Hiatal hernia
| Hiatal hernia | |
|---|---|
| Other names: Hiatus hernia | |
 | |
| A drawing of a hiatal hernia | |
| Specialty | Gastroenterology, general surgery |
| Symptoms | Taste of acid in the back of the mouth, heartburn, trouble swallowing[1] |
| Complications | Iron deficiency anemia, volvulus, bowel obstruction[1] |
| Types | Sliding, paraesophageal[1] |
| Risk factors | Obesity, older age, major trauma[1] |
| Diagnostic method | Endoscopy, medical imaging, manometry[1] |
| Treatment | Raising the head of the bed, weight loss, medications, surgery[1] |
| Medication | H2 blockers, proton pump inhibitors[1] |
| Frequency | 10–80% (US)[1] |
A hiatal hernia is a type of hernia in which abdominal organs (typically the stomach) slip through the diaphragm into the middle compartment of the chest.[1][2] This may result in gastroesophageal reflux disease (GERD) or laryngopharyngeal reflux (LPR) with symptoms such as a taste of acid in the back of the mouth or heartburn.[1][2] Other symptoms may include trouble swallowing and chest pains.[1] Complications may include iron deficiency anemia, volvulus, or bowel obstruction.[1]
The most common risk factors are obesity and older age.[1] Other risk factors include major trauma, scoliosis, and certain types of surgery.[1] There are two main types: sliding hernia, in which the body of the stomach moves up; and paraesophageal hernia, in which an abdominal organ moves beside the esophagus.[1] The diagnosis may be confirmed with endoscopy or medical imaging.[1] Endoscopy is typically only required when concerning symptoms are present, symptoms are resistant to treatment, or the person is over 50 years of age.[1]
Symptoms from a hiatal hernia may be improved by changes such as raising the head of the bed, weight loss, and adjusting eating habits.[1] Medications that reduce gastric acid such as H2 blockers or proton pump inhibitors may also help with the symptoms.[1] If the condition does not improve with medications, a surgery to carry out a laparoscopic fundoplication may be an option.[1]
Between 10% and 80% of people in the United States are affected.[1] Women are more commonly affected than men.[3] The condition becomes more common with age.[3] Hiatal hernias were first reported in 1853, and first diagnosed using x-rays in 1900.[4]
Signs and symptoms

Hiatal hernia has often been called the "great mimic" because its symptoms can resemble many disorders. Among them, a person with a hiatal hernia can experience dull pains in the chest, shortness of breath (caused by the hernia's effect on the diaphragm), heart palpitations (due to irritation of the vagus nerve), and swallowed food "balling up" and causing discomfort in the lower esophagus until it passes on to the stomach. In addition, hiatal hernias often result in heartburn but may also cause chest pain or pain with eating.[1]
In most cases however, a hiatal hernia does not cause any symptoms. The pain and discomfort that a patient experiences is due to the reflux of gastric acid. While there are several causes of acid reflux, it occurs more frequently in the presence of hiatal hernia.[5][6]
In newborns, the presence of Bochdalek hernia can be recognised[7] from symptoms such as difficulty breathing[8] fast respiration, increased heart rate.[9]
Causes
The following are potential causes of a hiatal hernia.[10] Increased pressure within the abdomen caused by:[10]
- Heavy lifting or bending over
- Frequent or hard coughing
- Hard sneezing
- Violent vomiting
- Straining during defecation (i.e., the Valsalva maneuver)
Obesity and older age are also general risk factors.[10]
Diagnosis
The diagnosis of a hiatal hernia is typically made through an upper GI series, endoscopy or high resolution manometry.[11]
-
A large hiatal hernia on chest X-ray marked by open arrows in contrast to the heart borders marked by closed arrows
-
This hiatal hernia is mainly identified by an air-fluid level (labeled with arrows).
-
Upper GI endoscopy depicting hiatal hernia
-
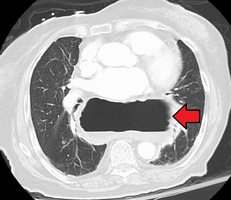
A hiatal hernia as seen on CT
-
A large hiatal hernia as seen on CT imaging
-
A large hiatal hernia as seen on CT imaging
-
As seen on ultrasound[12]
-
As seen on ultrasound[12]
Classification

Four types of esophageal hiatal hernia are identified:[13][14]
Type I: A type I hernia, also known as a sliding hiatal hernia, occurs when part of the stomach slides up through the hiatal opening in the diaphragm.[15] There is a widening of the muscular hiatal tunnel and circumferential laxity of the phrenoesophageal ligament, allowing a portion of the gastric cardia to herniate upward into the posterior mediastinum. The clinical significance of type I hernias is in their association with reflux disease. Sliding hernias are the most common type and account for 95% of all hiatal hernias.[16] (C)
Type II: A type II hernia, also known as a paraesophageal or rolling hernia, occurs when the fundus and greater curvature of the stomach roll up through the diaphragm, forming a pocket alongside the esophagus.[15] It results from a localized defect in the phrenoesophageal ligament while the gastroesophageal junction remains fixed to the pre aortic fascia and the median arcuate ligament[13]. The gastric fundus then serves as the leading point of herniation. Although type II hernias are associated with reflux disease, their primary clinical significance lies in the potential for mechanical complications[13]. (D)
Type III: Type III hernias have elements that indicates progressive enlargement of the hernia through the hiatus, the phrenoesophageal ligament stretches, displacing the gastroesophageal junction above the diaphragm[17][18]
Type IV: Type IV hiatus hernia is associated with a large defect in the phrenoesophageal ligament, allowing other organs, such as colon, spleen and small intestine to enter the hernia sac.[14] The end stage of type I and type II hernias occurs when the whole stomach migrates up into the chest by rotating 180° around its longitudinal axis, with the cardia and pylorus as fixed points. In this situation the abnormality is usually referred to as an intrathoracic stomach.[19]
Treatment
In the great majority of cases, people experience no significant discomfort, and no treatment is required. People with symptoms should elevate the head of their beds and avoid lying down directly after meals.[1] If the condition has been brought on by being overweight, weight loss may be indicated.[20]
Medications
In terms of medications for this condition, antisecretory drugs like proton pump inhibitors and H2 receptor blockers can be used to reduce acid secretion.[21]
Procedures
There is tentative evidence from non controlled trials that oral neuromuscular training may improve symptoms.[22]
Surgery
Surgery may be considered if reflux symptoms are not well controlled by medical therapy, if life long medication needs to be avoided, or there is presence of complications such as Barrett's esophagus, ulcer or stricture.[23][24] The operation is usually a fundoplication, also known as a Nissen fundoplication.[1][25][26] It involves wrapping the upper part of the stomach, the gastric fundus, around the lower part of the esophagus, preventing herniation of the stomach through the diaphragm, thereby reducing the reflux of gastric acid, and has been increasingly performed laparoscopically since the 1990s.[23][25] Complications are rare,[25] and include most commonly difficulty swallowing and bloating, which usually settle with time.[25] Haemorrhage, surgical hernias and infection can also occur.[25] Recovery is usually quick and long term results good.[23]
Epidemiology
Incidence of hiatal hernias increases with age; approximately 60% of individuals aged 50 or older have a hiatal hernia.[27] Of these, 9% are symptomatic, depending on the competence of the lower esophageal sphincter (LES). 95% of these are "sliding" hiatal hernias, in which the LES protrudes above the diaphragm along with the stomach,[28] and only 5% are the paraesophageal, in which the LES remains stationary, but the stomach protrudes above the diaphragm.[29]
Hiatal hernias are most common in North America and Western Europe and rare in rural African communities.[30] Some have proposed that insufficient dietary fiber and the use of a high sitting position for defecation may increase the risk.[31]
History
Hiatal hernias were first reported in 1853 by Bowditch. Two years later, Rokitansky showed that inflammation of the esophagus was due to acid reflux, and in 1900 hiatal hernias were diagnosed by Hirsch using x-rays.[4]
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 1.18 1.19 1.20 1.21 1.22 1.23 Roman, S; Kahrilas, PJ (23 October 2014). "The diagnosis and management of hiatus hernia". British Medical Journal (Clinical Research Ed.). 349: g6154. doi:10.1136/bmj.g6154. PMID 25341679. Archived from the original on 28 August 2021. Retrieved 16 December 2019.
However, the exact prevalence of hiatus hernia is difficult to determine because of the inherent subjectivity in diagnostic criteria. Consequently, estimates vary widely—for example, from 10% to 80% of the adult population in North America
- ↑ 2.0 2.1 "Hiatal Hernia". PubMed Health. Archived from the original on 28 April 2017. Retrieved 6 May 2017.
- ↑ 3.0 3.1 Smith, RE; Shahjehan, RD (January 2020). "Hiatal Hernia". PMID 32965871.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ 4.0 4.1 Stylopoulos, Nicholas; Rattner, David W. (January 2005). "The History of Hiatal Hernia Surgery". Annals of Surgery. 241 (1): 185–193. doi:10.1097/01.sla.0000149430.83220.7f. ISSN 0003-4932. PMID 15622007. Archived from the original on 2018-08-10. Retrieved 2021-01-14.
- ↑ Ferri, Fred F. (2014). Ferri's Clinical Advisor 2015 E-Book: 5 Books in 1. Elsevier Health Sciences. p. 970. ISBN 978-0-323-08430-7. Archived from the original on 28 August 2021. Retrieved 9 January 2021.
- ↑ "Symptoms & Causes of GER & GERD | NIDDK". National Institute of Diabetes and Digestive and Kidney Diseases. Archived from the original on 10 January 2021. Retrieved 9 January 2021.
- ↑ Chang SW, Lee HC, Yeung CY, Chan WT, Hsu CH, Kao HA, Hung HY, Chang JH, Sheu JC, Wang NL (2010). "A twenty-year review of early and late-presenting congenital Bochdalek diaphragmatic hernia: are they different clinical spectra?". Pediatrics and Neonatology. 51 (1): 26–30. doi:10.1016/S1875-9572(10)60006-X. PMID 20225535.
- ↑ Ganeshan DM, Correa AM, Bhosale P, Vaporciyan AA, Rice D, Mehran RJ, Walsh GL, Iyer R, Roth JA, Swisher SG, Hofstetter WL (2013). "Diaphragmatic hernia after esophagectomy in 440 patients with long-term follow-up". Ann Thorac Surg. 96 (4): 1138–45. doi:10.1016/j.athoracsur.2013.04.076. PMID 23810174.
- ↑ Alam, A; Chander, B.N. (July 2005). "Adult bochdalek hernia". MJAFI. 61 (3): 284–6. doi:10.1016/S0377-1237(05)80177-7. PMC 4925637. PMID 27407781.
- ↑ 10.0 10.1 10.2 "Hiatal hernia - Symptoms and causes". Mayo Clinic. Archived from the original on 28 September 2019. Retrieved 6 January 2021.
- ↑ Weitzendorfer, Michael; Köhler, Gernot; Antoniou, Stavros A.; Pallwein-Prettner, Leo; Manzenreiter, Lisa; Schredl, Philipp; Emmanuel, Klaus; Koch, Oliver Owen (2017). "Preoperative diagnosis of hiatal hernia: barium swallow X-ray, high-resolution manometry, or endoscopy?". European surgery: ACA: Acta chirurgica Austriaca. 49 (5): 210–217. doi:10.1007/s10353-017-0492-y. ISSN 1682-8631. Archived from the original on 17 December 2020. Retrieved 10 January 2021.
- ↑ 12.0 12.1 "UOTW #39 - Ultrasound of the Week". Ultrasound of the Week. 25 February 2015. Archived from the original on 9 May 2017. Retrieved 27 May 2017.
- ↑ 13.0 13.1 13.2 Kahrilas, Peter J.; Kim, Hyon C.; Pandolfino, John E. (2008). "Approaches to the diagnosis and grading of hiatal hernia". Best Practice & Research. Clinical Gastroenterology. pp. 601–616. doi:10.1016/j.bpg.2007.12.007. Archived from the original on 28 August 2021. Retrieved 18 January 2021.
- ↑ 14.0 14.1 Kissane, Nicole A.; Rattner, David W. (2012). "41. Paraesophageal and other complex diaphragmatic hernia". In Yeo, Charles J.; Pemberton, John H.; Peters, Jeffrey H.; Matthews, Jeffrey B.; McFadden, David W (eds.). Shackelford's Surgery of the Alimentary Tract E-Book. Philadelphia: Elsevier. p. 494. ISBN 978-1-4377-2206-2. Archived from the original on 2021-08-28. Retrieved 2021-01-10.
- ↑ 15.0 15.1 Lewis, Sharon Mantik (2017). Medical-surgical nursing : assessment and management of clinical problems. Bucher, Linda,, Heitkemper, Margaret M. (Margaret McLean),, Harding, Mariann (10th ed.). St. Louis, Missouri. ISBN 978-0-323-32852-4. OCLC 944472408.
- ↑ Dennis Kasper; Anthony Fauci; Stephen Hauser; Dan Longo; J. Larry Jameson; Joseph Loscalzo (8 April 2015). Harrison's Principles of Internal Medicine, 19e (19 ed.). McGraw-Hill Global Education. p. 1902. ISBN 978-0071802154.
- ↑ Migaczewski, Marcin; Grzesiak-Kuik, Agata; Pędziwiatr, Michał; Budzyński, Andrzej (2014). "Laparoscopic treatment of type III and IV hiatal hernia – authors' experience". Videosurgery and other Miniinvasive Techniques. 9 (2): 157–163. doi:10.5114/wiitm.2014.41625. ISSN 1895-4588. Archived from the original on 28 August 2021. Retrieved 12 January 2021.
- ↑ Moreno, Courtney Coursey; Mittal, Pardeep Kumar (2014). Gastrointestinal Imaging: A Teaching File. Lippincott Williams & Wilkins. p. 8. ISBN 978-1-4511-7337-6. Archived from the original on 28 August 2021. Retrieved 12 January 2021.
- ↑ Abbara, Suhny; Kalan, Mohammed M. H.; Lewicki, Ann M. (1 August 2003). "Intrathoracic Stomach Revisited". American Journal of Roentgenology. 181 (2): 403–414. doi:10.2214/ajr.181.2.1810403. ISSN 0361-803X. Archived from the original on 28 August 2021. Retrieved 10 January 2021.
- ↑ Thomas (Jr.), Donald E.; Jr, Donald E. Thomas (2014). The Lupus Encyclopedia: A Comprehensive Guide for Patients and Families. JHU Press. p. 447. ISBN 978-1-4214-0984-9. Archived from the original on 28 August 2021. Retrieved 18 January 2021.
- ↑ Linton, Adrianne Dill (2014). Introduction to Medical-Surgical Nursing - E-Book. Elsevier Health Sciences. p. 802. ISBN 978-0-323-29363-1. Archived from the original on 29 August 2021. Retrieved 9 January 2021.
- ↑ "Clinical and technical evidence | IQoro for hiatus hernia | Advice | NICE". www.nice.org.uk. Archived from the original on 28 August 2021. Retrieved 23 April 2020.
- ↑ 23.0 23.1 23.2 Pham, Thai H.; O'Rourke, Robert W.; Hunter, John G. (2012). "18. Laparoscopic and Open Nissan fundoplication". In Yeo, Charles J.; Pemberton, John H.; Peters, Jeffrey H.; Matthews, Jeffrey B.; McFadden, David W (eds.). Shackelford's Surgery of the Alimentary Tract E-Book. Philadelphia: Elsevier. pp. 226–228. ISBN 978-1-4377-2206-2. Archived from the original on 2021-08-28. Retrieved 2021-01-14.
- ↑ Stylopoulos N, Gazelle GS, Rattner DW (2002). "Paraesophageal hernias: operation or observation?". Ann Surg. 236 (4): 492–500. doi:10.1097/00000658-200210000-00012. PMC 1422604. PMID 12368678.
- ↑ 25.0 25.1 25.2 25.3 25.4 NHS (2010). "Laparoscopic nissen fundoplication: Patient information" (PDF). Oxford Radcliffe Hospitals NHS Trust. Archived (PDF) from the original on 17 May 2017. Retrieved 14 January 2021.
- ↑ Ozmen V, Oran ES, Gorgun E, Asoglu O, Igci A, Kecer M, Dizdaroglu F (2006). "Histologic and clinical outcome after laparoscopic Nissen fundoplication for gastroesophageal reflux disease and Barrett's esophagus". Surg Endosc. 20 (2): 226–9. doi:10.1007/s00464-005-0434-9. PMID 16362470.
- ↑ Goyal Raj K, "Chapter 286. Diseases of the Esophagus". Harrison's Principles of Internal Medicine, 17e.
- ↑ Watson, Thomas J.; Moritz, Troy (2020). "Sliding Hernia". StatPearls. StatPearls Publishing. Archived from the original on 28 August 2021. Retrieved 18 January 2021.
- ↑ Smith, Ryan E.; Shahjehan, Rai Dilawar (2020). "Hiatal Hernia". StatPearls. StatPearls Publishing. Archived from the original on 28 August 2021. Retrieved 18 January 2021.
- ↑ Burkitt DP (1981). "Hiatus hernia: is it preventable?". Am. J. Clin. Nutr. 34 (3): 428–31. doi:10.1093/ajcn/34.3.428. PMID 6259926.
- ↑ Sontag S (1999). "Defining GERD". Yale J Biol Med. 72 (2–3): 69–80. PMC 2579007. PMID 10780568.
External links
| Classification | |
|---|---|
| External resources |
- Hiatal hernia CT Scans Archived 2016-03-08 at the Wayback Machine - CT Cases