Postural orthostatic tachycardia syndrome
| Postural orthostatic tachycardia syndrome | |
|---|---|
| Other names: Postural tachycardia syndrome (POTS) | |
 | |
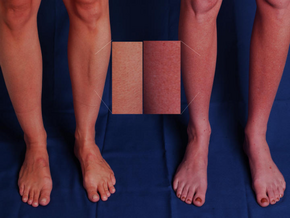
| Cyanosis of the limbs due to POTS | |
| Specialty | Cardiology, neurology |
| Symptoms | With standing: lightheadedness, trouble thinking, blurry vision, weakness[1] |
| Usual onset | Around age 20[1] |
| Duration | > 6 months[2] |
| Causes | Variable[3] |
| Risk factors | Family history[1] |
| Diagnostic method | An increase in heart rate by 30 beats/min with standing[1] |
| Differential diagnosis | Dehydration, heart problems, adrenal insufficiency, Parkinson disease[4] |
| Treatment | Avoiding factors that bring on symptoms, increasing dietary salt and water, compression stockings, exercise, cognitive behavioral therapy, medications[1] |
| Medication | Beta blockers, pyridostigmine, midodrine, and fludrocortisone.[1] |
| Prognosis | ~90% improve with treatment[5] |
| Frequency | ~ 500,000 (US)[4] |
Postural orthostatic tachycardia syndrome (POTS) is a condition in which a change from lying to standing causes an abnormally large increase in heart rate.[1] This occurs with symptoms that may include lightheadedness, trouble thinking, blurred vision or weakness.[1] Other commonly associated conditions include Ehlers–Danlos syndrome, mast cell activation syndrome, irritable bowel syndrome, insomnia, chronic headaches, chronic fatigue syndrome and fibromyalgia.[1]
The causes of POTS are varied.[3] Often, it begins after a viral infection, surgery or pregnancy.[5] Risk factors include a family history of the condition.[1] Diagnosis in adults is based on an increase in heart rate of more than 30 beats per minute within ten minutes of standing up which is accompanied by symptoms.[1] Low blood pressure with standing, however, does not occur.[1] Other conditions which can cause similar symptoms, such as dehydration, heart problems, adrenal insufficiency and Parkinson disease, must not be present.[4]
Treatment may include avoiding factors that bring on symptoms, increasing dietary salt and water, compression stockings, exercise, cognitive behavioral therapy (CBT) and medications.[1][6] Medications used may include beta blockers, pyridostigmine, midodrine or fludrocortisone.[1] More than 50% of people whose condition was triggered by a viral infection get better within five years.[5] About 90% improve with treatment.[5] It is estimated that 500,000 people are affected in the United States.[4] The average age of onset is 20 years old, and it occurs about 5 times more often in females.[1]
Signs and symptoms
In adults, the primary manifestation is an increase in heart rate of more than 30 beats per minute within ten minutes of standing up.[7][8] The resulting heart rate is typically more than 120 beats per minute.[7] For people aged between 12 and 19, the minimum increase for diagnosis is 40 beats per minute.[9] This is known as orthostatic (upright) tachycardia (fast heart rate). It occurs without any coinciding drop in blood pressure, as that would indicate orthostatic hypotension.[8] Certain medications to treat POTS may cause orthostatic hypotension. It is accompanied by other features of orthostatic intolerance—symptoms that develop in an upright position and are relieved by reclining.[8] These orthostatic symptoms include palpitations, light-headedness, chest discomfort, shortness of breath,[8] nausea, weakness or "heaviness" in the lower legs, blurred vision, and cognitive difficulties.[7] Symptoms may be exacerbated with prolonged sitting, prolonged standing, alcohol, heat, exercise, or eating a large meal.[citation needed]
In up to one third of people with POTS,[7] fainting occurs in response to postural changes or exercise.[10] Migraine-like headaches are common, sometimes with symptoms worsening in an upright position (orthostatic headache).[10] 40–50% of patients with POTS develop acrocyanosis of extremities, a reddish-purple color in the legs and/or hands when they stand (indicative of blood pooling).[11][10][12] 48% of people with POTS report chronic fatigue and 32% report sleep disturbances.[13][14][15][16] Others exhibit only the cardinal symptom of orthostatic tachycardia.[10] Additional signs and symptoms are varied, and may include excessive sweating, a lack of sweating, heat intolerance, digestive issues such as bloating, nausea, indigestion, constipation, and diarrhea, a flu-like feeling, coat-hanger pain, forgetfulness, brain fog, and presyncope.[17]
Brain fog
One of the most disabling and prevalent symptoms in POTS is "brain fog",[18] a term used by patients to describe the cognitive difficulties they experience. In one survey of 138 POTS patients, brain fog was defined as “forgetful” (91%), “difficulty thinking” (89%), and “difficulty focusing” (88%). Other common description was "Difficulty processing what others say" (80%), Confusion (71%), Lost (64%), and "Thoughts moving too quickly" (40%)[19] The same survey described the most common triggers of brain fog to be fatigue (91%), lack of sleep (90%), prolonged standing (87%) and dehydration (86%).[citation needed]
Neuropsychological testing has shown that a POTS-patient has reduced attention (Ruff 2&7 speed and WAIS-III digits forward), short-term memory (WAIS-III digits back), cognitive processing speed (Symbol digits modalities test) and executive function (Stroop word color and trails B).[20][21][22]
A potential cause for brain fog is a decrease in cerebral blood flow (CBF), especially in upright position.[23][24][25]
Another theory is that interoception of excessive autonomic activity causes interoceptive prediction errors (PE) to occur.[26] A prediction error is the mismatch between a prior expectation and reality.[27] This would cause anxiety which then overwhelms the consciousness of POTS-patient causing cognitive-affective symptoms. This then makes them predisposed to response-focused emotion regulation (ER) instead of an antecedent-focused ER.[26][28][29][30]
Causes
| Associated conditions[31][32] |
|---|
|
The symptoms of POTS can be caused by several distinct pathophysiological mechanisms.[8] These mechanisms are poorly understood,[9] and can overlap, with many people showing features of multiple POTS types.[8] Many people with POTS exhibit low blood volume (hypovolemia), which can decrease the rate of blood flow to the heart.[8] To compensate for this, the heart increases its cardiac output by beating faster,[33] leading to the symptoms of presyncope and reflex tachycardia.[8]
In the 30% to 60% of cases classified as hyperadrenergic POTS, norepinephrine levels are elevated on standing,[7] often due to hypovolemia or partial autonomic neuropathy.[8] A smaller minority of people with POTS have (typically very high) standing norepinephrine levels that are elevated even in the absence of hypovolemia and autonomic neuropathy; this is classified as central hyperadrenergic POTS.[8][12] The high norepinephrine levels contribute to symptoms of tachycardia.[8] Another subtype, neuropathic POTS, is associated with denervation of sympathetic nerves in the lower limbs.[8] In this subtype, it is thought that impaired constriction of the blood vessels causes blood to pool in the veins of the lower limbs.[7] Heart rate increases to compensate for this blood pooling.[34]
In up to 50% of cases, there was an onset of symptoms following a viral illness.[35] It may also be linked to vaccination, physical trauma, concussion, pregnancy, or surgery.[36][37][10] It is believed that these events could act as a trigger for an autoimmune response that result in POTS.[38]
POTS is more common in females than males. It has also been shown to be linked in patients with acute stressors such as pregnancy, recent surgery, or recent trauma. POTS also has been linked to patients with a history of autoimmune diseases,[36] irritable bowel syndrome, anemia, hyperthyroidism, fibromyalgia, diabetes, amyloidosis, sarcoidosis, systemic lupus erythematosus, and cancer. Genetics likely plays a role, with one study finding that one in eight POTS patients reported a history of orthostatic intolerance in their family.[33]
Autoimmunity
There is an increasing number of studies indicating that POTS is an autoimmune disease.[36][39][40][41][42][43] A high number of patients has elevated levels of autoantibodies against the adrenergic alpha 1 receptor and against the muscarinic acetylcholine M4 receptor.[44][45][46]
Especially elevations of adrenergic α1 receptor is associated with symptoms severity in patients with POTS.[44]
Secondary
If POTS is caused by another condition, it may be classified as secondary POTS.[47] Chronic diabetes mellitus is one common cause.[47] POTS can also be secondary to gastrointestinal disorders that are associated with low fluid intake due to nausea or fluid loss through diarrhea, leading to hypovolemia.[7] Systemic lupus erythematosus and other autoimmune diseases have also been linked to POTS.[36]
There is a subset of patients who present with both POTS and mast cell activation syndrome (MCAS), and it is not yet clear whether MCAS is a secondary cause of POTS or simply comorbid, however, treating MCAS for these patients can significantly improve POTS symptoms.[48]
POTS can also co-occur in all types of Ehlers–Danlos syndrome (EDS),[10] a hereditary connective tissue disorder marked by loose hypermobile joints prone to subluxations and dislocations, skin that exhibits moderate or greater laxity, easy bruising, and many other symptoms. A trifecta of POTS, EDS, and Mast Cell Activation Syndrome (MCAS) is becoming increasingly more common, with a genetic marker common among all three conditions.[49][50][51][52] POTS is also often accompanied by vasovagal syncope, with a 25% overlap being reported.[53] There are some overlaps between POTS and chronic fatigue syndrome, with evidence of POTS in 10–20% of CFS cases.[54][53] Fatigue and reduced exercise tolerance are prominent symptoms of both conditions, and dysautonomia may underlie both conditions.[53]
POTS can sometimes be a paraneoplastic syndrome associated with cancer.[55]
There are case reports of people developing POTS and other forms of dysautonomia post-COVID.[56][57][58][59][60][61][62][63][64][65] There is no good large-scale empirical evidence yet to prove a connection, so for now the evidence is preliminary .[66]
Diagnosis
POTS is most commonly diagnosed by a cardiologist (41%), cardiac electrophysiologist (15%), or Neurologist (19%).[31] The average number of physicians seen before receiving diagnosis is seven, and the average delay before diagnosis is 4.7 years.[31]
Diagnostic criteria
A POTS diagnosis requires the following characteristics:[67]
- For patients age 20 or older, increase in heart rate ≥30 bpm within ten minutes of upright posture (tilt test or standing) from a supine position
- For patients age 12–19, heart rate increase must be >40 bpm[9]
- Associated with related symptoms that are worse with upright posture and that improve with recumbence
- Chronic symptoms that have lasted for longer than six months
- In the absence of other disorders, medications, or functional states that are known to predispose to orthostatic tachycardia
Autoantibodies
Measurement of G protein–coupled receptor activity may be used as a diagnostic tool in the near future.[44]
Orthostatic intolerance
An increase in heart rate upon moving to an upright posture is known as orthostatic (upright) tachycardia (fast heart rate). It occurs without any coinciding drop in blood pressure, as that would indicate orthostatic hypotension.[8] Certain medications to treat POTS may cause orthostatic hypotension. It is accompanied by other features of orthostatic intolerance—symptoms that develop in an upright position and are relieved by reclining.[8] These orthostatic symptoms include palpitations, light-headedness, chest discomfort, shortness of breath,[8] nausea, weakness or "heaviness" in the lower legs, blurred vision, and cognitive difficulties.[7]
Differential diagnoses
A variety of autonomic tests are employed to exclude autonomic disorders that could underlie symptoms, while endocrine testing is used to exclude hyperthyroidism and rarer endocrine conditions.[10] Electrocardiography is normally performed on all patients to exclude other possible causes of tachycardia.[7][10] In cases where a particular associated condition or complicating factor are suspected, other non-autonomic tests may be used: echocardiography to exclude mitral valve prolapse, and thermal threshold tests for small-fiber neuropathy.[10]
Testing the cardiovascular response to prolonged head-up tilting, exercise, eating, and heat stress may help determine the best strategy for managing symptoms.[10] POTS has also been divided into several types (see § Causes), which may benefit from distinct treatments.[68] People with neuropathic POTS show a loss of sweating in the feet during sweat tests, as well as impaired norepinephrine release in the leg,[69] but not arm.[7][68][70] This is believed to reflect peripheral sympathetic denervation in the lower limbs.[69][71][7] People with hyperadrenergic POTS show a marked increase of blood pressure and norepinephrine levels when standing, and are more likely to suffer from prominent palpitations, anxiety, and tachycardia.[72][73][35][68]
People with POTS can be misdiagnosed with inappropriate sinus tachycardia as they present similarly. One distinguishing feature is those with POTS rarely exhibit >100 bpm while in a supine position, while patients with IST often have a resting heart rate >100 bpm. Additionally patients with POTS display a more pronounced change in heart rate in response to postural change.[47]
Treatment
| Aggravating factors[74] |
|---|
|
POTS treatment involves using multiple methods in combination to counteract cardiovascular dysfunction, address symptoms, and simultaneously address any associated disorders.[10] For most patients, water intake should be increased, especially after waking, in order to expand blood volume (reducing hypovolemia).[10] Eight to ten cups of water daily are recommended.[48] Increasing salt intake, by adding salt to food, taking salt tablets, or drinking sports drinks and other electrolyte solutions is an effective way to raise blood pressure by helping the body retain water. Different physicians recommend different amounts of sodium to their patients.[75] Combining these techniques with gradual physical training enhances their effect.[10] In some cases, when increasing oral fluids and salt intake is not enough, intravenous saline or the drug desmopressin is used to help increase fluid retention.[10][12]
Large meals worsen symptoms for some people. These people may benefit from eating small meals frequently throughout the day instead.[10] Alcohol and food high in carbohydrates can also exacerbate symptoms of orthostatic hypotension.[9] Excessive consumption of caffeine beverages should be avoided, because they can promote urine production (leading to fluid loss) and consequently hypovolemia.[10] Exposure to extreme heat may also aggravate symptoms.[48]
Prolonged physical inactivity can worsen the symptoms of POTS.[10] Techniques that increase a person's capacity for exercise, such as endurance training or graded exercise therapy, can relieve symptoms for some patients.[10] Aerobic exercise performed for 20 minutes a day, three times a week, is sometimes recommended for patients who can tolerate it.[75] Exercise may have the immediate effect of worsening tachycardia, especially after a meal or on a hot day.[10] In these cases, it may be easier to exercise in a semi-reclined position, such as riding a recumbent bicycle, rowing, or swimming.[10]
When changing to an upright posture, finishing a meal, or concluding exercise, a sustained hand grip can briefly raise the blood pressure, possibly reducing symptoms.[10] Compression garments can also be of benefit by constricting blood pressures with external body pressure.[10]
Medication
If nonpharmacological methods are ineffective, medication may be necessary.[10] Medications used may include beta blockers, pyridostigmine, midodrine,[76] or fludrocortisone.[77][7] As of 2013, no medication has been approved by the U.S. Food and Drug Administration to treat POTS, but a variety are used off-label.[48] Their efficacy has not yet been examined in long-term randomized controlled trials.[48]
Fludrocortisone may be used to enhance sodium retention and blood volume, which may be beneficial not only by augmenting sympathetically-mediated vasoconstriction, but also because a large subset of POTS patients appear to have low absolute blood volume.[78]
While people with POTS typically have normal or even elevated arterial blood pressure, the neuropathic form of POTS is presumed to constitute a selective sympathetic venous denervation.[78] In these patients the selective Alpha-1 adrenergic receptor agonist midodrine may increase venous return, enhance stroke volume, and improve symptoms.[78] Midodrine should only be taken during the daylight hours as it may promote supine hypertension.[78]
Sinus node blocker Ivabradine can successfully restrain heart rate in POTS without affecting blood pressure, demonstrated in approximately 60% of people with POTS treated in an open-label trial of ivabradine experienced symptom improvement.[79][80][78]
Pyridostigmine has been reported to restrain heart rate and improve chronic symptoms in approximately half of people.[48]
The selective alpha-1 agonist phenylephrine has been used successfully to enhance venous return and stroke volume in some people with POTS.[81] However, this medication may be hampered by poor oral bioavailability.[82]
| Subtypes | Action | Goal | Medication |
|---|---|---|---|
| Neuropathic | Alpha-1 adrenergic receptor agonist | Constrict the peripheral blood vessels aiding venous return. | Midodrine[83][84][85][86] |
| Splanchnic–mesenteric vasoconstriction | Splanchnic vasoconstriction | Octreotide[87][88] | |
| Hypovolemic | Synthetic mineralocorticoid | Forces the body to retain salt. Increase blood volume | Fludrocortisone (Florinef)[89][90] |
| Vasopressin receptor agonist | Helps retain water, Increase blood volume | Desmopressin (DDAVP) [91] | |
| Hyperadrenergic | beta-blockers (Non-Selective) | Decrease sympathetic tone and heart rate. | Propranolol (Inderal)[92][93][94] |
| beta-blockers (Selective) | Metoprolol (Toprol),[84][95] Bisoprolol[96][89] | ||
| Selective sinus node blockade | Directly reducing tachycardia. | Ivabradine[79][80][97][98][99] | |
| alpha-2 adrenergic receptor agonist | Decreases blood pressure and sympathetic nerve traffic. | Clonidine,[48] methyldopa[48] | |
| Anticholinesterase inhibitors | Splanchnic vasoconstriction. Increase blood pressure. | Pyridostigmine[100][101][102] | |
| Other (refractory) | Psychostimulant | Improve cognitive symptoms (Brain Fog) | Modafinil[103][104] |
| Central nervous system stimulant | Tighten blood vessels. Increases alertness and improves brain fog. | Methylphenidate (Ritalin, Concerta)[105] | |
| Direct and indirect α1-adrenoreceptor agonist. | Increased blood flows | Ephedrine and pseudoephedrine[106] | |
| Norepinephrine precursor | Improve blood vessel contraction | Droxidopa (Northera)[106][107] | |
| Alpha-2 adrenergic antagonist | Increase blood pressure | Yohimbine[108] |
Prognosis
POTS has a favorable prognosis when managed appropriately.[10] Symptoms improve within five years of diagnosis for many patients, and 60% return to their original level of functioning.[10] Approximately 90% of people with POTS respond to a combination of pharmacological and physical treatments.[47] Those who develop POTS in their early to mid teens during a period of rapid growth will most likely see complete symptom resolution in two to five years.[109] Outcomes are more guarded for adults newly diagnosed with POTS.[33] Some people do not recover, and a few even worsen with time.[47] The hyperadrenergic type of POTS typically requires continuous therapy.[47] If POTS is caused by another condition, outcomes depend on the prognosis of the underlying disorder.[47]
Epidemiology
The prevalence of POTS is unknown.[10] One study estimated a minimal rate of 170 POTS cases per 100,000 individuals, but the true prevalence is likely higher due to underdiagnosis.[10] Another study estimated that there are at least 500,000 cases in the United States.[110] POTS is more common in women than men, with a female-to-male ratio of 4:1.[68][111] Most people with POTS are aged between 20 and 40, with an average onset of 21.[31][68] Diagnoses of POTS beyond age 40 are rare, perhaps because symptoms improve with age.[10]
History
In 1871, physician Jacob Mendes Da Costa described a condition that resembled the modern concept of POTS. He named it irritable heart syndrome.[10] Cardiologist Thomas Lewis expanded on the description, coining the term soldier's heart because it was often found among military personnel.[10] The condition came to be known as Da Costa syndrome,[10] which is now recognized as several distinct disorders, including POTS.[citation needed]
Postural tachycardia syndrome was coined in 1982 in a description of a patient who had postural tachycardia, but not orthostatic hypotension.[10] Ronald Schondorf and Phillip A. Low of the Mayo Clinic first used the name postural orthostatic tachycardia syndrome, POTS, in 1993.[10][112]
Notable cases
British politician The Baroness Blackwood of North Oxford revealed in March 2015 that she had been diagnosed with Ehlers–Danlos syndrome in 2013 and that she had later been diagnosed with POTS.[113] She was appointed Parliamentary Under-Secretary of State for Life Science by Prime Minister Theresa May in 2019 and given a life peerage which enabled her to take a seat in Parliament. As a junior minister, it is her responsibility to answer questions in parliament on the subjects of Health and departmental business. When answering these questions, it is customary for ministers to sit when listening to the question and then to rise to give an answer from the despatch box, thus standing up and sitting down numerous times in quick succession throughout a series of questions. On 17th June 2019, she fainted during one of these questioning sessions after standing up from a sitting position four times in the space of twelve minutes,[114] and it was suggested that her POTS was a factor in her fainting. Asked about the incident, she stated: "I was frustrated and embarrassed my body gave up on me at work...But I am grateful it gives me a chance to shine a light on a condition many others are also living with."[115]
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 Benarroch EE (December 2012). "Postural tachycardia syndrome: a heterogeneous and multifactorial disorder". Mayo Clinic Proceedings. 87 (12): 1214–25. doi:10.1016/j.mayocp.2012.08.013. PMC 3547546. PMID 23122672.
- ↑ Lawrence, Ruth A.; Lawrence, Robert M. (2010). Breastfeeding E-Book: A Guide for the Medical Professional. Elsevier Health Sciences. p. 580. ISBN 9781437735901. Archived from the original on 2019-03-07. Retrieved 2020-06-08.
- ↑ 3.0 3.1 Ferri, Fred F. (2016). Ferri's Clinical Advisor 2017 E-Book: 5 Books in 1. Elsevier Health Sciences. p. 1019.e2. ISBN 9780323448383. Archived from the original on 2020-07-06. Retrieved 2020-06-08.
- ↑ 4.0 4.1 4.2 4.3 Bogle, JM; Goodman, BP; Barrs, DM (May 2017). "Postural orthostatic tachycardia syndrome for the otolaryngologist". The Laryngoscope. 127 (5): 1195–1198. doi:10.1002/lary.26269. PMID 27578452.
- ↑ 5.0 5.1 5.2 5.3 Grubb BP (May 2008). "Postural tachycardia syndrome". Circulation. 117 (21): 2814–7. doi:10.1161/CIRCULATIONAHA.107.761643. PMID 18506020.
- ↑ Kizilbash, SJ; Ahrens, SP; Bruce, BK; Chelimsky, G; Driscoll, SW; Harbeck-Weber, C; Lloyd, RM; Mack, KJ; Nelson, DE; Ninis, N; Pianosi, PT; Stewart, JM; Weiss, KE; Fischer, PR (2014). "Adolescent fatigue, POTS, and recovery: a guide for clinicians". Current Problems in Pediatric and Adolescent Health Care. 44 (5): 108–33. doi:10.1016/j.cppeds.2013.12.014. PMC 5819886. PMID 24819031.
- ↑ 7.00 7.01 7.02 7.03 7.04 7.05 7.06 7.07 7.08 7.09 7.10 7.11 Benarroch EE (December 2012). "Postural tachycardia syndrome: a heterogeneous and multifactorial disorder". Mayo Clinic Proceedings. 87 (12): 1214–25. doi:10.1016/j.mayocp.2012.08.013. PMC 3547546. PMID 23122672.
- ↑ 8.00 8.01 8.02 8.03 8.04 8.05 8.06 8.07 8.08 8.09 8.10 8.11 8.12 8.13 8.14 Mar PL, Raj SR (2014). "Neuronal and hormonal perturbations in postural tachycardia syndrome". Frontiers in Physiology. 5: 220. doi:10.3389/fphys.2014.00220. PMC 4059278. PMID 24982638.
- ↑ 9.0 9.1 9.2 9.3 Freeman R, Wieling W, Axelrod FB, Benditt DG, Benarroch E, Biaggioni I, et al. (April 2011). "Consensus statement on the definition of orthostatic hypotension, neurally mediated syncope and the postural tachycardia syndrome". Clinical Autonomic Research. 21 (2): 69–72. doi:10.1007/s10286-011-0119-5. PMID 21431947. S2CID 11628648.
- ↑ 10.00 10.01 10.02 10.03 10.04 10.05 10.06 10.07 10.08 10.09 10.10 10.11 10.12 10.13 10.14 10.15 10.16 10.17 10.18 10.19 10.20 10.21 10.22 10.23 10.24 10.25 10.26 10.27 10.28 10.29 10.30 10.31 10.32 Mathias CJ, Low DA, Iodice V, Owens AP, Kirbis M, Grahame R (December 2011). "Postural tachycardia syndrome--current experience and concepts". Nature Reviews. Neurology. 8 (1): 22–34. doi:10.1038/nrneurol.2011.187. PMID 22143364. S2CID 26947896.
- ↑ Abou-Diab J, Moubayed D, Taddeo D, Jamoulle O, Stheneur C (2018-04-24). "Acrocyanosis Presentation in Postural Orthostatic Tachycardia Syndrome". International Journal of Clinical Pediatrics. 7 (1–2): 13–16. doi:10.14740/ijcp293w.
- ↑ 12.0 12.1 12.2 Raj SR (April 2006). "The Postural Tachycardia Syndrome (POTS): pathophysiology, diagnosis & management". Indian Pacing and Electrophysiology Journal. 6 (2): 84–99. PMC 1501099. PMID 16943900.
- ↑ Mallien J, Isenmann S, Mrazek A, Haensch CA (2014-07-07). "Sleep disturbances and autonomic dysfunction in patients with postural orthostatic tachycardia syndrome". Frontiers in Neurology. 5: 118. doi:10.3389/fneur.2014.00118. PMC 4083342. PMID 25071706.
- ↑ Bagai K, Song Y, Ling JF, Malow B, Black BK, Biaggioni I, et al. (April 2011). "Sleep disturbances and diminished quality of life in postural tachycardia syndrome". Journal of Clinical Sleep Medicine. 7 (2): 204–10. doi:10.5664/jcsm.28110. PMC 3077350. PMID 21509337.
- ↑ Haensch CA, Mallien J, Isenmann S (2012-04-25). "Sleep Disturbances in Postural Orthostatic Tachycardia Syndrome (POTS): A Polysomnographic and Questionnaires Based Study (P05.206)". Neurology. 78 (1 Supplement): P05.206. doi:10.1212/WNL.78.1_MeetingAbstracts.P05.206. Archived from the original on 2021-11-10. Retrieved 2022-02-22.
- ↑ Pederson CL, Blettner Brook J (2017-04-12). "Sleep disturbance linked to suicidal ideation in postural orthostatic tachycardia syndrome". Nature and Science of Sleep. 9: 109–115. doi:10.2147/nss.s128513. PMC 5396946. PMID 28442939.
- ↑ "POTS: Causes, Symptoms, Diagnosis & Treatment". Cleveland Clinic. Archived from the original on 2021-11-12. Retrieved 2020-04-04.
- ↑ Wells R, Paterson F, Bacchi S, Page A, Baumert M, Lau DH (June 2020). "Brain fog in postural tachycardia syndrome: An objective cerebral blood flow and neurocognitive analysis". Journal of Arrhythmia. 36 (3): 549–552. doi:10.1002/joa3.12325. PMC 7280003. PMID 32528589.
- ↑ Ross AJ, Medow MS, Rowe PC, Stewart JM (December 2013). "What is brain fog? An evaluation of the symptom in postural tachycardia syndrome". Clinical Autonomic Research. 23 (6): 305–11. doi:10.1007/s10286-013-0212-z. PMC 3896080. PMID 23999934.
- ↑ Raj V, Opie M, Arnold AC (December 2018). "Cognitive and psychological issues in postural tachycardia syndrome". Autonomic Neuroscience. 215: 46–55. doi:10.1016/j.autneu.2018.03.004. PMC 6160364. PMID 29628432.
- ↑ Arnold AC, Haman K, Garland EM, Raj V, Dupont WD, Biaggioni I, et al. (January 2015). "Cognitive dysfunction in postural tachycardia syndrome". Clinical Science. 128 (1): 39–45. doi:10.1042/CS20140251. PMC 4161607. PMID 25001527.
- ↑ Anderson JW, Lambert EA, Sari CI, Dawood T, Esler MD, Vaddadi G, Lambert GW (2014). "Cognitive function, health-related quality of life, and symptoms of depression and anxiety sensitivity are impaired in patients with the postural orthostatic tachycardia syndrome (POTS)". Frontiers in Physiology. 5: 230. doi:10.3389/fphys.2014.00230. PMC 4070177. PMID 25009504.
- ↑ Low PA, Novak V, Spies JM, Novak P, Petty GW (1999). "Cerebrovascular Regulation in the Postural Orthostatic Tachycardia Syndrome (POTS)". The American Journal of the Medical Sciences. 317 (2): 124–133. doi:10.1016/s0002-9629(15)40486-0. ISSN 0002-9629. PMID 10037116.
- ↑ Novak P (2016). "Cerebral Blood Flow, Heart Rate, and Blood Pressure Patterns during the Tilt Test in Common Orthostatic Syndromes". Neuroscience Journal. 2016: 6127340. doi:10.1155/2016/6127340. PMC 4972931. PMID 27525257.
- ↑ Ocon AJ, Medow MS, Taneja I, Clarke D, Stewart JM (August 2009). "Decreased upright cerebral blood flow and cerebral autoregulation in normocapnic postural tachycardia syndrome". American Journal of Physiology. Heart and Circulatory Physiology. 297 (2): H664-73. doi:10.1152/ajpheart.00138.2009. PMC 2724195. PMID 19502561.
- ↑ 26.0 26.1 Owens AP, Low DA, Critchley HD, Mathias CJ (July 2018). "Emotional orienting during interoceptive threat in orthostatic intolerance: Dysautonomic contributions to psychological symptomatology in the postural tachycardia syndrome and vasovagal syncope" (PDF). Autonomic Neuroscience. 212: 42–47. doi:10.1016/j.autneu.2018.01.004. PMID 29519640. S2CID 3819068. Archived (PDF) from the original on 2020-11-13. Retrieved 2022-02-22.
- ↑ den Ouden HE, Kok P, de Lange FP (2012). "How prediction errors shape perception, attention, and motivation". Frontiers in Psychology. 3: 548. doi:10.3389/fpsyg.2012.00548. PMC 3518876. PMID 23248610.
- ↑ Owens AP, Low DA, Iodice V, Critchley HD, Mathias CJ (March 2017). "The genesis and presentation of anxiety in disorders of autonomic overexcitation" (PDF). Autonomic Neuroscience. 203: 81–87. doi:10.1016/j.autneu.2016.10.004. PMID 27865628. S2CID 24913175. Archived (PDF) from the original on 2021-07-20. Retrieved 2022-02-22.
- ↑ Owens AP, Allen M, Ondobaka S, Friston KJ (July 2018). "Interoceptive inference: From computational neuroscience to clinic". Neuroscience and Biobehavioral Reviews. 90: 174–183. doi:10.1016/j.neubiorev.2018.04.017. PMID 29694845. S2CID 19089564. Archived from the original on 2022-02-23. Retrieved 2022-02-22.
- ↑ Eccles JA, Owens AP, Mathias CJ, Umeda S, Critchley HD (2015). "Neurovisceral phenotypes in the expression of psychiatric symptoms". Frontiers in Neuroscience. 9: 4. doi:10.3389/fnins.2015.00004. PMC 4322642. PMID 25713509.
- ↑ 31.0 31.1 31.2 31.3 Shaw BH, Stiles LE, Bourne K, Green EA, Shibao CA, Okamoto LE, et al. (October 2019). "The face of postural tachycardia syndrome - insights from a large cross-sectional online community-based survey". Journal of Internal Medicine. 286 (4): 438–448. doi:10.1111/joim.12895. PMC 6790699. PMID 30861229.
- ↑ "Most common conditions reported with POTS based on the experiences of 1,227 diagnosed members of the POTS research community". Stuff That Works. Archived from the original on 2022-02-23. Retrieved 2022-02-22.
- ↑ 33.0 33.1 33.2 Johnson JN, Mack KJ, Kuntz NL, Brands CK, Porter CJ, Fischer PR (February 2010). "Postural orthostatic tachycardia syndrome: a clinical review". Pediatric Neurology. 42 (2): 77–85. doi:10.1016/j.pediatrneurol.2009.07.002. PMID 20117742.
- ↑ Kavi L, Gammage MD, Grubb BP, Karabin BL (June 2012). "Postural tachycardia syndrome: multiple symptoms, but easily missed". The British Journal of General Practice. 62 (599): 286–7. doi:10.3399/bjgp12X648963. PMC 3361090. PMID 22687203.
- ↑ 35.0 35.1 Kanjwal K, Saeed B, Karabin B, Kanjwal Y, Grubb BP (2011). "Clinical presentation and management of patients with hyperadrenergic postural orthostatic tachycardia syndrome. A single center experience". Cardiology Journal. 18 (5): 527–31. doi:10.5603/cj.2011.0008. PMID 21947988.
- ↑ 36.0 36.1 36.2 36.3 Vernino S, Stiles LE (December 2018). "Autoimmunity in postural orthostatic tachycardia syndrome: Current understanding". Autonomic Neuroscience. Postural Orthostatic Tachycardia Syndrome (POTS). 215: 78–82. doi:10.1016/j.autneu.2018.04.005. PMID 29909990.
- ↑ Fedorowski A (April 2019). "Postural orthostatic tachycardia syndrome: clinical presentation, aetiology and management". Journal of Internal Medicine. 285 (4): 352–366. doi:10.1111/joim.12852. PMID 30372565.
- ↑ Wilson RG (November 4, 2015). "Understanding POTS, Syncope and Other Autonomic Disorders". Cleveland Clinic. Archived from the original on January 17, 2021. Retrieved February 22, 2022.
- ↑ Fedorowski A, Li H, Yu X, Koelsch KA, Harris VM, Liles C, et al. (July 2017). "Antiadrenergic autoimmunity in postural tachycardia syndrome". Europace. 19 (7): 1211–1219. doi:10.1093/europace/euw154. PMC 5834103. PMID 27702852.
- ↑ Dahan S, Tomljenovic L, Shoenfeld Y (April 2016). "Postural Orthostatic Tachycardia Syndrome (POTS)--A novel member of the autoimmune family". Lupus. 25 (4): 339–42. doi:10.1177/0961203316629558. PMID 26846691.
- ↑ Miller AJ, Doherty TA (October 2019). "Hop to It: The First Animal Model of Autoimmune Postural Orthostatic Tachycardia Syndrome". Journal of the American Heart Association. 8 (19): e014084. doi:10.1161/JAHA.119.014084. PMC 6806054. PMID 31547756.
- ↑ Li H, Zhang G, Zhou L, Nuss Z, Beel M, Hines B, et al. (October 2019). "Adrenergic Autoantibody-Induced Postural Tachycardia Syndrome in Rabbits". Journal of the American Heart Association. 8 (19): e013006. doi:10.1161/JAHA.119.013006. PMC 6806023. PMID 31547749.
- ↑ Miglis MG, Muppidi S (February 2020). "Is postural tachycardia syndrome an autoimmune disorder? And other updates on recent autonomic research". Clinical Autonomic Research. 30 (1): 3–5. doi:10.1007/s10286-019-00661-5. PMID 31938977.
- ↑ 44.0 44.1 44.2 Kharraziha I, Axelsson J, Ricci F, Di Martino G, Persson M, Sutton R, et al. (August 2020). "Serum Activity Against G Protein-Coupled Receptors and Severity of Orthostatic Symptoms in Postural Orthostatic Tachycardia Syndrome". Journal of the American Heart Association. 9 (15): e015989. doi:10.1161/JAHA.120.015989. PMC 7792263. PMID 32750291.
- ↑ Gunning WT, Kvale H, Kramer PM, Karabin BL, Grubb BP (September 2019). "Postural Orthostatic Tachycardia Syndrome Is Associated With Elevated G-Protein Coupled Receptor Autoantibodies". Journal of the American Heart Association. 8 (18): e013602. doi:10.1161/JAHA.119.013602. PMC 6818019. PMID 31495251.
- ↑ Gunning WT, Stepkowski SM, Kramer PM, Karabin BL, Grubb BP (February 2021). "Inflammatory Biomarkers in Postural Orthostatic Tachycardia Syndrome with Elevated G-Protein-Coupled Receptor Autoantibodies". Journal of Clinical Medicine. 10 (4): 623. doi:10.3390/jcm10040623. PMC 7914580. PMID 33562074.
- ↑ 47.0 47.1 47.2 47.3 47.4 47.5 47.6 Grubb BP (May 2008). "Postural tachycardia syndrome". Circulation. 117 (21): 2814–7. doi:10.1161/CIRCULATIONAHA.107.761643. PMID 18506020.
- ↑ 48.0 48.1 48.2 48.3 48.4 48.5 48.6 48.7 Raj SR (June 2013). "Postural tachycardia syndrome (POTS)". Circulation. 127 (23): 2336–42. doi:10.1161/CIRCULATIONAHA.112.144501. PMC 3756553. PMID 23753844.
- ↑ Bonamichi-Santos R, Yoshimi-Kanamori K, Giavina-Bianchi P, Aun MV (August 2018). "Association of Postural Tachycardia Syndrome and Ehlers-Danlos Syndrome with Mast Cell Activation Disorders". Immunology and Allergy Clinics of North America. Mastocytosis. 38 (3): 497–504. doi:10.1016/j.iac.2018.04.004. PMID 30007466.
- ↑ Cheung I, Vadas P (2015). "A New Disease Cluster: Mast Cell Activation Syndrome, Postural Orthostatic Tachycardia Syndrome, and Ehlers-Danlos Syndrome". Journal of Allergy and Clinical Immunology. 135 (2): AB65. doi:10.1016/j.jaci.2014.12.1146.
- ↑ Kohn A, Chang C (June 2020). "The Relationship Between Hypermobile Ehlers-Danlos Syndrome (hEDS), Postural Orthostatic Tachycardia Syndrome (POTS), and Mast Cell Activation Syndrome (MCAS)". Clinical Reviews in Allergy & Immunology. 58 (3): 273–297. doi:10.1007/s12016-019-08755-8. PMID 31267471. S2CID 195787615.
- ↑ Chang AR, Vadas P (2019). "Prevalence of Symptoms of Mast Cell Activation in Patients with Postural Orthostatic Tachycardia Syndrome and Hypermobile Ehlers-Danlos Syndrome". Journal of Allergy and Clinical Immunology. 143 (2): AB182. doi:10.1016/j.jaci.2018.12.558.
- ↑ 53.0 53.1 53.2 Carew S, Connor MO, Cooke J, Conway R, Sheehy C, Costelloe A, Lyons D (January 2009). "A review of postural orthostatic tachycardia syndrome". Europace. 11 (1): 18–25. doi:10.1093/europace/eun324. PMID 19088364.
- ↑ Dipaola F, Barberi C, Castelnuovo E, Minonzio M, Fornerone R, Shiffer D, et al. (August 2020). "Time Course of Autonomic Symptoms in Postural Orthostatic Tachycardia Syndrome (POTS) Patients: Two-Year Follow-Up Results". International Journal of Environmental Research and Public Health. 17 (16): 5872. doi:10.3390/ijerph17165872. PMC 7460485. PMID 32823577.
- ↑ McKeon A, Lennon VA, Lachance DH, Fealey RD, Pittock SJ (June 2009). "Ganglionic acetylcholine receptor autoantibody: oncological, neurological, and serological accompaniments". Archives of Neurology. 66 (6): 735–41. doi:10.1001/archneurol.2009.78. PMC 3764484. PMID 19506133.
- ↑ Blitshteyn S, Whitelaw S (March 2021). "Postural orthostatic tachycardia syndrome (POTS) and other autonomic disorders after COVID-19 infection: a case series of 20 patients". Immunologic Research. 69 (2): 205–211. doi:10.1007/s12026-021-09185-5. PMC 8009458. PMID 33786700.
- ↑ Miglis MG, Prieto T, Shaik R, Muppidi S, Sinn DI, Jaradeh S (October 2020). "A case report of postural tachycardia syndrome after COVID-19". Clinical Autonomic Research. 30 (5): 449–451. doi:10.1007/s10286-020-00727-9. PMC 7471493. PMID 32880754.
- ↑ Davido B, Seang S, Barizien N, Tubiana R, de Truchis P (March 2021). "'Post-COVID-19 chronic symptoms' - Author's reply". Clinical Microbiology and Infection. 27 (3): 495–496. doi:10.1016/j.cmi.2020.09.001. PMC 7474820. PMID 32898714.
- ↑ Yong E (2020-09-21). "The Core Lesson of the COVID-19 Heart Debate". The Atlantic. Archived from the original on 2020-09-22. Retrieved 2020-09-22.
Some long-haulers have been diagnosed with dysautonomia—a group of disorders that disrupt involuntary bodily functions, including heartbeats (which can become inexplicably fast) and blood pressure (which can suddenly crash).
- ↑ Prior R. "Months after Covid-19 infection, patients report breathing difficulty and fatigue". CNN. Archived from the original on 2020-09-26. Retrieved 2020-09-22.
Gahan and others with long-haul Covid-19 symptoms face a condition called postural orthostatic tachycardia syndrome, which refers to a sharp rise in heart rate that occurs when moving from a reclining to standing position. The pull of gravity causes blood to pool in the legs. This condition can cause dizziness, lightheadedness and fainting.
- ↑ Eshak N, Abdelnabi M, Ball S, Elgwairi E, Creed K, Test V, Nugent K (October 2020). "Dysautonomia: An Overlooked Neurological Manifestation in a Critically ill COVID-19 Patient". The American Journal of the Medical Sciences. 360 (4): 427–429. doi:10.1016/j.amjms.2020.07.022. PMC 7366085. PMID 32739039.
- ↑ Jensen L (2020-08-11). "Can Your Long-haul Covid-19 Symptoms be Explained by Dysautonomia?". Medium. Archived from the original on 2020-10-02. Retrieved 2020-09-23.
- ↑ Du L, Ring S (24 August 2020). "Debilitating Covid-19 Effects and Economic Costs May Linger for Years". www.bloomberg.com. Archived from the original on 2021-03-07. Retrieved 2022-02-22.
He was recently diagnosed with postural orthostatic tachycardia syndrome -- a problem with the autonomic nervous system. The condition, which may develop after a viral illness, often causes heart palpitations, chest pain and brain fog, according to the Cleveland Clinic.
- ↑ Morley JE (2020-10-05). "Editorial: COVID-19 - The Long Road to Recovery". The Journal of Nutrition, Health & Aging. 24 (9): 917–919. doi:10.1007/s12603-020-1473-6. PMC 7533666. PMID 33155615.
- ↑ Parker William; Moudgil Rohit; Singh Tamanna (2021-05-11). "Postural orthostatic tachycardia syndrome in six patients following covid-19 infection". Journal of the American College of Cardiology. 77 (18_Supplement_1): 3163. doi:10.1016/S0735-1097(21)04518-6. PMC 8091396.
- ↑ "COVID-19 and POTS: What You Should Know". WebMD. Archived from the original on 2021-07-31. Retrieved 2021-07-31.
- ↑ Garland EM, Celedonio JE, Raj SR (September 2015). "Postural Tachycardia Syndrome: Beyond Orthostatic Intolerance". Current Neurology and Neuroscience Reports. 15 (9): 60. doi:10.1007/s11910-015-0583-8. PMC 4664448. PMID 26198889.
- ↑ 68.0 68.1 68.2 68.3 68.4 Low PA, Sandroni P, Joyner M, Shen WK (March 2009). "Postural tachycardia syndrome (POTS)". Journal of Cardiovascular Electrophysiology. 20 (3): 352–8. doi:10.1111/j.1540-8167.2008.01407.x. PMC 3904426. PMID 19207771.
- ↑ 69.0 69.1 Jacob G, Shannon JR, Costa F, Furlan R, Biaggioni I, Mosqueda-Garcia R, et al. (April 1999). "Abnormal norepinephrine clearance and adrenergic receptor sensitivity in idiopathic orthostatic intolerance". Circulation. 99 (13): 1706–12. doi:10.1161/01.CIR.99.13.1706. PMID 10190880.
- ↑ Jacob G, Costa F, Shannon JR, Robertson RM, Wathen M, Stein M, et al. (October 2000). "The neuropathic postural tachycardia syndrome". The New England Journal of Medicine. 343 (14): 1008–14. doi:10.1056/NEJM200010053431404. PMID 11018167.
- ↑ Lambert E, Lambert GW (2014). "Sympathetic dysfunction in vasovagal syncope and the postural orthostatic tachycardia syndrome". Frontiers in Physiology. 5: 280. doi:10.3389/fphys.2014.00280. PMC 4112787. PMID 25120493.
- ↑ Zhang Q, Chen X, Li J, Du J (December 2014). "Clinical features of hyperadrenergic postural tachycardia syndrome in children". Pediatrics International. 56 (6): 813–816. doi:10.1111/ped.12392. PMID 24862636. S2CID 20740649.
- ↑ Crnošija L, Krbot Skorić M, Adamec I, Lovrić M, Junaković A, Mišmaš A, et al. (February 2016). "Hemodynamic profile and heart rate variability in hyperadrenergic versus non-hyperadrenergic postural orthostatic tachycardia syndrome". Clinical Neurophysiology. 127 (2): 1639–1644. doi:10.1016/j.clinph.2015.08.015. PMID 26386646. S2CID 6008891.
- ↑ Sandroni P, Opfer-Gehrking TL, McPhee BR, Low PA (November 1999). "Postural tachycardia syndrome: clinical features and follow-up study". Mayo Clinic Proceedings. 74 (11): 1106–10. doi:10.4065/74.11.1106. PMID 10560597.
- ↑ 75.0 75.1 Grubb BP, Kanjwal Y, Kosinski DJ (January 2006). "The postural tachycardia syndrome: a concise guide to diagnosis and management". Journal of Cardiovascular Electrophysiology. 17 (1): 108–12. doi:10.1111/j.1540-8167.2005.00318.x. PMID 16426415. S2CID 38915192.
- ↑ Deng W, Liu Y, Liu AD, Holmberg L, Ochs T, Li X, et al. (April 2014). "Difference between supine and upright blood pressure associates to the efficacy of midodrine on postural orthostatic tachycardia syndrome (POTS) in children". Pediatric Cardiology. 35 (4): 719–25. doi:10.1007/s00246-013-0843-9. PMID 24253613. S2CID 105235.
- ↑ Nogués M, Delorme R, Saadia D, Heidel K, Benarroch E (August 2001). "Postural tachycardia syndrome in syringomyelia: response to fludrocortisone and beta-blockers". Clinical Autonomic Research. 11 (4): 265–7. doi:10.1007/BF02298959. PMID 11710800. S2CID 9596669.
- ↑ 78.0 78.1 78.2 78.3 78.4 "2015 Heart Rhythm Society Expert Consensus Statement on the Diagnosis and Treatment of Postural Tachycardia Syndrome, Inappropriate Sinus Tachycardia, and Vasovagal Syncope". Archived from the original on 2017-03-03. Retrieved 2017-03-03.
- ↑ 79.0 79.1 McDonald C, Frith J, Newton JL (March 2011). "Single centre experience of ivabradine in postural orthostatic tachycardia syndrome". Europace. 13 (3): 427–30. doi:10.1093/europace/euq390. PMC 3043639. PMID 21062792.
- ↑ 80.0 80.1 Tahir F, Bin Arif T, Majid Z, Ahmed J, Khalid M (April 2020). "Ivabradine in Postural Orthostatic Tachycardia Syndrome: A Review of the Literature". Cureus. 12 (4): e7868. doi:10.7759/cureus.7868. PMC 7255540. PMID 32489723.
- ↑ "Archived copy" (PDF). Archived (PDF) from the original on 2017-03-03. Retrieved 2017-03-03.
{{cite web}}: CS1 maint: archived copy as title (link) - ↑ "Archived copy". Archived from the original on 2017-03-03. Retrieved 2017-03-03.
{{cite web}}: CS1 maint: archived copy as title (link) - ↑ Chen L, Wang L, Sun J, Qin J, Tang C, Jin H, Du J (2011). "Midodrine hydrochloride is effective in the treatment of children with postural orthostatic tachycardia syndrome". Circulation Journal. 75 (4): 927–31. doi:10.1253/circj.CJ-10-0514. PMID 21301135.
- ↑ 84.0 84.1 Lai CC, Fischer PR, Brands CK, Fisher JL, Porter CB, Driscoll SW, Graner KK (February 2009). "Outcomes in adolescents with postural orthostatic tachycardia syndrome treated with midodrine and beta-blockers". Pacing and Clinical Electrophysiology. 32 (2): 234–8. doi:10.1111/j.1540-8159.2008.02207.x. PMID 19170913. S2CID 611824.
- ↑ Yang J, Liao Y, Zhang F, Chen L, Junbao DU, Jin H (2014-01-01). "The follow-up study on the treatment of children with postural orthostatic tachycardia syndrome". International Journal of Pediatrics (in 中文). 41 (1): 76–79. ISSN 1673-4408. Archived from the original on 2022-02-23. Retrieved 2022-02-22.
- ↑ Chen L, Du JB, Jin HF, Zhang QY, Li WZ, Wang L, Wang YL (September 2008). "[Effect of selective alpha1 receptor agonist in the treatment of children with postural orthostatic tachycardia syndrome]". Zhonghua Er Ke Za Zhi = Chinese Journal of Pediatrics. 46 (9): 688–91. PMID 19099860.
- ↑ Khan M, Ouyang J, Perkins K, Somauroo J, Joseph F (2015). "Treatment of Refractory Postural Tachycardia Syndrome with Subcutaneous Octreotide Delivered Using an Insulin Pump". Case Reports in Medicine. 2015: 545029. doi:10.1155/2015/545029. PMC 4452321. PMID 26089909.
- ↑ Hoeldtke RD, Bryner KD, Hoeldtke ME, Hobbs G (December 2006). "Treatment of postural tachycardia syndrome: a comparison of octreotide and midodrine". Clinical Autonomic Research. 16 (6): 390–5. doi:10.1007/s10286-006-0373-0. PMID 17036177. S2CID 22288783.
The two drugs had similar potencies; combination therapy was not significantly better than monotherapy.
- ↑ 89.0 89.1 Freitas J, Santos R, Azevedo E, Costa O, Carvalho M, de Freitas AF (October 2000). "Clinical improvement in patients with orthostatic intolerance after treatment with bisoprolol and fludrocortisone". Clinical Autonomic Research. 10 (5): 293–9. doi:10.1007/BF02281112. PMID 11198485. S2CID 20843222.
- ↑ Postural tachycardia syndrome : a concise and practical guide to management and associated conditions. Nicholas Gall, Lesley Kavi, Melvin D. Lobo. Cham: Springer. 2021. pp. 229–230. ISBN 978-3-030-54165-1. OCLC 1204143485. Archived from the original on 2022-02-23. Retrieved 2022-02-22.
{{cite book}}: CS1 maint: others (link) - ↑ Coffin ST, Black BK, Biaggioni I, Paranjape SY, Orozco C, Black PW, et al. (September 2012). "Desmopressin acutely decreases tachycardia and improves symptoms in the postural tachycardia syndrome". Heart Rhythm. 9 (9): 1484–90. doi:10.1016/j.hrthm.2012.05.002. PMC 3419341. PMID 22561596.
- ↑ Fu Q, Vangundy TB, Shibata S, Auchus RJ, Williams GH, Levine BD (August 2011). "Exercise training versus propranolol in the treatment of the postural orthostatic tachycardia syndrome". Hypertension. 58 (2): 167–75. doi:10.1161/HYPERTENSIONAHA.111.172262. PMC 3142863. PMID 21690484.
- ↑ Arnold AC, Okamoto LE, Diedrich A, Paranjape SY, Raj SR, Biaggioni I, Gamboa A (May 2013). "Low-dose propranolol and exercise capacity in postural tachycardia syndrome: a randomized study". Neurology. 80 (21): 1927–33. doi:10.1212/WNL.0b013e318293e310. PMC 3716342. PMID 23616163.
- ↑ Raj SR, Black BK, Biaggioni I, Paranjape SY, Ramirez M, Dupont WD, Robertson D (September 2009). "Propranolol decreases tachycardia and improves symptoms in the postural tachycardia syndrome: less is more". Circulation. 120 (9): 725–34. doi:10.1161/CIRCULATIONAHA.108.846501. PMC 2758650. PMID 19687359.
- ↑ Chen L, Du JB, Zhang QY, Wang C, Du ZD, Wang HW, et al. (December 2007). "[A multicenter study on treatment of autonomous nerve-mediated syncope in children with beta-receptor blocker]". Zhonghua Er Ke Za Zhi = Chinese Journal of Pediatrics. 45 (12): 885–8. PMID 18339272.
- ↑ Moon J, Kim DY, Lee WJ, Lee HS, Lim JA, Kim TJ, et al. (July 2018). "Efficacy of Propranolol, Bisoprolol, and Pyridostigmine for Postural Tachycardia Syndrome: a Randomized Clinical Trial". Neurotherapeutics. 15 (3): 785–795. doi:10.1007/s13311-018-0612-9. PMC 6095784. PMID 29500811.
- ↑ Barzilai M, Jacob G (July 2015). "The Effect of Ivabradine on the Heart Rate and Sympathovagal Balance in Postural Tachycardia Syndrome Patients". Rambam Maimonides Medical Journal. 6 (3): e0028. doi:10.5041/RMMJ.10213. PMC 4524401. PMID 26241226.
- ↑ Hersi AS (August 2010). "Potentially new indication of ivabradine: treatment of a patient with postural orthostatic tachycardia syndrome". The Open Cardiovascular Medicine Journal. 4 (1): 166–7. doi:10.2174/1874192401004010166. PMC 2995161. PMID 21127745.
- ↑ Taub PR, Zadourian A, Lo HC, Ormiston CK, Golshan S, Hsu JC (February 2021). "Randomized Trial of Ivabradine in Patients With Hyperadrenergic Postural Orthostatic Tachycardia Syndrome". Journal of the American College of Cardiology. 77 (7): 861–871. doi:10.1016/j.jacc.2020.12.029. PMID 33602468.
- ↑ Kanjwal K, Karabin B, Sheikh M, Elmer L, Kanjwal Y, Saeed B, Grubb BP (June 2011). "Pyridostigmine in the treatment of postural orthostatic tachycardia: a single-center experience". Pacing and Clinical Electrophysiology. 34 (6): 750–5. doi:10.1111/j.1540-8159.2011.03047.x. PMID 21410722. S2CID 20405336.
- ↑ Raj SR, Black BK, Biaggioni I, Harris PA, Robertson D (May 2005). "Acetylcholinesterase inhibition improves tachycardia in postural tachycardia syndrome". Circulation. 111 (21): 2734–40. doi:10.1161/CIRCULATIONAHA.104.497594. PMID 15911704.
- ↑ Low, Phillip A. "A Study of Pyridostigmine in Postural Tachycardia Syndrome". ClinicalTrials.gov. NCT00409435. Archived from the original on 2020-10-29. Retrieved 2020-10-26.
- ↑ Kpaeyeh J, Mar PL, Raj V, Black BK, Arnold AC, Biaggioni I, et al. (December 2014). "Hemodynamic profiles and tolerability of modafinil in the treatment of postural tachycardia syndrome: a randomized, placebo-controlled trial". Journal of Clinical Psychopharmacology. 34 (6): 738–41. doi:10.1097/JCP.0000000000000221. PMC 4239166. PMID 25222185.
- ↑ Biaggioni, Italo (8 January 2021). "Modafinil and Cognitive Function in POTS". ClinicalTrials.gov. NCT01988883. Archived from the original on 25 April 2021. Retrieved 22 February 2022.
- ↑ Kanjwal K, Saeed B, Karabin B, Kanjwal Y, Grubb BP (January 2012). "Use of methylphenidate in the treatment of patients suffering from refractory postural tachycardia syndrome". American Journal of Therapeutics. 19 (1): 2–6. doi:10.1097/MJT.0b013e3181dd21d2. PMID 20460983. S2CID 11453764.
- ↑ 106.0 106.1 Fedorowski A (2018). Camm AJ, Lüscher TF, Maurer G, Serruys PW (eds.). Orthostatic intolerance: orthostatic hypotension and postural orthostatic tachycardia syndrome. Oxford University Press. doi:10.1093/med/9780198784906.001.0001. ISBN 978-0-19-182714-3.
- ↑ Ruzieh M, Dasa O, Pacenta A, Karabin B, Grubb B (2017). "Droxidopa in the Treatment of Postural Orthostatic Tachycardia Syndrome". American Journal of Therapeutics. 24 (2): e157–e161. doi:10.1097/MJT.0000000000000468. PMID 27563801. S2CID 205808005.
- ↑ Goldstein DS, Smith LJ (2002). NDRF Hans. The National Dysautonomia Research Foundation. Archived from the original on 2021-05-04. Retrieved 2022-02-22.
- ↑ Agarwal AK, Garg R, Ritch A, Sarkar P (July 2007). "Postural orthostatic tachycardia syndrome". Postgraduate Medical Journal. 83 (981): 478–80. doi:10.1136/pgmj.2006.055046. PMC 2600095. PMID 17621618.
- ↑ Bogle JM, Goodman BP, Barrs DM (May 2017). "Postural orthostatic tachycardia syndrome for the otolaryngologist". The Laryngoscope. 127 (5): 1195–1198. doi:10.1002/lary.26269. PMID 27578452. S2CID 24233032.
- ↑ Boris JR, Bernadzikowski T (December 2018). "Utilisation of medications to reduce symptoms in children with postural orthostatic tachycardia syndrome". Cardiology in the Young. 28 (12): 1386–1392. doi:10.1017/S1047951118001373. PMID 30079848. S2CID 51922967.
- ↑ Schondorf R, Low PA (January 1993). "Idiopathic postural orthostatic tachycardia syndrome: an attenuated form of acute pandysautonomia?". Neurology. 43 (1): 132–7. doi:10.1212/WNL.43.1_Part_1.132. PMID 8423877. S2CID 43860206.
- ↑ Rodgers, Keeley (31 March 2015). "Nicola Blackwood: I'm battling a genetic mobility condition EhlersDanlos". Oxford Mail. Archived from the original on 10 April 2021. Retrieved 8 June 2020.
- ↑ https://hansard.parliament.uk/Lords/2019-06-17/debates/0F5AE418-A5F5-4CA8-8B71-2694F6D6EAFB/HospitalsListeria Archived 2020-07-06 at the Wayback Machine Baroness Blackwood of North Oxford makes four speeches (thus standing up four times) between 5:52PM and 6:04PM.
- ↑ "House of Lords collapse 'no big deal'". BBC News. 25 June 2019. Archived from the original on 9 January 2021. Retrieved 25 June 2019.
External links
| Classification |
|---|
- Pages with script errors
- CS1 maint: archived copy as title
- CS1 中文-language sources (zh)
- CS1 maint: others
- Webarchive template wayback links
- All articles with unsourced statements
- Articles with unsourced statements from August 2020
- Articles with invalid date parameter in template
- Articles with unsourced statements from December 2020
- Vascular diseases
- Peripheral nervous system disorders
- Endocrine diseases
- Syndromes
- RTT
- RTTNEURO