Ocular hypotony
| Ocular hypotony | |
|---|---|
| Other names: Ocular hypotension | |
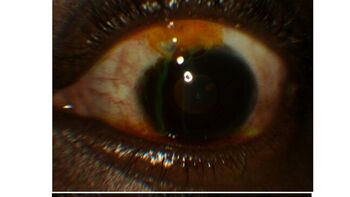 | |
| Seidel test assesses for occurrence of aqueous humor leakage through a defect | |
| Specialty | Ophthalmology |
| Frequency | Lua error in Module:PrevalenceData at line 5: attempt to index field 'wikibase' (a nil value). |
Ocular hypotony, or ocular hypotension, or shortly hypotony, is the medical condition in which intraocular pressure (IOP) of the eye is very low.
Normal IOP ranges between 10–20 mm Hg.[1] The eye is considered hypotonous if the IOP is ≤5 mm Hg (some sources say IOP less than 6.5 mmHg).[2][3]
Types
Ocular hypotony is divided into statistical and clinical types. If intraocular pressure is low (less than 6.5 mm Hg) it is called statistical hypotony, and if the reduced IOP causes a decrease in vision, it is called clinical.[4]
Signs and symptoms
Complications
Decreased IOP may lead to phthisis bulbi.[3] Hypotony maculopathy is another complication caused by very low IOP.[5]
Causes
Hypotony may occur either due to decreased production of aqueous humor or due to increased outflow. Hypotony has many causes including post-surgical wound leak from the eye, chronic inflammation within the eye including iridocyclitis, hypoperfusion, tractional ciliary body detachment or retinal detachment.[6] Eye inflammation, medications including anti glaucoma drugs, or proliferative vitreoretinopathy causes decreased production.[7] Increased outflow or aqueous loss may occur following a glaucoma surgery, trauma, cyclodialysis cleft or retinal detachment.[7]
Diagnosis
In terms of the evaluation of Ocular hypotony we find that the following is done:[8]
- Optical coherence tomography
- Seidel test
- Ultrasound biomicroscopy
Treatment
Treatment of hypotony is depending on the cause of the condition.[7] Chronic ocular hypotony may be treated with intraocular injection of sodium hyaluronate.[9] If the cause of hypotony is an over filtering bleb, cycloplegia using atropine may be used.[2]
References
- ↑ "Eye Pressure". American Academy of Ophthalmology. 19 January 2018. Archived from the original on 4 December 2022. Retrieved 22 November 2022.
- ↑ 2.0 2.1 N.Y, Valerie Trubnik, MD, FACS, Mineola. "Managing Hypotony After Trabeculectomy". www.reviewofophthalmology.com. Archived from the original on 2021-12-07. Retrieved 2022-11-22.
- ↑ 3.0 3.1 Schmack, Ingo; Völcker, Hans E; Grossniklaus, Hans E (1 January 2010). "Chapter 54 - Phthisis bulbi". Ocular Disease. W.B. Saunders. pp. 415–423. ISBN 978-0-7020-2983-7. Archived from the original on 13 April 2022. Retrieved 22 November 2022.
- ↑ Thomas, Merina; Vajaranant, Thasarat S.; Aref, Ahmad A. (December 2015). "Hypotony Maculopathy: Clinical Presentation and Therapeutic Methods". Ophthalmology and Therapy. 4 (2): 79–88. doi:10.1007/s40123-015-0037-z. ISSN 2193-8245. PMC 4675727. PMID 26253854.
- ↑ "Hypotony Maculopathy - EyeWiki". eyewiki.aao.org. Archived from the original on 2022-04-13. Retrieved 2022-11-22.
- ↑ "Ocular Hypotony: Background, Pathophysiology, Epidemiology". 19 July 2021. Archived from the original on 13 April 2022. Retrieved 22 November 2022.
- ↑ 7.0 7.1 7.2 Fine, Howard F.; Biscette, O'neil; Chang, Stanley; Schiff, William M. (January 2007). "Ocular hypotony: a review". Comprehensive Ophthalmology Update. 8 (1): 29–37. ISSN 1527-7313. PMID 17394757. Archived from the original on 2022-04-13. Retrieved 2022-11-22.
- ↑ Okonkwo, Ogugua N.; Tripathy, Koushik (2023). "Ocular Hypotony". StatPearls. StatPearls Publishing. Retrieved 18 August 2023.
- ↑ Küçükerdönmez, C.; Beutel, J.; Bartz-Schmidt, K. U.; Gelisken, F. (1 February 2009). "Treatment of chronic ocular hypotony with intraocular application of sodium hyaluronate". British Journal of Ophthalmology. 93 (2): 235–239. doi:10.1136/bjo.2008.143834. ISSN 0007-1161. PMID 18829633. S2CID 36520175. Archived from the original on 31 January 2023. Retrieved 22 November 2022.