3 out of 10 criteria yields sensitivity and specificity of 82 and 87%:
- Unexplained weight loss > 4 kg
- Livedo reticularis
- Testicular pain
- Myalgias, weakness
- Abdominal pain, diarrhea, and GI bleeding
- Mononeuropathy or polyneuropathy
- New onset diastolic blood pressure > 90 mmHg
- Elevated serum blood urea nitrogen (> 40 mg/dL) or serum creatinine (> 1.5 mg/dL)
- Hepatitis B infection
- Arteriographic abnormalities
- Arterial biopsy showing polymorphonuclear cells
Kawasaki disease. Usually in children (age<4), it affects large, medium, and small vessels, prominently the coronary arteries. Associated with a mucocutaneous lymph node syndrome. Diagnosis requires fever lasting five days or more with at least four out of five criteria:
- Bilateral conjunctival injection
- Injected or fissured lips, injected pharynx, or strawberry tongue
- Erythema of palms/soles, edema of hands/feet, periungual desquamation
- Polymorphous rash
- Cervical lymphadenopathy (at least one node > 1.5 cm)
Isolated cerebral vasculitis. Affects medium and small arteries over a diffuse CNS area, without symptomatic extracranial vessel involvement. Patients have CNS symptoms as well as cerebral vasculitis by angiography and leptomeningeal biopsy.
Small vessel vasculitis
There are several vasculitides that affect small vessels.[12]
Pauci-immune
Granulomatosis with polyangiitis. Systemic vasculitis of medium and small arteries, including venules and arterioles. Produces granulomatous inflammation of the respiratory tracts and necrotizing, pauci-immune glomerulonephritis. Most common cause of saddle nose deformity in USA (nose flattened due to destruction of nasal septum by granulomatous inflammation). Almost all patients with granulomatosis with polyangiitis have c-antineutrophil cytoplasmic antibody, but not vice versa. Current treatment of choice is cyclophosphamide. At least two out of four criteria yields sensitivity and specificity of 88 and 92%.
- Nasal or oral inflammation (oral ulcers or purulent/bloody nasal discharge, may be painful)
- Abnormal chest X-ray with showing nodules, infiltrates, or cavities
- Microscopic hematuria or red blood cell casts
- Vessel biopsy shows granulomatous inflammation
- Peak incidence: ages 40–60, males > females
Eosinophilic granulomatosis with polyangiitis (formerly known as Churg–Strauss syndrome). Affects medium and small vessels with vascular and extravascular granulomatosis. Classically involves arteries of lungs and skin, but may be generalized. At least four criteria yields sensitivity and specificity of 85 and 99.7%.
- Asthma (history of wheezing or presently wheezing)
- Eosinophilia > 10% on complete blood count
- Mononeuropathy or polyneuropathy
- Migratory or transient pulmonary opacities on chest x-ray
- Paranasal sinus abnormalities
- Vessel biopsy showing eosinophils in extravascular areas
Microscopic polyarteritis/polyangiitis. Affects capillaries, venules, or arterioles. Thought to be part of a group that includes granulomatosis with polyangiitis since both are associated with antineutrophil cytoplasmic antibody and similar extrapulmonary manifestations. Patients do not usually have symptomatic or histologic respiratory involvement.
Immune complex
Hypersensitivity vasculitis (allergic vasculitis). Usually due to a hypersensitivity reaction to a known drug. Drugs most commonly implicated are penicillin, sulphonamides and thiazide diuretics.[13] Methamphetamine and other sympathomimetics can cause a cerebral vasculitis alongside polyarteritis nodosa like systemic features. With other drugs,there is presence of skin vasculitis with palpable petechiae or purpura. Biopsy of these lesions reveal inflammation of the small vessels, termed leukocytoclastic vasculitis, which is most prominent in postcapillary venules. At least three out of five criteria yields sensitivity and specificity of 71 and 84%:
- Age > 16
- Use of possible triggering drug in relation to symptoms
- Palpable purpura
- Maculopapular rash
- Skin biopsy showing neutrophils around vessel
IgA vasculitis (formerly known as Henoch–Schonlein purpura). Systemic vasculitis due to tissue deposition of IgA-containing immune complexes. Biopsy of lesions shows inflammation of small vessels. It is considered a form of hypersensitivity vasculitis but is distinguished by prominent deposits of IgA. This is the most common vasculitis in children. Presence of three or more criteria yielded sensitivity of 87% while less than two criteria yielded hypersensitivity vasculitis in 74%:
- Palpable purpura (usually of buttocks and legs)
- Bowel angina
- GI bleed
- Hematuria
- Onset < 20 years
- No new medications
Essential cryoglobulinemic vasculitis. Most often due to hepatitis C infection, immune complexes of cryoglobulins – proteins that consists of immunoglobulins and complement and precipitate in the cold while dissolving upon rewarming – are deposited in walls of capillaries, venules, or arterioles. Therefore, complement will be low with histology showing vessel inflammation with immune deposits.
Other/ungrouped
Vasculitis secondary to connective tissue disorders. Usually secondary to systemic lupus erythematosus (SLE), rheumatoid arthritis (RA), relapsing polychondritis, Behçet's disease, and other connective tissue disorders.
Vasculitis secondary to viral infection. Usually due to hepatitis B and C, human immunodeficiency virus, cytomegalovirus, Epstein–Barr virus, and parvovirus B19.
Signs and symptoms
Patients usually present with systemic symptoms with single or multiorgan dysfunction. Common (and nonspecific) complaints include fatigue, weakness, fever, joint pains, abdominal pain, hypertension, chronic kidney disease, and neurologic dysfunction. The following symptoms should raise a strong suspicion of a vasculitis:
- Mononeuritis multiplex. Also known as asymmetric polyneuropathy, in a non-diabetic this is suggestive of vasculitis.
- Palpable purpura. If patients have this in isolation, it is most likely due to cutaneous leukocytoclastic vasculitis. If the purpura is in combination with systemic organ involvement, it is most likely to be Henoch–Schönlein purpura or microscopic polyangiitis.
- Pulmonary-renal syndrome. Individuals who are coughing up blood and have kidney involvement are likely to have granulomatosis with polyangiitis, microscopic polyangiitis, or anti-GBM disease (Goodpasture syndrome).
Diagnosis
A detailed history is important to elicit any recent medications, any risk of hepatitis infection, or any recent diagnosis with a connective tissue disorder such as systemic lupus erythematosus (SLE). A thorough physical exam is needed as usual.
- Lab tests. Basic lab tests may include a complete blood count, chemiestries (look for creatinine), creatine phosphokinase level, liver function tests, erythrocyte sedimentation rate, hepatitis serologies, urinalysis, chest X-ray, and an electrocardiogram. Additional, more specific tests include:
- Antinuclear antibody test can detect an underlying connective tissue disorder, especially lupus erythematosus
- Complement levels that are low can suggest mixed cryoglobulinemia, hepatitis C infection, and lupus erythematosus], but not most other vasculitides.
- Antineutrophil cytoplasmic antibody may suggest granulomatosis with polyangiitis, microscopic polyangiitis, eosinophilic granulomatosis with polyangiitis, or drug-induced vasculitis, but is not diagnostic.
- Electromyography. It is useful if a systemic vasculitis is suspected and neuromuscular symptoms are present.
- Arteriography. Arteriograms are helpful in vasculitis affecting the large and medium vessels but not helpful in small vessel vasculitis. Angiograms of mesenteric or renal arteries in polyarteritis nodosa may show aneurysms, occlusions, and vascular wall abnormalities. Arteriography are not diagnostic in itself if other accessible areas for biopsy are present. However, in Takayasu's arteritis, where the aorta may be involved, it is unlikely a biopsy will be successful and angiography can be diagnostic.
- Tissue biopsy. This is the gold standard of diagnosis when it is taken from the most involved area.
Treatment
Treatment is targeted to the underlying cause. However, most vasculitis in general are treated with steroids (e.g., methylprednisolone) because the underlying cause of the vasculitis is due to hyperactive immunological damage. Immunosuppressants such as cyclophosphamide and azathioprine may also be given.
A systematic review of antineutrophil cytoplasmic antibody-positive vasculitis identified best treatments depending on whether the goal is to induce remission or maintenance and depending on severity of the vasculitis.[14]
References
- ↑ Cruz BA, Ramanoelina J, Mahr A, et al. (October 2003). "Prognosis and outcome of 26 patients with systemic necrotizing vasculitis admitted to the intensive care unit". Rheumatology. 42 (10): 1183–8. doi:10.1093/rheumatology/keg322. PMID 12777637.
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran Pathologic Basis of Disease. St. Louis, Mo: Elsevier Saunders. p. 534. ISBN 978-0-7216-0187-8.
- ↑ "systemic necrotizing vasculitis" at Dorland's Medical Dictionary
- ↑ Généreau T, Lortholary O, Pottier MA, et al. (December 1999). "Temporal artery biopsy: a diagnostic tool for systemic necrotizing vasculitis. French Vasculitis Study Group". Arthritis Rheum. 42 (12): 2674–81. doi:10.1002/1529-0131(199912)42:12<2674::AID-ANR25>3.0.CO;2-A. PMID 10616017.
- ↑ Jennette JC, Falk RJ, Andrassy K, et al. (February 1994). "Nomenclature of systemic vasculitides. Proposal of an international consensus conference". Arthritis Rheum. 37 (2): 187–92. doi:10.1002/art.1780370206. PMID 8129773.
- ↑ Sørensen SF, Slot O, Tvede N, Petersen J (June 2000). "A prospective study of vasculitis patients collected in a five year period: evaluation of the Chapel Hill nomenclature". Ann. Rheum. Dis. 59 (6): 478–82. doi:10.1136/ard.59.6.478. PMC 1753166. PMID 10834866.
- ↑ Gonzalez-Gay MA, Garcia-Porrua C, Guerrero J, Rodriguez-Ledo P, Llorca J (June 2003). "The epidemiology of the primary systemic vasculitides in northwest Spain: implications of the Chapel Hill Consensus Conference definitions". Arthritis Rheum. 49 (3): 388–93. doi:10.1002/art.11115. PMID 12794795.
- ↑ Churg J (September 1993). "Large vessel vasculitis". Clin. Exp. Immunol. 93 Suppl 1 (Suppl 1): 11–2. doi:10.1111/j.1365-2249.1993.tb06216.x. PMC 1554929. PMID 8103424.
- ↑ Weyand CM, Goronzy JJ (July 2003). "Medium- and large-vessel vasculitis". New England Journal of Medicine. 349 (2): 160–9. doi:10.1056/NEJMra022694. PMID 12853590.
- ↑ Hoffman GS (September 2003). "Large-vessel vasculitis: unresolved issues". Arthritis Rheum. 48 (9): 2406–14. doi:10.1002/art.11243. PMID 13130459.
- ↑ Seo P, Stone JH (December 2007). "Small-vessel and medium-vessel vasculitis". Arthritis Rheum. 57 (8): 1552–9. doi:10.1002/art.23105. PMID 18050229.
- ↑ Jennette JC, Falk RJ (1997). "Small-vessel vasculitis". N. Engl. J. Med. 337 (21): 1512–23. doi:10.1056/NEJM199711203372106. PMID 9366584.
- ↑ Axford J, O'Callaghan C, (eds). 2004. Medicine. Oxford. Blackwell Publishing.
- ↑ Bosch X, Guilabert A, Espinosa G, Mirapeix E (2007). "Treatment of antineutrophil cytoplasmic antibody associated vasculitis: a systematic review". JAMA. 298 (6): 655–69. doi:10.1001/jama.298.6.655. PMID 17684188.
External links
| Classification | |
|---|---|
| External resources |