Nephritis
| Nephritis | |
|---|---|
 | |
| Enlarged kidney (anatomy) | |
| Specialty | Nephrology |
| Types | Glomerulonephritis[1] and Interstitial nephritis[2] |
| Diagnostic method | Ultrasound, X-ray[3] |
| Treatment | Depends on type(See type) |
Nephritis is inflammation of the kidneys and may involve the glomeruli, tubules, or interstitial tissue surrounding the glomeruli and tubules.[4] It is one of several different types of nephropathy.
Types
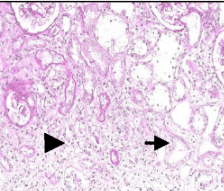
- Glomerulonephritis is inflammation of the glomeruli. Glomerulonephritis is often implied when using the term "nephritis" without qualification.[1]
- Interstitial nephritis (or tubulo-interstitial nephritis) is inflammation of the spaces between renal tubules.[2]
Causes
Nephritis is often caused by infections, and toxins, but is most commonly caused by autoimmune disorders that affect the major organs like kidneys.[5]
- Pyelonephritis is inflammation that results from a urinary tract infection that reaches the renal pelvis of the kidney.[6]
- Lupus nephritis is inflammation of the kidney caused by systemic lupus erythematosus (SLE), a disease of the immune system.[7]
- Athletic nephritis is nephritis resulting from strenuous exercise.[8] Bloody urine after strenuous exercise may also result from march hemoglobinuria, which is caused by trauma to red blood cells, causing their rupture, which leads to the release of hemoglobin into the urine.[9]
Mechanism

Nephritis can produce glomerular injury, by disturbing the glomerular structure with inflammatory cell proliferation.[10] This can lead to reduced glomerular blood flow, leading to reduced urine output (oliguria)[11] and retention of waste products (uremia).[12] As a result, red blood cells may leak out of damaged glomeruli, causing blood to appear in the urine (hematuria).[13]
Low renal blood flow activates the renin–angiotensin–aldosterone system (RAAS), causing fluid retention and mild hypertension.[14] As the kidneys inflame, they begin to excrete needed protein from the affected individual's body into the urine stream. This condition is called proteinuria.[15]
Loss of necessary protein due to nephritis can result in several life-threatening symptoms. The most serious complication of nephritis can occur if there is significant loss of the proteins that keep blood from clotting excessively. Loss of these proteins can result in blood clots, causing sudden stroke.[16]
Diagnosis
The diagnosis depends on the cause of the nephritis, and in the case of lupus nephritis, blood tests, X-rays and an ultrasound can help ascertain if the individual has the condition.[3]
Treatment
Treatment (or management) of nephritis depends on what has provoked the inflammation of the kidney(s). In the case of lupus nephritis, hydroxychloroquine could be used.[17]
Prevalence

Nephritis represents the ninth most common cause of death among all women in the US (and the fifth leading cause among non-Hispanic black women).[19]
Worldwide, the highest rates[clarification needed] of nephritis are 50-55% for African or Asian descent followed by Hispanic at 43% and Caucasian at 17%.[20]
The average age of an individual diagnosed with kidney inflammation (in this case, lupus nephritis) is 28.4 years old.[21]
See also
References
- ↑ 1.0 1.1 "Glomerulonephritis: MedlinePlus Medical Encyclopedia". www.nlm.nih.gov. Archived from the original on 2016-07-05. Retrieved 2015-06-14.
- ↑ 2.0 2.1 "Interstitial nephritis: MedlinePlus Medical Encyclopedia". www.nlm.nih.gov. Archived from the original on 2016-07-05. Retrieved 2015-06-14.
- ↑ 3.0 3.1 "American College of Rheumatology guidelines for screening, treatment, and management of lupus nephritis. | National Guideline Clearinghouse". www.guideline.gov. Archived from the original on 15 September 2016. Retrieved 23 July 2016.
- ↑ Keto Acids – Advances in Research and Application 2013 Edition p.220e
- ↑ "Acute Nephritis; Nephrosis; Nephritic syndrome information. Patient | Patient". Patient. Archived from the original on 12 December 2022. Retrieved 23 July 2016.
- ↑ "Pyelonephritis: Kidney Infection". www.niddk.nih.gov. Archived from the original on 2016-06-11. Retrieved 2015-06-14.
- ↑ "Lupus Nephritis". www.niddk.nih.gov. Archived from the original on 2017-01-04. Retrieved 2015-06-14.
- ↑ "Nephritis Symptoms". esagil.org. Archived from the original on 2018-09-14. Retrieved 2022-10-07.
- ↑ Shinton, N. K. (2007). Desk Reference for Hematology. CRC Press. ISBN 9781420005127. Archived from the original on 2022-12-23. Retrieved 2019-02-14.
- ↑ "Glomerular Diseases". www.niddk.nih.gov. Archived from the original on 2015-06-12. Retrieved 2015-06-15.
- ↑ "Oliguria: Background, Etiology, Epidemiology". Medscape. eMedicine. Archived from the original on 12 December 2022. Retrieved 23 July 2016.
- ↑ "uremia | accumulation in the blood of constituents normally eliminated in the urine that produces a severe toxic condition and usually occurs in severe kidney disease". www.merriam-webster.com. Archived from the original on 2016-02-15. Retrieved 2015-06-14.
- ↑ "Hematuria (Blood in the Urine)". www.niddk.nih.gov. Archived from the original on 2016-06-24. Retrieved 2015-06-14.
- ↑ Ashar, Bimal; Miller, Redonda; Sisson, Stephen; Hospital, Johns Hopkins (2012-02-20). Johns Hopkins Internal Medicine Board Review: Certification and Recertification. Elsevier Health Sciences. ISBN 978-0323087988.
- ↑ "Proteinuria". www.niddk.nih.gov. Archived from the original on 2015-07-05. Retrieved 2015-06-14.
- ↑ Thomas, Donald E. Jr (2014-05-22). The Lupus Encyclopedia: A Comprehensive Guide for Patients and Families. JHU Press. ISBN 9781421409849.
- ↑ "Hydroxychloroquine: MedlinePlus Drug Information". medlineplus.gov. Archived from the original on 3 January 2018. Retrieved 23 July 2016.
- ↑ "WHO Disease and injury country estimates". World Health Organization. 2009. Retrieved Nov 11, 2009.
- ↑ "Leading Causes of Death - Women's Health USA 2010". mchb.hrsa.gov. Archived from the original on 2017-06-29. Retrieved 2015-06-14.
- ↑ Lerma, Edgar; Rosner, Mitchell (2012-10-28). Clinical Decisions in Nephrology, Hypertension and Kidney Transplantation. Springer Science & Business Media. ISBN 9781461444541. Archived from the original on 2022-12-23. Retrieved 2022-10-07.
- ↑ "Lupus Nephritis: Practice Essentials, Background, Pathophysiology". 2018-04-22. Archived from the original on 2019-12-20. Retrieved 2022-10-07.
{{cite journal}}: Cite journal requires|journal=(help)
External links
| Classification |
|---|