Rheumatoid nodule
| Rheumatoid nodule | |
|---|---|
 | |
| Micrograph of a rheumatoid nodule, showing the characteristic palisading granuloma with a core consisting of necrotic collagen and fibrin. H&E stain. | |
| Specialty | Rheumatology |
A rheumatoid nodule is a lump of tissue, or an area of swelling, that appear on the exterior of the skin usually around the olecranon (tip of the elbow) or the interphalangeal joints (finger knuckles), but can appear in other areas.[1] There are four different types of rheumatoid nodules: subcutaneous rheumatoid nodules, cardiac nodules, pulmonary nodules, and central nervous systems nodules. These nodules occur almost exclusively in association with rheumatoid arthritis. Very rarely do rheumatoid nodules occur as rheumatoid nodulosis (multiple nodules on the hands or other areas) in the absence of rheumatoid arthritis. Rheumatoid nodules can also appear in other areas of the body other than the skin. Less commonly they occur in the lining of the lung or other internal organs. The occurrence of nodules in the lung of miners exposed to silica dust was known as Caplan’s syndrome.[2] Rarely, the nodules occur at diverse sites on body (e.g. upper eyelid, distal region of the soles of the feet, vulva and internally in the gallbladder, lung, heart valves, larynx, and spine).[3]
Rheumatoid nodules can vary in size from 2 mm to 5 cm and are usually rather firm to the touch. Quite often they are associated with synovial pockets or bursae. About 5% of people with rheumatoid arthritis have such nodules within two years of disease onset, and the cumulative prevalence is about 20 to 30%.[4] Risk factors of developing rheumatoid nodules include as smoking and trauma to small vessels.[5]
In the majority of the time, nodules are not painful or disabling in any way. They are usually more of an unsightly nuisance. However, rheumatoid nodules can become painful when infection or ulcers occur on the skin of the nodule. Some nodules can actually disappear over time, but other times, they can grow larger making prediction of nodular size difficult to predict.[6]
Treatment also can be quite difficult, but surgical removal and injection of corticosteroids have both shown good results towards the treatment for rheumatoid nodules.
Signs and symptoms
The clinical presentation of Rheumatoid nodules is well-demarcated, flesh colored, subcutaneous lumps[7]
Risk Factors
Rheumatoid nodules develop if a person currently has rheumatoid arthritis. However, not all people with rheumatoid arthritis develop rheumatoid nodules. Some risk factors for rheumatoid nodules for people with rheumatoid arthritis may include:[5]
- Smoking (strong association)
- Elevated levels of serum rheumatoid factors
- HLA-DRB1 gene (weak association)
- Trauma to small vessels
- Having severe rheumatoid arthritis
- Taking Methotrexate over other arthritis drugs[8]
Pathophysiology
Although the exact process is unknown, there are a few hypotheses for the generation of rheumatoid nodules. It has been observed that rheumatoid nodules frequently form over extensor sites and areas vulnerable to trauma.[9] The trauma causes inflammatory particles to build up and leads to a secondary inflammatory response which ultimately causes fibrin release and necrosis.[5] Another hypothesis suggests that the inflammation of blood vessels activates complement components, which leads to the deposit of rheumatoid factors and fibrin.[5]
The rheumatoid nodule is the most common cutaneous manifestation of rheumatoid arthritis (RA).[9] Rheumatoid arthritis involves chronic inflammation of synovial membranes, which leads to degradation of articular cartilage and the juxta-articular bone. Inflammation is caused by T cells, B cells and monocytes when endothelial cells are activated. Neovascularization, or the growth of new blood vessels, serves as an additional marker for rheumatoid arthritis. A hyperplastic synovial lining layer can be caused by the expansion of synovial fibroblast and macrophage cells.[9] This expansion of the synovial membrane, sometimes referred to as "pannus," can lead to bony erosions and cartilage degradation at the site of the cartilage-bone junction in the periarticular bone.[10]
It is important to note that the cause of rheumatoid arthritis is unknown. It is speculated that genetic and environmental factors can both contribute to the development of rheumatoid arthritis. Gene loci and antigens, such as HLA class II antigens, have been seen as closely associated with rheumatoid arthritis.[11] Environmental risk factors include smoking, periodontitis, viral infections and gut, mouth and lung microbiomes. Researchers have noted that Prevotella species, which are expanded in the gastrointestinal tract in early RA, and Porphyromonas gingivalis, which is associated with periodontitis, may have a role in pathogenesis.[12]
Pathology
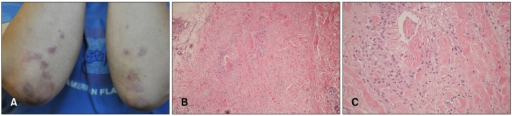
Histological examination of nodules shows that they consist of a shell of fibrous tissue surrounding a center of fibrinoid necrosis.[13] Pea-sized nodules have one centre. Larger nodules tend to be multilocular, with many separate shells or with connections between the necrotic centers. Individual necrotic centers may contain a cleft or several centers of necrosis may all open on to a large bursal pocket containing synovial fluid.
The boundary between the necrotic center and the outer fibrous shell is made up of the characteristic feature of the nodule, which is known as a cellular palisade. The palisade is a densely packed layer of macrophages and fibroblasts which tend to be arranged radially, like the seeds of a kiwifruit or fig.[13] Further out into the fibrous shell there is a zone that contains T cells and plasma cells in association with blood vessels.[14] The histology of pulmonary nodules are similar to that of subcutaneous nodules, with central necrosis surrounded by palisading macrophages and inflammatory infiltrate.[5]
Diagnosis
Differential diagnosis of rheumatoid nodules can be classified from localization, depth pathology, age of onset, persistence, rheumatoid factor, concomitant joint disease, and bone erosions. Diagnosis is typically determined clinically by a rheumatologist.[5] Rheumatoid arthritis associated rheumatoid nodules are typically subcutaneous and occur at extensor sites. The onset typically starts in adulthood and presents with rheumatoid factors and bone erosions, and concomitant joint diseases. The pathology is characterized by central necrosis, palisading mononuclear cells, and perivascular lymphocytic infiltrations.[14]
Rheumatoid nodulosis is characterized by multiple subcutaneous nodules presenting with rheumatoid factors but an absence of joint complaints. The nodules are typically small and concentrated on the extensor sites of the hands and feet, sometimes accompanied by bone erosions. The onset typically starts in adulthood with a pathology similar to rheumatoid arthritis associated rheumatoid nodules.[14]
Benign rheumatoid nodules are often not associated with rheumatoid factors or concomitant joint diseases.[15] They are typically found on the feet, scalp, and pretibial regions. Frequently seen in children before the age of 18, the pathology is similar to that of rheumatoid arthritis associated rheumatoid nodules. The nodules are non-tender and undergo rapid growth, but also resolve spontaneously.[14] A similar presentation occurring more intracutaneously (superficial) is known as granuloma annulare.[14]
Rheumatic fever nodules are typically associated with acute rheumatic fever in children. They are not accompanied by rheumatoid factors or bone erosions, but are associated with concomitant joint diseases. No larger than the size of peas, they are typically found at extensor sites and processus spinosi of the vertebrae. The pathology is characterized by central necrosis and little histiocytic/lymphocytic infiltration.[14][16]
Prevention
There are no methods as of right now to completely prevent the development of rheumatoid nodules, but for those diagnosed with rheumatoid arthritis, proper management of the disease could reduce the risk of nodule formation. Additionally, proper medication adherence, smoking cessation, increasing physical activity, and keeping up with doctor appointments are just some lifestyle changes that could "prevent" nodules.[6]
Treatment
Treatment for rheumatoid nodules may be tricky as some treatments for rheumatoid arthritis can act against the nodules. Common drug therapies for rheumatoid arthritis may show no benefits towards the treatment for rheumatoid nodules. Common drug therapies, such as anti TNF treatment or other immunosuppressive drugs, for rheumatoid arthritis has shown little effect on the nodules.[17] In fact, it has been shown that Methotrexate, a drug often used in rheumatoid arthritis, is actually correlated with the increased risk of nodule formation.[8] Because rheumatoid nodules also cause pain or nerve entrapment, treatment for these symptoms with nonsteroidal anti-inflammatory drugs may be sufficient.[5] Other drug therapies, such as corticosteroids, have shown to decrease nodular size, however, it can increase the risk of infection as well.[18] Local corticosteroid injections seems to be the most studied treatment for rheumatoid nodules as of now.
Surgery to have the nodule removed is another option that can be done to treat rheumatoid nodules. However, usually these are usually only indicated in the case of eroding/ necrotising skin.[19]
Prevalence
There are 4 different types of rheumatoid nodules: subcutaneous rheumatoid nodules, cardiac nodules, pulmonary nodules and central nervous system nodules.
Subcutaneous rheumatoid nodules
According to a study done by the BARFOT study group, 7% of individuals diagnosed with rheumatoid arthritis reported the presence of subcutaneous rheumatoid nodules upon initial diagnosis. And about 30-40% of all those diagnosed with rheumatoid arthritis reported developing these nodules throughout the course of the disease.[20] Subcutaneous rheumatoid nodules is correlated with the increased risk of cardiovascular and respiratory disease, and those with detected subcutaneous rheumatoid nodules should be assessed for cardiovascular and respiratory risk factors.[1]
Cardiac nodules
Rheumatoid nodules may also form in the heart. Specifically, it could develop in the myocardium, pericardium, and other valvular structures, and these nodules can be discovered through echocardiograms.[21] There are little studies with minimal data on the development of cardiac nodules in association with rheumatoid arthritis, but the general consensus is that such occurrences is relatively rare.
Pulmonary Nodules
The reported prevalence of pulmonary nodules has varying depending on the method of detection. In a 1984 study done on lung biopsies in rheumatoid arthritis, the reported prevalence was about 32% in a sample size of 40 individuals.[22] However, another clinical study utilizing a different method of detection; plain film radiographs of the chest; showed that only 2 out of 516 people (~0.4%) diagnosed with rheumatoid arthritis developed pulmonary nodules.[23] Additionally, other clinical studies have reported increased pulmonary nodule growth following treatments with methotrexate,[8] leflunomide,[24] and etanercept.[25]
Central nervous system nodules
Like cardiac nodules, nodules developing in the central nervous system is also relatively rare. Most reports of nodule growth on the central nervous system also presented with severe stages of erosive joint diseases.[26] Generally, these nodules can be detected through MRI and confirmed through biopsies. As of right now, there are no known mediations that have been reported in reducing nodules in the central nervous systems.
See also
References
- ↑ 1.0 1.1 "UpToDate". www.uptodate.com. Archived from the original on 2022-02-21. Retrieved 2020-07-31.
- ↑ "Rheumatoid pneumoconiosis: MedlinePlus Medical Encyclopedia". medlineplus.gov. Archived from the original on 2019-07-27. Retrieved 2020-07-31.
- ↑ Upile T, Jerjes W, Sipaul F, Singh S, Hopper C, Wright A, Sandison A (October 2007). "Rheumatoid nodule of the thyrohyoid membrane: a case report". Journal of Medical Case Reports. 1: 123. doi:10.1186/1752-1947-1-123. PMC 2174496. PMID 17974016.
- ↑ "Rheumatoid Arthritis Symptoms". Johns Hopkins Arthritis Center. Archived from the original on 2020-09-20. Retrieved 2020-07-31.
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 5.6 Tilstra JS, Lienesch DW (July 2015). "Rheumatoid Nodules". Dermatologic Clinics. Granulomatous Disorders of Adult Skin. 33 (3): 361–71. doi:10.1016/j.det.2015.03.004. PMID 26143419.
- ↑ 6.0 6.1 "Rheumatoid nodules: Symptoms, causes, and pictures". www.medicalnewstoday.com. 2017-10-28. Archived from the original on 2020-10-31. Retrieved 2020-07-31.
- ↑ "RHEUMATOID NODULES". AOCD. Archived from the original on 4 March 2022. Retrieved 3 March 2022.
- ↑ 8.0 8.1 8.2 Takashima S, Ota M (July 2015). "Methotrexate-induced nodulosis". CMAJ. 187 (10): E327. doi:10.1503/cmaj.140852. PMC 4500730. PMID 25780053.
- ↑ 9.0 9.1 9.2 Sayah A, English JC (August 2005). "Rheumatoid arthritis: a review of the cutaneous manifestations". Journal of the American Academy of Dermatology. 53 (2): 191–209, quiz 210–2. doi:10.1016/j.jaad.2004.07.023. PMID 16021111.
- ↑ Aletaha D, Smolen JS (October 2018). "Diagnosis and Management of Rheumatoid Arthritis: A Review". JAMA. 320 (13): 1360–1372. doi:10.1001/jama.2018.13103. PMID 30285183. S2CID 52914947.
- ↑ Kampstra AS, Toes RE (August 2017). "HLA class II and rheumatoid arthritis: the bumpy road of revelation". Immunogenetics. 69 (8–9): 597–603. doi:10.1007/s00251-017-0987-5. PMC 5537318. PMID 28695293.
- ↑ Tan EM, Smolen JS (September 2016). "Historical observations contributing insights on etiopathogenesis of rheumatoid arthritis and role of rheumatoid factor". The Journal of Experimental Medicine. 213 (10): 1937–50. doi:10.1084/jem.20160792. PMC 5030811. PMID 27621417.
- ↑ 13.0 13.1 Ziff M (June 1990). "The rheumatoid nodule". Arthritis and Rheumatism. 33 (6): 761–7. doi:10.1002/art.1780330601. PMID 2194460.
- ↑ 14.0 14.1 14.2 14.3 14.4 14.5 Veys EM, De Keyser F (September 1993). "Rheumatoid nodules: differential diagnosis and immunohistological findings". Annals of the Rheumatic Diseases. 52 (9): 625–6. doi:10.1136/ard.52.9.625. PMC 1005134. PMID 8239755.
- ↑ Burry HC, Caughey DE, Palmer DG (December 1979). "Benign rheumatoid nodules". Australian and New Zealand Journal of Medicine. 9 (6): 697–701. doi:10.1111/j.1445-5994.1979.tb04203.x. PMID 294929.
- ↑ Wood MG, Beerman H (February 1960). "Necrobiosis lipoidica, granuloma annulare, and rheumatoid nodule". The Journal of Investigative Dermatology. 34: 139–47. doi:10.1038/jid.1960.20. PMID 13845823.
- ↑ Kekow J, Welte T, Kellner U, Pap T (March 2002). "Development of rheumatoid nodules during anti-tumor necrosis factor alpha therapy with etanercept". Arthritis and Rheumatism. 46 (3): 843–4. doi:10.1002/art.10096. PMID 11920425.
- ↑ Voulgari PV, Papazisi D, Bai M, Zagorianakou P, Assimakopoulos D, Drosos AA (June 2005). "Laryngeal involvement in rheumatoid arthritis". Rheumatology International. 25 (5): 321–5. doi:10.1007/s00296-005-0594-x. PMID 15761726. S2CID 29900567.
- ↑ Arnold C (October 1996). "The management of rheumatoid nodules". American Journal of Orthopedics. 25 (10): 706–8. PMID 8922170.
- ↑ Nyhäll-Wåhlin BM, Jacobsson LT, Petersson IF, Turesson C (May 2006). "Smoking is a strong risk factor for rheumatoid nodules in early rheumatoid arthritis". Annals of the Rheumatic Diseases. 65 (5): 601–6. doi:10.1136/ard.2005.039172. PMC 1798137. PMID 16166104.
- ↑ Kitas G, Banks MJ, Bacon PA (2001-01-01). "Cardiac involvement in rheumatoid disease". Clinical Medicine. 1 (1): 18–21. doi:10.7861/clinmedicine.1-1-18. PMC 4952030. PMID 11358070.
- ↑ Koslow M, Young JR, Baqir M, Joanne EY, Johnson G, Ryu J (October 2017). "Clinical and Imaging Features Distinguish Rheumatoid Pulmonary Nodules From Malignancy in Rheumatoid Patients". Chest. 152 (4): A752. doi:10.1016/j.chest.2017.08.782.
- ↑ Walker WC, Wright V (November 1968). "Pulmonary lesions and rheumatoid arthritis". Medicine. 47 (6): 501–20. doi:10.1097/00005792-196811000-00003. PMID 5727884. S2CID 41885830.
- ↑ Rozin A, Yigla M, Guralnik L, Keidar Z, Vlodavsky E, Rozenbaum M, et al. (May 2006). "Rheumatoid lung nodulosis and osteopathy associated with leflunomide therapy". Clinical Rheumatology. 25 (3): 384–8. doi:10.1007/s10067-005-0024-1. PMID 16211338. S2CID 10001824.
- ↑ Watson P, Simler N, Screaton N, Lillicrap M (June 2008). "Management of accelerated pulmonary nodulosis following etanercept therapy in a patient with rheumatoid arthritis". Rheumatology. 47 (6): 928–9. doi:10.1093/rheumatology/ken102. PMID 18385217.
- ↑ Takahashi M, Yamamoto J, Idei M, Nakano Y, Soejima Y, Saito T, et al. (2014). "Multiple intracranial nodules associated with rheumatoid arthritis: case report". Neurologia Medico-Chirurgica. 54 (4): 317–20. doi:10.2176/nmc.cr2012-0259. PMC 4533475. PMID 24140764. Archived from the original on 2022-03-04. Retrieved 2022-01-02.
External links
| Classification |
|---|