Spinal stenosis
| Spinal stenosis | |
|---|---|
 | |
| Spinal stenosis | |
| Specialty | Orthopedics, neurosurgery |
| Symptoms | Pain, numbness, or weakness in the arms or legs[1] |
| Complications | Loss of bladder control, loss of bowel control, sexual dysfunction[1] |
| Usual onset | Gradual[1] |
| Types | Cervical, thoracic, lumbar[2] |
| Causes | Osteoarthritis, rheumatoid arthritis, spinal tumors, trauma, Paget's disease of the bone, scoliosis, spondylolisthesis, achondroplasia[3] |
| Diagnostic method | Based on symptoms and medical imaging[4] |
| Differential diagnosis | Cauda equina syndrome, osteomylitis, peripheral vascular disease, fibromyalgia[5] |
| Treatment | Medications, exercises, bracing, surgery.[6] |
| Medication | NSAIDs, acetaminophen, steroid injections[7] |
| Frequency | Up to 8% of people[4] |
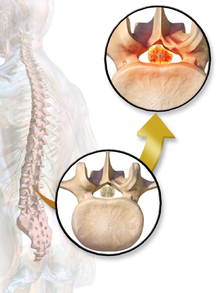
Spinal stenosis is an abnormal narrowing of the spinal canal or neural foramen that results in pressure on the spinal cord or nerve roots.[6] Symptoms may include pain, numbness, or weakness in the arms or legs.[1] Symptoms are typically gradual in onset and improve with bending forwards.[1] Severe symptoms may include loss of bladder control, loss of bowel control, or sexual dysfunction.[1]
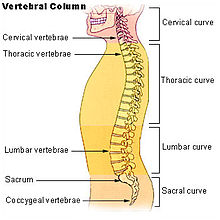
Causes may include osteoarthritis, rheumatoid arthritis, spinal tumors, trauma, Paget's disease of the bone, scoliosis, spondylolisthesis, and the genetic condition achondroplasia.[3] It can be classified by the part of the spine affected into cervical, thoracic, and lumbar stenosis.[2] Lumbar stenosis is the most common, followed by cervical stenosis.[2] Diagnosis is generally based on symptoms and medical imaging.[4]
Treatment may involve medications, bracing, or surgery.[6] Medications may include NSAIDs, acetaminophen, or steroid injections.[7] Stretching and strengthening exercises may also be useful.[1] Limiting certain activities may be recommended.[6] Surgery is typically only done if other treatments are not effective, with the usual procedure being a decompressive laminectomy.[7]
Spinal stenosis occurs in as many as 8% of people.[4] It occurs most commonly in people over the age of 50.[8] Males and females are affected equally often.[9] The first modern description of the condition is from 1803 by Antoine Portal, and there is evidence of the condition dating back to Ancient Egypt.[10]
Types
The most common forms are cervical spinal stenosis, which are at the level of the neck, and lumbar spinal stenosis, at the level of the lower back. Thoracic spinal stenosis, at the level of the mid-back, is much less common.[11]
In lumbar stenosis, the spinal nerve roots in the lower back are compressed which can lead to symptoms of sciatica (tingling, weakness, or numbness that radiates from the low back and into the buttocks and legs).
Cervical spinal stenosis can be far more dangerous by compressing the spinal cord. Cervical canal stenosis may lead to myelopathy, a serious condition causing symptoms including major body weakness and paralysis.[12] Such severe spinal stenosis symptoms are virtually absent in lumbar stenosis, however, as the spinal cord terminates at the top end of the adult lumbar spine, with only nerve roots (cauda equina) continuing further down.[13] Cervical spinal stenosis is a condition involving narrowing of the spinal canal at the level of the neck. It is frequently due to chronic degeneration,[14] but may also be congenital or traumatic. Treatment frequently is surgical.[14]
Signs and symptoms
Common
- Standing discomfort (94%)
- Discomfort/pain, in shoulder, arm, hand (78%)
- Bilateral symptoms (68%)
- Numbness at or below the level of involvement (63%)
- Weakness at or below the level of involvement (43%)
- Pain or weakness in buttock / thigh only (8%)
- Pain or weakness below the knee (3%)[15]
Neurological disorders
- Cervical (spondylotic) myelopathy,[16] a syndrome caused by compression of the cervical spinal cord which is associated with "numb and clumsy hands", imbalance, loss of bladder and bowel control, and weakness that can progress to paralysis.
- Pinched nerve,[17] causing numbness.
- Intermittent neurogenic claudication[15][18][19] characterized by lower limb numbness, weakness, diffuse or radicular leg pain associated with paresthesia (bilaterally),[18] weakness and/or heaviness in buttocks radiating into lower extremities with walking or prolonged standing.[15] Symptoms occur with extension of spine and are relieved with spine flexion. Minimal to zero symptoms when seated or supine.[15]
- Radiculopathy (with or without radicular pain)[18] neurologic condition—nerve root dysfunction causes objective signs such as weakness, loss of sensation and of reflex.
- Cauda equina syndrome[20] - Lower extremity pain, weakness, numbness that may involve perineum and buttocks, associated with bladder and bowel dysfunction.
- Lower back pain[15][19] due to degenerative disc or joint changes.[21]
Causes
Aging
Any of the factors below may cause the spaces in the spine to narrow.
- Spinal ligaments can thicken (ligamenta flava)[22][23]
- Bone spurs develop on the bone and into the spinal canal or foraminal openings
- Intervertebral discs may bulge or herniate into the canal or foraminal openings[24]
- Degenerative disc disease causes narrowing of the spaces [25]
- Facet joints break down
- Facet joints may hypertrophy[26]
- Compression fractures of the spine, which are common in osteoporosis[27]
- Cysts form on the facet joints causing compression of the spinal sac of nerves (thecal sac)
Arthritis
- Osteoarthritis
- Rheumatoid arthritis—much less common cause of spinal problems
Congenital
- Spinal canal is too small at birth
- Structural deformities of the vertebrae may cause narrowing of the spinal canal
Instability of the spine
- A vertebra slips forward on another (spondylolisthesis)
Trauma
- Accidents and injuries may dislocate the spine and the spinal canal or cause burst fractures that yield fragments of bone that go through the canal.[28]
- Patients with cervical myelopathy caused by narrowing of the spinal canal are at higher risks of acute spinal cord injury if involved in accidents.[29]
Tumors
- Irregular growths of soft tissue will cause inflammation.
- Growth of tissue into the canal pressing on nerves, the sac of nerves, or the spinal cord.
Diagnosis

The diagnosis of spinal stenosis involves a complete evaluation of the spine. The process usually begins with a medical history and physical examination. X-ray and MRI scans are typically used to determine the extent and location of the nerve compression.
Medical history
The medical history is the most important aspect of the examination as it will tell the physician about subjective symptoms, possible causes for spinal stenosis, and other possible causes of back pain.[30]
Physical examination
The physical examination of a patient with spinal stenosis will give the physician information about exactly where nerve compression is occurring. Some important factors that should be investigated are any areas of sensory abnormalities, numbness, irregular reflexes, and any muscular weakness.[30]
MRI
MRI has become the most frequently used study to diagnose spinal stenosis. The MRI uses electromagnetic signals to produce images of the spine. MRIs are helpful because they show more structures, including nerves, muscles, and ligaments, than seen on X-rays or CT scans. MRIs are helpful at showing exactly what is causing spinal nerve compression.
CT myelogram
A spinal tap is performed in the low back with dye injected into the spinal fluid. X-Rays are performed followed by a CT scan of the spine to help see narrowing of the spinal canal. This is a very effective study in cases of lateral recess stenosis. It is also necessary for patients in which MRI is contraindicated, such as those with implanted pacemakers.
Red flags
- Fever
- Nocturnal pain
- Gait disturbance
- Structural deformity
- Unexplained weight loss
- Previous carcinoma
- Severe pain upon lying down
- Recent trauma with suspicious fracture
- Presence of severe or progressive neurologic deficit[20]
Treatments
Treatment options are either surgical or non-surgical. Overall evidence is inconclusive whether non-surgical or surgical treatment is the better for lumbar spinal stenosis.[31]
Non-surgical treatments
The effectiveness of non surgical treatments is unclear as they have not been well studied.[32]
- Education about the course of the condition and how to relieve symptoms
- Medicines to relieve pain and inflammation, such as acetaminophen, nonsteroidal anti-inflammatory drugs (NSAIDs)
- Exercise, to maintain or achieve overall good health, aerobic exercise, such as riding a stationary bicycle, which allows for a forward lean, walking, or swimming can relieve symptoms
- Weight loss, to relieve symptoms and slow progression of the stenosis
- Physical therapy to support self-care.[33] Also may give instructs on stretching and strength exercises that may lead to a decrease in pain and other symptoms.
- Lumbar epidural steroid or anesthetic injections have low quality evidence to support their use.[32][34]
Surgery
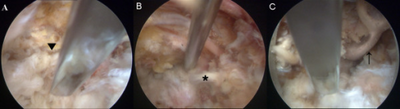
Lumbar decompressive laminectomy: This involves removing the roof of bone overlying the spinal canal and thickened ligaments in order to decompress the nerves and sac of nerves. 70-90% of people have good results.[35]
- Interlaminar implant: This is a non-fusion U-shaped device which is placed between two bones in the lower back that maintains motion in the spine and keeps the spine stable after a lumbar decompressive surgery. The U-shaped device maintains height between the bones in the spine so nerves can exit freely and extend to lower extremities.[36]
- Surgery for cervical myelopathy is either conducted from the front or from the back, depending on several factors such as where the compression occurs and how the cervical spine is aligned.
- Anterior cervical discectomy and fusion: A surgical treatment of nerve root or spinal cord compression by decompressing the spinal cord and nerve roots of the cervical spine with a discectomy in order to stabilize the corresponding vertebrae.
- Posterior approaches seek to generate space around the spinal cord by removing parts of the posterior elements of the spine. Techniques include laminectomy, laminectomy and fusion, and laminoplasty.
Decompression plus fusion appears no better than decompression alone, while spinal spacers appears better than decompression plus fusion but not better than decompression alone.[37] No differences were found in the type of decompression.[37]
Epidemiology
- The NAMCS data shows the incidence in the U.S. population to be 3.9% of 29,964,894 visits for mechanical back problems.[38]
- The Longitudinal Framingham Heart Study found 1% of men and 1.5% of women had vertebral slippage at mean age of 54. Over the next 25 years, 11% of men and 25% of women developed degenerative vertebral slippage.[39]
Research
A RCT is being conducted in Sweden, to compare surgery versus non-surgical treatment for lumbar spinal stenosis.[40]
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 "Spinal Stenosis". National Institute of Arthritis and Musculoskeletal and Skin Diseases. 11 April 2017. Archived from the original on 20 March 2021. Retrieved 19 December 2017.
- ↑ 2.0 2.1 2.2 Canale, S. Terry; Beaty, James H. (2012). Campbell's Operative Orthopaedics E-Book. Elsevier Health Sciences. p. 1994. ISBN 978-0323087186. Archived from the original on 2019-09-01. Retrieved 2017-12-19.
- ↑ 3.0 3.1 "Spinal Stenosis". National Institute of Arthritis and Musculoskeletal and Skin Diseases. 11 April 2017. Archived from the original on 20 March 2021. Retrieved 19 December 2017.
- ↑ 4.0 4.1 4.2 4.3 Domino, Frank J. (2010). The 5-Minute Clinical Consult 2011. Lippincott Williams & Wilkins. p. 1224. ISBN 9781608312597. Archived from the original on 2019-09-03. Retrieved 2017-12-19.
- ↑ Ferri, Fred F. (2017). Ferri's Clinical Advisor 2018 E-Book: 5 Books in 1. Elsevier Health Sciences. p. 1202. ISBN 9780323529570. Archived from the original on 2019-09-05. Retrieved 2017-12-19.
- ↑ 6.0 6.1 6.2 6.3 "Spinal Stenosis". National Institute of Arthritis and Musculoskeletal and Skin Diseases. 11 April 2017. Archived from the original on 20 March 2021. Retrieved 19 December 2017.
- ↑ 7.0 7.1 7.2 "Spinal Stenosis". National Institute of Arthritis and Musculoskeletal and Skin Diseases. 11 April 2017. Archived from the original on 20 March 2021. Retrieved 19 December 2017.
- ↑ "Spinal Stenosis". National Institute of Arthritis and Musculoskeletal and Skin Diseases. 11 April 2017. Archived from the original on 20 March 2021. Retrieved 19 December 2017.
- ↑ "Lumbar Spinal Stenosis". OrthoInfo - AAOS. December 2013. Archived from the original on 26 January 2021. Retrieved 19 December 2017.
- ↑ Boos, Norbert; Aebi, Max (2008). Spinal Disorders: Fundamentals of Diagnosis and Treatment. Springer Science & Business Media. pp. 21–22. ISBN 9783540690917. Archived from the original on 2019-09-05. Retrieved 2017-12-19.
- ↑ Vokshoor A (February 14, 2010). "Spinal Stenosis". eMedicine. Archived from the original on December 30, 2010. Retrieved December 30, 2010.
- ↑ "CSM Symptoms". Myelopathy.org. Archived from the original on 2015-11-18. Retrieved 2015-11-23.
- ↑ Waxman, SG (2000). Correlative Neuroanatomy (24th ed.).
- ↑ 14.0 14.1 Meyer F, Börm W, Thomé C (May 2008). "Degenerative cervical spinal stenosis: current strategies in diagnosis and treatment". Deutsches Ärzteblatt International. 105 (20): 366–72. doi:10.3238/arztebl.2008.0366. PMC 2696878. PMID 19626174.
- ↑ 15.0 15.1 15.2 15.3 15.4 Mazanec DJ, Podichetty VK, Hsia A (November 2002). "Lumbar canal stenosis: start with nonsurgical therapy". Cleveland Clinic Journal of Medicine. 69 (11): 909–17. doi:10.3949/ccjm.69.11.909. PMID 12430977. Archived from the original on 2021-08-29. Retrieved 2019-11-30.
- ↑ "What is CSM?". Myelopathy.org. Archived from the original on 2015-11-18. Retrieved 2015-11-23.
- ↑ "Cervical Radiculopathy (Pinched Nerve)". AAOS. Archived from the original on 3 November 2017. Retrieved 13 December 2011.
- ↑ 18.0 18.1 18.2 Costantini A, Buchser E, Van Buyten JP (October 2010). "Spinal cord stimulation for the treatment of chronic pain in patients with lumbar spinal stenosis". Neuromodulation. 13 (4): 275–9, discussion 279–80. doi:10.1111/j.1525-1403.2010.00289.x. PMID 21992882.
- ↑ 19.0 19.1 Goren A, Yildiz N, Topuz O, Findikoglu G, Ardic F (July 2010). "Efficacy of exercise and ultrasound in patients with lumbar spinal stenosis: a prospective randomized controlled trial". Clinical Rehabilitation. 24 (7): 623–31. doi:10.1177/0269215510367539. PMID 20530650. Archived from the original on 2021-08-29. Retrieved 2020-02-01.
- ↑ 20.0 20.1 Doorly, T. P., Lambing, C. L., Malanga, G. A., Maurer, P. M., Ralph R., R. (2010). Algorithmic approach to the management of the patient with lumbar spinal stenosis. Journal of Family Practice, 59 S1-S8
- ↑ Mazanec, D. J., Podichetty, V. K., Hsia, A. (2002) Lumbar Clinic Journal of Medicine 69 (11).
- ↑ Park JB, Lee JK, Park SJ, Riew KD, "Hypertrophy of ligamentum flavum in lumbar spinal stenosis associated with increased proteinase inhibitor concentration," Archived 2019-02-07 at the Wayback Machine J Bone Joint Surg Am. 2005 Dec;87(12):2750-7.
- ↑ ligamentum flavum Archived 2017-06-29 at the Wayback Machine, Physio-Pedia.com
- ↑ "Herniated Disk," Archived 2017-07-18 at the Wayback Machine Mayo-Clinic.org
- ↑ "Degenerative Disk Disease," Archived 2017-07-12 at the Wayback Machine Mayfieldclinic.com
- ↑ Lim, Andy; D’Urso, Paul (October 2009). "Single-level bilateral facet joint hypertrophy causing thoracic spinal canal stenosis". Journal of Clinical Neuroscience. 16 (10): 1363–1365. doi:10.1016/j.jocn.2008.10.023. ISSN 0967-5868. Archived from the original on 2021-08-29. Retrieved 2020-05-12.
- ↑ "Causes of Spinal Compression Fractures," Archived 2017-06-26 at the Wayback Machine, WebMD
- ↑ "Spinal stenosis Causes". Mayo Clinic. 2012-06-28. Archived from the original on 2013-06-18. Retrieved 2015-04-17.
- ↑ Wu JC, Ko CC, Yen YS, Huang WC, Chen YC, Liu L, et al. (July 2013). "Epidemiology of cervical spondylotic myelopathy and its risk of causing spinal cord injury: a national cohort study". Neurosurgical Focus. 35 (1): E10. doi:10.3171/2013.4.FOCUS13122. PMID 23815246.
- ↑ 30.0 30.1 Cluett, Jonathan, M.D. (2010) Spinal Stenosis - How is Spinal Stenosis Diagnosed? Archived 2012-01-29 at the Wayback Machine
- ↑ Zaina F, Tomkins-Lane C, Carragee E, Negrini S (January 2016). "Surgical versus non-surgical treatment for lumbar spinal stenosis". The Cochrane Database of Systematic Reviews. 1 (1): CD010264. doi:10.1002/14651858.CD010264.pub2. PMC 6669253. PMID 26824399.
- ↑ 32.0 32.1 Ammendolia C, Stuber KJ, Rok E, Rampersaud R, Kennedy CA, Pennick V, et al. (August 2013). "Nonoperative treatment for lumbar spinal stenosis with neurogenic claudication". The Cochrane Database of Systematic Reviews. 8 (8): CD010712. doi:10.1002/14651858.CD010712. PMID 23996271. Archived from the original on 2021-08-29. Retrieved 2019-11-30.
- ↑ "Lumbar Spinal Stenosis-Treatment Overview". WebMD. Archived from the original on 2017-07-07. Retrieved 2015-04-17.
- ↑ Chou R, Hashimoto R, Friedly J, Fu R, Bougatsos C, Dana T, et al. (September 2015). "Epidural Corticosteroid Injections for Radiculopathy and Spinal Stenosis: A Systematic Review and Meta-analysis". Annals of Internal Medicine. 163 (5): 373–81. doi:10.7326/M15-0934. PMID 26302454. Archived from the original on 2021-08-29. Retrieved 2020-02-01.
- ↑ Malamut, edited by Joseph I. Sirven, Barbara L. (2008). Clinical neurology of the older adult (2nd ed.). Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. p. 220. ISBN 9780781769471. Archived from the original on 2021-08-29. Retrieved 2017-09-14.
- ↑ "coflex Interlaminar Technology - P110008". FDA. 2014-01-17. Archived from the original on 2015-04-17. Retrieved 2015-04-17.
- ↑ 37.0 37.1 Machado GC, Ferreira PH, Yoo RI, Harris IA, Pinheiro MB, Koes BW, et al. (November 2016). "Surgical options for lumbar spinal stenosis". The Cochrane Database of Systematic Reviews. 11: CD012421. doi:10.1002/14651858.cd012421. PMC 6464992. PMID 27801521.
- ↑ "Spinal Stenosis Details". Spinalstenosis.org. Archived from the original on 2015-04-23. Retrieved 2015-04-17.
- ↑ Treatment of Degenerative Lumbar Spinal Stenosis, Evidence Report/Technology Assessment, No. 32 Archived 2012-05-09 at the Wayback Machine. (2001). In AHRQ Archive. Retrieved 2/29/2012.
- ↑ Pazarlis, Konstantinos; Punga, Anna; Schizas, Nikos; Sandén, Bengt; Michaëlsson, Karl; Försth, Peter (2019-08-01). "Study protocol for a randomised controlled trial with clinical, neurophysiological, laboratory and radiological outcome for surgical versus non-surgical treatment for lumbar spinal stenosis: the Uppsala Spinal Stenosis Trial (UppSten)". BMJ Open. 9 (8): e030578. doi:10.1136/bmjopen-2019-030578. ISSN 2044-6055. PMC 6707759. PMID 31434781. Archived from the original on 2020-02-21. Retrieved 2020-02-21.
External links
| Classification | |
|---|---|
| External resources |
- Uvm.edu Archived 2015-04-17 at the Wayback Machine
- Ncbi.nlm.nih.gov Archived 2014-02-18 at the Wayback Machine
- Questions and Answers about Spinal Stenosis Archived 2015-02-04 at the Wayback Machine - US National Institute of Arthritis and Musculoskeletal and Skin Diseases