Stewart–Treves syndrome
Stewart–Treves syndrome, refers to a lymphangiosarcoma, a rare complication that forms as a result of chronic, long-standing lymphedema. Although it most commonly refers to malignancies associated with chronic lymphedema resulting from mastectomy and/or radiotherapy for breast cancer,[1] it may also describe lymphangiosarcomas that result from congenital and other causes of chronic secondary lymphedema.[2] Lymphangiosarcoma arising from cancer-related lymphedema has become much less common with better surgical techniques, radiation therapy, and conservative treatment.[3] The prognosis, even with wide surgical excision and subsequent radiotherapy, is poor.[4]
Symptoms and signs
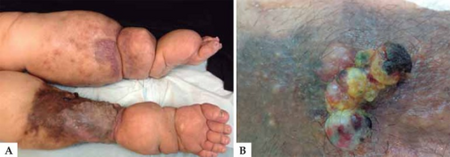
Among the clinical presentation for this condition, Stewart–Treves syndrome , are: purplish patch that becomes a skin nodule, mass under the skin, and non- healing eschar with recurrent bleeding.[5]
Cause
The cause of this condition is not known, however there seems to be an association with cases of lymphedema.[5]
Diagnosis
The diagnosis for this condition is based on the following:[5]
- Clinical presentation
- Imaging studies
- Skin biopsy
- Special blood test
Treatment
The treatment of choice is a large resection or amputation of the affected limb. Radiation therapy can precede or follow surgical treatment. Tumors that have advanced locally or have metastasized can be treated with mono or polychemotherapy, systemically or locally.[6] However, chemotherapy and radiation therapy have not been shown to improve survivorship significantly.[2] In cases of upper limbs, forequarter amputation (disarticulation of upperlimb along with clavicle and scapula) is preferred.
Prognosis
Early detection is key. Untreated patients usually live 5 to 8 months after diagnosis.[2]
Incidence
In the 1960s, the incidence 5 years after a radical mastectomy varied from 0.07% to 0.45%.[7] Today, it occurs in 0.03% of patients surviving 10 or more years after radical mastectomy.[6]
History
It was discovered by Fred W. Stewart and Norman Treves in 1948.
See also
- Lymphangiosarcoma
- Angiosarcoma
- Mastectomy
- Postcardiotomy syndrome
- List of cutaneous conditions
- Lymphedema
References
- ↑ James, William D.; Berger, Timothy G.; et al. (2006). Andrews' Diseases of the Skin: clinical Dermatology. Saunders Elsevier. ISBN 978-0-7216-2921-6.
- ↑ 2.0 2.1 2.2 Sharma, A; Schwartz, RA (June 2012). "Stewart-Treves syndrome: Pathogenesis and management". J Am Acad Dermatol. 67 (6): 1342–8. doi:10.1016/j.jaad.2012.04.028. PMID 22682884.
- ↑ Kumar MBBS MD FRCPath, Vinay (2010). Robins and Cotran: Pathologic Basis of Disease 8th Edition. Philadelphia, PA: Saunders Elsevier. p. 1093. ISBN 978-1-4160-3121-5.
- ↑ Pincus LB, Fox LP (August 2008). "Images in clinical medicine. The Stewart-Treves syndrome". N. Engl. J. Med. 359 (9): 950. doi:10.1056/NEJMicm071344. PMID 18753651.
- ↑ 5.0 5.1 5.2 "Stewart Treves syndrome | Genetic and Rare Diseases Information Center (GARD) – an NCATS Program". rarediseases.info.nih.gov. Archived from the original on 18 March 2021. Retrieved 10 September 2021.
- ↑ 6.0 6.1 Wierzbicka-Hainaut, E; Guillet, G (December 2010). "[Stewart-Treves syndrome (angiosarcoma on lyphoedema): A rare complication of lymphoedema]". Presse Méd. 39 (12): 1305–8. doi:10.1016/j.lpm.2010.06.017. PMID 20970956.
- ↑ Heitmann, C; Ingianni, G (January 2000). "Stewart-Treves syndrome: lymphangiosarcoma following mastectomy". Ann Plast Surg. 44 (1): 72–5. doi:10.1097/00000637-200044010-00012. PMID 10651369.
External links
| External resources |
|---|