Snyder–Robinson syndrome
| Snyder–Robinson syndrome | |
|---|---|
| Other names: Spermine synthase deficiency | |
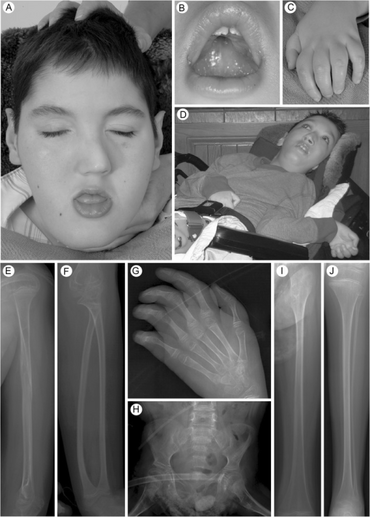 | |
| Snyder–Robinson syndrome-a,b) Face c) hand d) hands e) left humerus f) left forearm g) left hand h) pelvis i)left femur j)left lower leg | |
| Symptoms | Intellectual disability, facial asymmetry, kyphoscoliosis, osteoporosis, hypotonia, asthenic build, seizures |
| Usual onset | Adolescence, childhood, infancy |
| Causes | Genetic[1] |
| Differential diagnosis | Glycerol kinase deficiency, Urban syndrome, Rett syndrome, cerebral palsy, Prader–Willi syndrome |
| Frequency | <1 per 1,000,000 |
Snyder–Robinson syndrome (SRS) is an extremely rare inherited genetic disorder[1] characterized by muscular and skeletal abnormalities, varying degrees of intellectual disability, seizures,[2] and slow development.[3]
SRS is caused by a mutated SMS gene at chromosome Xp21.3-p22.12, which carries instructions for producing the enzyme spermine synthase.[4] Spermine synthase in turn helps the body produce spermine, a polyamine critical to cell processes such as cell division, tissue repair, and apoptosis.[5] The resulting shortage of spermine in cells causes problems with development and brain function, though the exact mechanism is not understood.
The syndrome has also been referred to as Snyder–Robinson X-linked mental retardation syndrome (MRXSSR) and spermine synthase deficiency. SRS exclusively affects males.[1] Only about ten families currently have a child with SRS, and 50 people have been diagnosed worldwide since 1969.[6]
Signs and symptoms
Snyder–Robinson usually is noticeable in infants, causing hypotonia and declining muscle tone with age. Seizures can occur in childhood, and children are especially susceptible to broken bones.[3]
During early childhood, SRS causes mild to profound intellectual disability; speech difficulties; problems with walking; osteoporosis; marfanoid habitus; and scoliosis, kyphosis, or both (kyphoscoliosis). Distinctive facial features include a cleft palate, facial asymmetry, and a prominent lower lip. Kidney problems may also occur, such as nephrocalcinosis and renal cysts.[citation needed]
Cause
SRS is a recessive X-linked condition.[7] There are no known female cases, as both copies of the X chromosome would need to be mutated.[citation needed]
Diagnosis
When SRS is suspected, doctors will order a molecular genetic test to confirm a mutation in the SMS gene—specifically a "hemizygous loss-of-function... pathogenic variant". However, there are currently no formal criteria for a diagnosis.[3]
Management
Individuals with Snyder–Robinson may be assisted by occupational therapy, physical or speech therapy. Anti-seizure medications such as carbamazepine, phenobarbital, and clobazam can be used to manage seizures[2]—the medication used often is influenced by the type of seizure. Bone density can be determined via a DXA scan and may be improved with calcium supplements.[3]
In 2014, several parents of individuals with SRS founded the Snyder–Robinson Foundation, a 501(c)(3) non-profit based in the US.[8][6] It is a member of the National Organization for Rare Disorders.[9]
History
SRS was first reported in a 1969 paper published in Clinical Pediatrics by Russell D. Snyder[10] and Arthur Robinson, who described the syndrome as "recessive sex-linked mental retardation in the absence of other recognizable abnormalities".[11]
References
- ↑ 1.0 1.1 1.2 "Snyder-Robinson syndrome". Genetics Home Reference. NIH. Archived from the original on 28 July 2018. Retrieved 1 July 2019.
- ↑ 2.0 2.1 Rosato, Donna (June 21, 2017). "Who's on Medicaid Might Surprise You". Consumer Reports. Archived from the original on 3 May 2019. Retrieved 1 July 2019.
- ↑ 3.0 3.1 3.2 3.3 Albert, Jessica; Schwartz, Charles E.; Boerkoel, Cornelius F.; Stevenson, Roger E. (June 27, 2013). "Snyder-Robinson Syndrome". GeneReviews. Seattle: University of Washington, Seattle. PMID 23805436. Archived from the original on 27 January 2016. Retrieved 1 July 2019.
- ↑ Cason, A. Lauren; Ikeguchi, Yoshihiko; Skinner, Cindy; Wood, Tim C.; Holden, Kenton R.; Lubs, Herbert A.; Martinez, Francisco; Simensen, Richard J.; Stevenson, Roger E.; Pegg, Anthony E.; Schwartz, Charles E. (24 September 2003). "X-linked spermine synthase gene (SMS) defect: the first polyamine deficiency syndrome". European Journal of Human Genetics. 11 (12): 937–944. doi:10.1038/sj.ejhg.5201072. PMID 14508504.
- ↑ Murray-Stewart, Tracy; Dunworth, Matthew; Foley, Jackson R.; Schwartz, Charles E.; Casero, Jr., Robert A. (7 December 2018). "Polyamine Homeostasis in Snyder-Robinson Syndrome". Medical Sciences. Polyamine Metabolism in Disease and Polyamine-Targeted Therapies. 6 (4): 112. doi:10.3390/medsci6040112. ISSN 2076-3271. PMC 6318755. PMID 30544565.
- ↑ 6.0 6.1 Gilreath, Ariel (March 10, 2018). "GGC hopes to create model for researching rare diseases". The Index-Journal. Archived from the original on 28 December 2019. Retrieved 1 July 2019.
- ↑ "X-linked intellectual disability, Snyder type". Orphanet. Archived from the original on 15 November 2017. Retrieved 1 July 2019.
- ↑ Miranda, Coty Dolores (January 13, 2019). "Dr. Mary Jo Kutler closes out cherished practice". Ahwatukee Foothills News. Archived from the original on 19 January 2019. Retrieved 1 July 2019.
- ↑ "About Us". The Snyder-Robinson Foundation. 2019-06-15. Archived from the original on 2019-07-01. Retrieved 1 July 2019.
- ↑ Snyder, Russell D. (July 1, 1968). "Facial Palsy Following Measles Vaccination, a Possible Connection". Pediatrics. 42 (1): 215–216. ISSN 0031-4005. PMID 5657694. Archived from the original on January 11, 2022. Retrieved July 15, 2021.
- ↑ Snyder, Russell D.; Robinson, Arthur (November 1, 1969). "Recessive Sex-Linked Mental Retardation in the Absence of Other Recognizable Abnormalities: Report of a Family". Clinical Pediatrics. 8 (11): 669–674. doi:10.1177/000992286900801114. PMID 5823961. S2CID 32198336.
External links
- The Snyder–Robinson Foundation Archived 2021-04-23 at the Wayback Machine
- Albert, Jessica; Schwartz, Charles E.; Boerkoel, Cornelius F.; Stevenson, Roger E. (June 27, 2013). "Snyder-Robinson Syndrome". GeneReviews. Seattle: University of Washington, Seattle. PMID 23805436. Archived from the original on 27 January 2016. Retrieved 1 July 2019.
- Snyder, Russell D.; Robinson, Arthur (November 1, 1969). "Recessive Sex-Linked Mental Retardation in the Absence of Other Recognizable Abnormalities: Report of a Family". Clinical Pediatrics. 8 (11): 669–674. doi:10.1177/000992286900801114. PMID 5823961. S2CID 32198336.
| Classification | |
|---|---|
| External resources |