Superior cluneal nerves
| Superior cluneal nerves | |
|---|---|
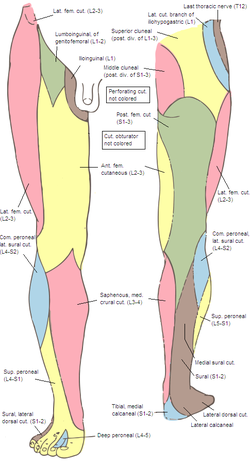 Cutaneous nerves of the right lower extremity. Front and posterior views. (Posterior division of lumbar visible in yellow at top right.) | |
| Details | |
| From | dorsal rami of L1-L3 nerve roots |
| Innervates | upper buttocks |
| Identifiers | |
| Latin | nervi clunium superiores |
| TA98 | A14.2.05.006 |
| TA2 | 6493 |
| FMA | 75468 |
| Anatomical terms of neuroanatomy | |
The superior cluneal nerves are pure sensory nerves that innervate the skin of the upper part of the buttocks. They are the terminal ends of the L1-L3 spinal nerve dorsal rami lateral branches. They are one of three different types of cluneal nerves (the middle and inferior cluneal nerves being the other two). They travel inferiorly through multiple layers of muscles, then traverse osteofibrous tunnels between the thoracolumbar fascia and iliac crest.[1]
Dysfunction of the superior cluneal nerves is often due to entrapment as the nerves cross the iliac crest – this can result in numbness, tingling or pain in the low back and upper buttocks region. Superior cluneal nerve dysfunction is a clinical diagnosis that can be supported by diagnostic nerve blocks.[1]
The superior cluneal nerves were first described by Maigne et al. in 1989 as a source of low back pain.[2]
Anatomy
Origin
These nerves are grouped as the superior cluneal nerves due to their trajectory over the iliac spine, as opposed to the lateral, medial and inferior cluneal nerves. These nerves most commonly originate from the dorsal rami of the L1, L2, and L3 nerve roots. In cadaver studies, a small percentage of patients will also have origins at the L4 and L5 nerve roots.[3][4]
Course and relations
After they branch off the dorsal rami, they pass through the erector spinae muscle, psoas major, paraspinal muscles, and then inferior latissimus dorsi to reach the iliac crest.[5]
The nerves then pass through an osteofibrous tunnel created by the thoracolumbar fascia and rim of the superior iliac crest.[6] Cadaver studies have noted that some patients have boney grooves along the rim that house the superior cluneal nerves. On average, these grooves are found between 5–7 cm from the midline.[7][8] These grooves can often be visualized with an ultrasound.[8]
The nerves terminate over the gluteal fascia distal to the iliac crest.[citation needed]
Clinical significance
Damage to the cluneal nerves can be from direct injury or from entrapment between the muscles or in the osteofibrous tunnel. Direct injury to the cluneal nerves can happen during posterior iliac crest harvest to obtain bone mineral for other surgeries, such as spinal arthrodesis.[9][10] Entrapment of the nerve can occur at any point but is most common across the osteofibrous tunnel.[citation needed]
Superior cluneal nerve dysfunction
Dysfunction of the superior cluneal nerves lead to many different neuropathic symptoms such as burning pain, numbness, tingling, and dysesthesia around the low back and upper gluteal area. The most common symptoms are localized unilateral low back pain, though up to anywhere between 40 and 82% of patients may complain of leg symptoms – pain or dysethesia.[5][11][12] The onset of pain can vary, with some patients report sudden onset of pain with a known inciting incident.[13] These symptoms can be exacerbated by lumbar flexion, extension, and rotation.[1] Manual compression over the posterior superior iliac crest, such as with wearing tight clothing and belts, can also reproduce symptoms.[1][5] Many patients also have tender points located around the posterior iliac crest, approximately 7 cm from midline which correlates with cadaver studies demonstrating the location at which the nerves cross the iliac crest.[5][14] On physical exam, the pain can be reproduced by the excessive motions listed above or by tapping along the posterior superior iliac crest, which would be a positive Tinel-like sign.[5][14] In the setting of nerve entrapment between the muscles, activation of the muscles with lumbar extension can reproduce the pain.[5] Besides pain, patients can also have reduced sensation to light touch over the nerve distribution.[1][5][14]
Diagnosis of superior cluneal nerve dysfunction requires the help of a skilled clinician as it requires a good history and physical examination. Imaging, such as magnetic resonance imaging, can be used to rule out other pathologies. In many cases, this diagnosis is made after treatment of more common pathologies with similar symptoms. The most common overlapping pathologies include facet joint pain, sacroiliac joint dysfunction, and lumbosacral radiculopathy. Electrodiagnostic studies, including electromyography and nerve conduction studies, can also help rule out other pathologies.[1] Currently, there is no consistent protocol for testing the superior cluneal nerves with a nerve conduction study. Diagnosis of superior cluneal nerve entrapment can be aided by diagnostic blocks of the nerve across the iliac crest.[1][5]
Treatment
The treatment for superior cluneal nerve dysfunction can vary based on the clinician and severity of symptoms. There is currently limited evidence for treatment at this time. Physical therapy can be initiated to improve strength and flexibility. The addition of non-steroidal anti-inflammatory medications can help with overall discomfort but has not been shown to have direct effects of the nerve. Specifically, the use of COX-2 inhibitors is a reasonable first step.[1] Other treatments of superior cluneal nerve dysfunction include both minimally invasive interventions and surgical options. Minimally invasive treatments include nerve blocks, neuroablation, and neuromodulation.[5] Efficacy of these interventions are still being studied and no clear evidence to show long term benefits in larger studies. Minimally invasive treatments can be performed with ultrasound or fluoroscopy to improve safety and accuracy.
Nerve blocks are injections that target specific nerves to serve as both therapeutic and diagnostic purposes. They have been used for a variety of neuropathic conditions including facet joint pain. Nerve block injections specifically targeted at the superior cluneal nerves are limited.[5] However, these blocks are minimally invasive and involve injecting medications at the nerves as they cross the iliac crest.[11] These blocks can be done with local anesthetics with or without corticosteroids.[1][5][11] Improvement in pain after these blocks suggest that these nerves are the source of the patient's symptoms, however these blocks are often temporary and studies regarding corticosteroid reported 68% of patients had improved back pain after 1-3 repetitive blocks.[11] These injections can be performed with or without image modalities, though the use of ultrasound guidance may help optimize medication delivery [11][8][15] These procedures can also be done under fluoroscopy.
Neuroablation can be performed with chemical neurolysis or radiofrequency ablation. These techniques are often used on the medial branch nerves to treat low back pain and have been applied to the superior cluneal nerves. The use of phenol has been noted to relieve pain for up to 9 months but may not completely resolve symptoms.[5]
Neuromodulation of the cluneal nerve with peripheral nerve stimulation has not been widely established as an effective treatment, though there are some studies that show significant benefits.[5][16]
Surgical intervention typically involves decompression of the nerves from the osteofibrous tunnels. Few studies have shown long term benefits of surgical intervention.[17][18]
Additional images
-
Diagram of the distribution of the cutaneous branches of the posterior divisions of the spinal nerves.
-
Areas of distribution of the cutaneous branches of the posterior divisions of the spinal nerves.
References
- ^ a b c d e f g h i Waldman SD. Atlas of Uncommon Pain Syndromes. 3rd ed. Philadelphia, PA: Saunders/Elsevier; 2014.
- ^ Maigne, J. Y.; Lazareth, J. P.; Surville, H. Guérin; Maigne, R. (1989). "The lateral cutaneous branches of the dorsal rami of the thoraco-lumbar junction". Surgical and Radiologic Anatomy. 11 (4): 289–293. doi:10.1007/BF02098698. PMID 2533408. S2CID 39158958.
- ^ Iwanaga, Joe; Simonds, Emily; Schumacher, Maia; Oskouian, Rod J.; Tubbs, R. Shane (2019). "Anatomic Study of Superior Cluneal Nerves: Revisiting the Contribution of Lumbar Spinal Nerves". World Neurosurgery. 128: e12–e15. doi:10.1016/j.wneu.2019.02.159. PMID 30862587. S2CID 76663848.
- ^ Konno, Tomoyuki; Aota, Yoichi; Kuniya, Hiroshi; Saito, Tomoyuki; Qu, Ning; Hayashi, Shogo; Kawata, Shinichi; Itoh, Masahiro (2017). "Anatomical etiology of "pseudo-sciatica" from superior cluneal nerve entrapment: A laboratory investigation". Journal of Pain Research. 10: 2539–2545. doi:10.2147/jpr.s142115. PMC 5677392. PMID 29138591.
- ^ a b c d e f g h i j k l m Karri, Jay; Singh, Mani; Orhurhu, Vwaire; Joshi, Mihir; Abd-Elsayed, Alaa (2020). "Pain Syndromes Secondary to Cluneal Nerve Entrapment". Current Pain and Headache Reports. 24 (10): 61. doi:10.1007/s11916-020-00891-7. PMID 32821979. S2CID 221199448.
- ^ Lu, J.; Ebraheim, N. A.; Huntoon, M.; Heck, B. E.; Yeasting, R. A. (1998). "Anatomic considerations of superior cluneal nerve at posterior iliac crest region". Clinical Orthopaedics and Related Research (347): 224–228. PMID 9520894.
- ^ Iwanaga, Joe; Simonds, Emily; Schumacher, Maia; Yilmaz, Emre; Altafulla, Juan; Tubbs, R. Shane (2019). "Anatomic Study of the Superior Cluneal Nerve and Its Related Groove on the Iliac Crest". World Neurosurgery. 125: e925–e928. doi:10.1016/j.wneu.2019.01.210. PMID 30763748. S2CID 73430020.
- ^ a b c Fan, Kun; Cheng, Chen; Gong, Wen-Yi (2021). "A simple and novel ultrasound-guided approach for superior cluneal nerves block". Anaesthesia Critical Care & Pain Medicine. 40 (2): 100838. doi:10.1016/j.accpm.2021.100838. PMID 33757913. S2CID 232337450.
- ^ Ebraheim, Nabil A.; Elgafy, Hossein; Xu, Rongming (2001). "Bone-Graft Harvesting from Iliac and Fibular Donor Sites: Techniques and Complications". Journal of the American Academy of Orthopaedic Surgeons. 9 (3): 210–218. doi:10.5435/00124635-200105000-00007. PMID 11421578. S2CID 24103745.
- ^ Tubbs, R. Shane; Levin, Matthew R.; Loukas, Marios; Potts, Eric A.; Cohen-Gadol, Aaron A. (2010). "Anatomy and landmarks for the superior and middle cluneal nerves: Application to posterior iliac crest harvest and entrapment syndromes". Journal of Neurosurgery: Spine. 13 (3): 356–359. doi:10.3171/2010.3.spine09747. PMID 20809730.
- ^ a b c d e Kuniya, Hiroshi; Aota, Yoichi; Kawai, Takuya; Kaneko, Kan-Ichiro; Konno, Tomoyuki; Saito, Tomoyuki (2014). "Prospective study of superior cluneal nerve disorder as a potential cause of low back pain and leg symptoms". Journal of Orthopaedic Surgery and Research. 9: 139. doi:10.1186/s13018-014-0139-7. PMC 4299373. PMID 25551470.
- ^ Miki, Koichi; Kim, Kyongsong; Isu, Toyohiko; Matsumoto, Juntaro; Kokubo, Rinko; Isobe, Masanori; Inoue, Tooru (2019). "Characteristics of Low Back Pain due to Superior Cluneal Nerve Entrapment Neuropathy". Asian Spine Journal. 13 (5): 772–778. doi:10.31616/asj.2018.0324. PMC 6773996. PMID 31079427.
- ^ Kim, Kyongsong; Isu, Toyohiko; Chiba, Yasuhiro; Iwamoto, Naotaka; Yamazaki, Kazuyoshi; Morimoto, Daijiro; Isobe, Masanori; Inoue, Kiyoharu (2015). "Treatment of low back pain in patients with vertebral compression fractures and superior cluneal nerve entrapment neuropathies". Surgical Neurology International. 6 (25): S619-21. doi:10.4103/2152-7806.170455. PMC 4671138. PMID 26693392.
- ^ a b c Isu, Toyohiko; Kim, Kyongsong; Morimoto, Daijiro; Iwamoto, Naotaka (2018). "Superior and Middle Cluneal Nerve Entrapment as a Cause of Low Back Pain". Neurospine. 15 (1): 25–32. doi:10.14245/ns.1836024.012. PMC 5944640. PMID 29656623. S2CID 4899042.
- ^ Nielsen, Thomas Dahl; Moriggl, Bernhard; Barckman, Jeppe; Jensen, Jan Mick; Kolsen-Petersen, Jens Aage; Søballe, Kjeld; Børglum, Jens; Bendtsen, Thomas Fichtner (2019). "Randomized trial of ultrasound-guided superior cluneal nerve block". Regional Anesthesia & Pain Medicine. 44 (8): 772–780. doi:10.1136/rapm-2018-100174. PMID 31061111. S2CID 146810542.
- ^ Deer, Timothy; Pope, Jason; Benyamin, Ramsin; Vallejo, Ricardo; Friedman, Andrew; Caraway, David; Staats, Peter; Grigsby, Eric; Porter Mcroberts, W.; McJunkin, Tory; Shubin, Richard; Vahedifar, Payam; Tavanaiepour, Daryoush; Levy, Robert; Kapural, Leonardo; Mekhail, Nagy (2016). "Prospective, Multicenter, Randomized, Double-Blinded, Partial Crossover Study to Assess the Safety and Efficacy of the Novel Neuromodulation System in the Treatment of Patients with Chronic Pain of Peripheral Nerve Origin". Neuromodulation: Technology at the Neural Interface. 19 (1): 91–100. doi:10.1111/ner.12381. PMID 26799373. S2CID 23413856.
- ^ Maigne, Jean-Yves; Doursounian, Levon (1997). "Entrapment Neuropathy of the Medial Superior Cluneal Nerve". Spine. 22 (10): 1156–1159. doi:10.1097/00007632-199705150-00017. PMID 9160476. S2CID 40323409.
- ^ Morimoto, Daijiro; Isu, Toyohiko; Kim, Kyongsong; Chiba, Yasuhiro; Iwamoto, Naotaka; Isobe, Masanori; Morita, Akio (2017). "Long-term Outcome of Surgical Treatment for Superior Cluneal Nerve Entrapment Neuropathy". Spine. 42 (10): 783–788. doi:10.1097/brs.0000000000001913. PMID 27669049. S2CID 4383288.
External links
- glutealregion at The Anatomy Lesson by Wesley Norman (Georgetown University)
- Anatomy photo:11:07-0102 at the SUNY Downstate Medical Center - "Superficial Anatomy of the Lower Extremity: Cutaneous Nerves of the Posterior Aspect of the Lower Extremity"
