Methylene blue
 | |
| Names | |
|---|---|
| Trade names | Urelene blue, Provayblue, Proveblue, others[1][2] |
| Other names | CI 52015, basic blue 9[3] |
| |
| Clinical data | |
| Drug class | Thiazine dye[4] |
| Main uses | Methemoglobinemia[4][2] |
| Side effects | Headache, vomiting, confusion, shortness of breath, high blood pressure[4] |
| Pregnancy category |
|
| Routes of use | By mouth, intravenous (IV) |
| Defined daily dose | not established[5] |
| External links | |
| AHFS/Drugs.com | Monograph |
| Legal | |
| License data |
|
| Legal status |
|
| Pharmacokinetics | |
| Elimination half-life | 5 to 24 hours[4] |
| Chemical and physical data | |
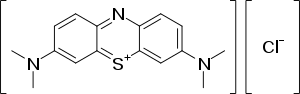
| Formula | C16H18ClN3S |
| Molar mass | 319.85 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
Methylene blue, also known as methylthioninium chloride, is a medication and dye.[4] As a medication, it is mainly used to treat methemoglobinemia.[4][2] Specifically, it is used to treat methemoglobin levels that are greater than 30% or in which there are symptoms despite oxygen therapy.[2] It has previously been used for cyanide poisoning and urinary tract infections, but this use is no longer recommended.[4] It is typically given by injection into a vein.[4]
Common side effects include headache, vomiting, confusion, shortness of breath, and high blood pressure.[4] Other side effects include serotonin syndrome, red blood cell breakdown, and allergic reactions.[4] Use often turns the urine, sweat, and stool blue to green in color.[2] While use during pregnancy may harm the baby, not using it in methemoglobinemia is likely more dangerous.[4][2] Methylene blue is a thiazine dye.[4] It works by converting the ferric iron in hemoglobin to ferrous iron.[2]
Methylene blue was first prepared in 1876, by Heinrich Caro.[6] It is on the World Health Organization's List of Essential Medicines.[7] In the United States, a 50 mg vial costs about US$191.40.[8] In the United Kingdom, a 50 mg vial costs the NHS about £39.38.[2]
Medical uses
Methemoglobinemia
Methylene blue is employed as a medication for the treatment of methemoglobinemia. This can arise from ingestion of certain pharmaceuticals, toxins, or broad beans.[9] Normally, through the NADH or NADPH dependent methemoglobin reductase enzymes, methemoglobin is reduced back to hemoglobin. When large amounts of methemoglobin occur secondary to toxins, methemoglobin reductases are overwhelmed. Methylene blue, when injected intravenously as an antidote, is itself first reduced to leucomethylene blue, which then reduces the heme group from methemoglobin to hemoglobin. Methylene blue can reduce the half life of methemoglobin from hours to minutes.[10] At high doses, however, methylene blue actually induces methemoglobinemia, reversing this pathway.[10]
Combined with light
Methylene blue combined with light has been used to treat resistant plaque psoriasis.[11]
Urinary tract infection
Methylene blue is a component of a urinary analgesic/anti-infective/anti-spasmodic known as "Prosed DS", a combination of phenyl salicylate, benzoic acid, hyoscyamine sulfate, and methenamine (aka hexamethylenetetramine and not to be confused with 'methanamine').[12]
Cyanide poisoning
Since its reduction potential is similar to that of oxygen and can be reduced by components of the electron transport chain, large doses of methylene blue are sometimes used as an antidote to potassium cyanide poisoning, a method first successfully tested in 1933 by Dr. Matilda Moldenhauer Brooks in San Francisco,[13] although first demonstrated by Bo Sahlin of Lund University, in 1926.[13][14]
Dye or stain

Methylene blue is used in endoscopic polypectomy as an adjunct to saline or epinephrine, and is used for injection into the submucosa around the polyp to be removed. This allows the submucosal tissue plane to be identified after the polyp is removed, which is useful in determining if more tissue needs to be removed, or if there has been a high risk for perforation. Methylene blue is also used as a dye in chromoendoscopy, and is sprayed onto the mucosa of the gastrointestinal tract in order to identify dysplasia, or pre-cancerous lesions. Intravenously injected methylene blue is readily released into the urine and thus can be used to test the urinary tract for leaks or fistulas.
In surgeries such as sentinel lymph node dissections, methylene blue can be used to visually trace the lymphatic drainage of tested tissues. Similarly, methylene blue is added to bone cement in orthopedic operations to provide easy discrimination between native bone and cement. Additionally, methylene blue accelerates the hardening of bone cement, increasing the speed at which bone cement can be effectively applied. Methylene blue is used as an aid to visualisation/orientation in a number of medical devices, including a Surgical sealant film, TissuePatch. In fistulas and pilonidal sinuses it is used to identify the tract for complete excision.[citation needed] It can also be used during gastrointestinal surgeries (such as bowel resection or gastric bypass) to test for leaks.
When methylene blue is "polychromed" (oxidized in solution or "ripened" by fungal metabolism,[15] as originally noted in the thesis of Dr. D. L. Romanowsky in the 1890s), it gets serially demethylated and forms all the tri-, di-, mono- and non-methyl intermediates, which are Azure B, Azure A, Azure C, and thionine, respectively.[16] This is the basis of the basophilic part of the spectrum of Romanowski-Giemsa effect. If only synthetic Azure B and Eosin Y is used, it may serve as a standardized Giemsa stain; but, without methylene blue, the normal neutrophilic granules tend to overstain and look like toxic granules. On the other hand, if methylene blue is used it might help to give the normal look of neutrophil granules and may also enhance the staining of nucleoli and polychromatophilic RBCs (reticulocytes).[17]
A traditional application of methylene blue is the intravital or supravital staining of nerve fibers, an effect first described by Paul Ehrlich in 1887.[18] A dilute solution of the dye is either injected into tissue or applied to small freshly removed pieces. The selective blue coloration develops with exposure to air (oxygen) and can be fixed by immersion of the stained specimen in an aqueous solution of ammonium molybdate. Vital methylene blue was formerly much used for examining the innervation of muscle, skin and internal organs.[19][20][21] The mechanism of selective dye uptake is incompletely understood; vital staining of nerve fibers in skin is prevented by ouabain, a drug that inhibits the Na/K-ATPase of cell membranes.[22]
Placebo
Methylene blue has been used as a placebo; physicians would tell their patients to expect their urine to change color and view this as a sign that their condition had improved.[23] This same side effect makes methylene blue difficult to test in traditional placebo-controlled clinical studies.[24]
Ifosfamide toxicity
Another use of methylene blue is to treat ifosfamide neurotoxicity. Methylene blue was first reported for treatment and prophylaxis of ifosfamide neuropsychiatric toxicity in 1994. A toxic metabolite of ifosfamide, chloroacetaldehyde (CAA), disrupts the mitochondrial respiratory chain, leading to an accumulation of nicotinamide adenine dinucleotide hydrogen (NADH). Methylene blue acts as an alternative electron acceptor, and reverses the NADH inhibition of hepatic gluconeogenesis while also inhibiting the transformation of chloroethylamine into chloroacetaldehyde, and inhibits multiple amine oxidase activities, preventing the formation of CAA.[25] The dosing of methylene blue for treatment of ifosfamide neurotoxicity varies, depending upon its use simultaneously as an adjuvant in ifosfamide infusion, versus its use to reverse psychiatric symptoms that manifest after completion of an ifosfamide infusion. Reports suggest that methylene blue up to six doses a day have resulted in improvement of symptoms within 10 minutes to several days.[26] Alternatively, it has been suggested that intravenous methylene blue every six hours for prophylaxis during ifosfamide treatment in people with history of ifosfamide neuropsychiatric toxicity.[27] Prophylactic administration of methylene blue the day before initiation of ifosfamide, and three times daily during ifosfamide chemotherapy has been recommended to lower the occurrence of ifosfamide neurotoxicity.[28]
Shock
It has also been used in septic shock and anaphylaxis.[29][30]
Methylene blue consistently increases blood pressure in people with vasoplegic syndrome (redistributive shock), but has not been shown to improve delivery of oxygen to tissues or to decrease mortality.[31][32][33][34]
Dosage
The defined daily dose is not established[5]
Side effects
| Cardiovascular | Central Nervous System | Dermatologic | Gastrointestinal | Genito-urinary | Hematologic |
|---|---|---|---|---|---|
| • Hypertension • Precordial pain |
• Dizziness • Mental confusion • Headache • Fever |
• Staining of skin • Injection site necrosis (SC) |
• Fecal discoloration • Nausea • Vomiting • Abdominal pain |
• Discoloration of urine (doses over 80 µg) • Bladder irritation |
• Anemia |
Methylene blue is a monoamine oxidase inhibitor (MAOI),[37] and if infused intravenously at doses exceeding 5 mg/kg, may precipitate serious serotonin toxicity, serotonin syndrome, if combined with any selective serotonin reuptake inhibitors (SSRIs) or other serotonin reuptake inhibitor (e.g., duloxetine, sibutramine, venlafaxine, clomipramine, imipramine).[38]
It causes hemolytic anemia in carriers of the G6PD (favism) enzymatic deficiency.
Chemistry
Methylene blue is a formal derivative of phenothiazine. It is a dark green powder that yields a blue solution in water. The hydrated form has 3 molecules of water per unit of methylene blue. Methylene blue has a pH of 6 in water(10g/l) at 25 °C (77 °F).
Preparation
This compound is prepared by oxidation of dimethyl-4-phenylenediamine in the presence of sodium thiosulfate:[39]
Light absorption properties
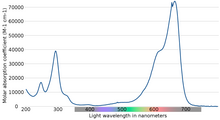
The maximum absorption of light is near 670 nm. The specifics of absorption depend on a number of factors, including protonation, adsorption to other materials, and metachromasy - the formation of dimers and higher-order aggregates depending on concentration and other interactions:[40]
| Species | Absorption peak | Extinction coefficient (dm3/mole·cm) |
|---|---|---|
| MB+ (solution) | 664 | 95000 |
| MBH2+ (solution) | 741 | 76000 |
| (MB+)2 (solution) | 605 | 132000 |
| (MB+)3 (solution) | 580 | 110000 |
| MB+ (adsorbed on clay) | 673 | 116000 |
| MBH2+ (adsorbed on clay) | 763 | 86000 |
| (MB+)2 (adsorbed on clay) | 596 | 80000 |
| (MB+)3 (adsorbed on clay) | 570 | 114000 |
Other uses

Redox indicator
Methylene blue is widely used as a redox indicator in analytical chemistry. Solutions of this substance are blue when in an oxidizing environment, but will turn colorless if exposed to a reducing agent. The redox properties can be seen in a classical demonstration of chemical kinetics in general chemistry, the "blue bottle" experiment. Typically, a solution is made of glucose (dextrose), methylene blue, and sodium hydroxide. Upon shaking the bottle, oxygen oxidizes methylene blue, and the solution turns blue. The dextrose will gradually reduce the methylene blue to its colorless, reduced form. Hence, when the dissolved dextrose is entirely consumed, the solution will turn blue again. The redox midpoint potential E0' is +0.01 V.[41]
Peroxide generator
Methylene blue is also a photosensitizer used to create singlet oxygen when exposed to both oxygen and light. It is used in this regard to make organic peroxides by a Diels-Alder reaction which is spin forbidden with normal atmospheric triplet oxygen.
Sulfide analysis
The formation of methylene blue after the reaction of hydrogen sulfide with dimethyl-p-phenylenediamine and iron(III) at pH 0.4 – 0.7 is used to determine by photometric measurements sulfide concentration in the range 0.020 to 1.50 mg/L (20 ppb to 1.5 ppm). The test is very sensitive and the blue coloration developing upon contact of the reagents with dissolved H2S is stable for 60 min. Ready-to-use kits such as the Spectroquant sulfide test[42] facilitate routine analyses. The methylene blue sulfide test is a convenient method often used in soil microbiology to quickly detect in water the metabolic activity of sulfate reducing bacteria (SRB). It should be observed that in this test, methylene blue is a product of reaction and not a reagent.
The addition of a strong reducing agent, such as ascorbic acid, to a sulfide-containing solution is sometimes used to prevent sulfide oxidation from atmospheric oxygen. Although it is certainly a sound precaution for the determination of sulfide with an ion selective electrode, it might however hamper the development of the blue color if the freshly formed methylene blue is also reduced, as described here above in the paragraph on redox indicator.
Water testing
A color reaction in an acidified, aqueous methylene blue solution containing chloroform can detect anionic surfactants in a water sample. Such a test is known as an MBAS assay (methylene blue active substances assay).
The MBAS assay cannot distinguish between specific surfactants, however. Some examples of anionic surfactants are carboxylates, phosphates, sulfates, and sulfonates.
Methylene blue value of fine aggregate
Methylene blue value reflects the amount of clay minerals in aggregate samples.[43] Methylene blue solution is successively added to fine aggregate which is being agitating in water. The presence of free dye solution can be checked with stain test on a filter paper.[44]
Biological staining
In biology methylene blue is used as a dye for a number of different staining procedures, such as Wright's stain and Jenner's stain. Since it is a temporary staining technique, methylene blue can also be used to examine RNA or DNA under the microscope or in a gel: as an example, a solution of methylene blue can be used to stain RNA on hybridization membranes in northern blotting to verify the amount of nucleic acid present. While methylene blue is not as sensitive as ethidium bromide, it is less toxic and it does not intercalate in nucleic acid chains, thus avoiding interference with nucleic acid retention on hybridization membranes or with the hybridization process itself.
It can also be used as an indicator to determine whether eukaryotic cells such as yeast are alive or dead. The methylene blue is reduced in viable cells, leaving them unstained. However dead cells are unable to reduce the oxidized methylene blue and the cells are stained blue. Methylene blue can interfere with the respiration of the yeast as it picks up hydrogen ions made during the process.
Aquaculture
Methylene blue is used in aquaculture and by tropical fish hobbyists as a treatment for fungal infections. It can also be effective in treating fish infected with ich although a combination of malachite green and formaldehyde is far more effective against the parasitic protozoa Ichthyophthirius multifiliis. It is usually used to protect newly laid fish eggs from being infected by fungus or bacteria. This is useful when the hobbyist wants to artificially hatch the fish eggs. Methylene Blue is also very effective when used as part of a "medicated fish bath" for treatment of ammonia, nitrite, and cyanide poisoning as well as for topical and internal treatment of injured or sick fish as a "first response".[45]
History
Methylene blue has been described as "the first fully synthetic drug used in medicine." Methylene blue was first prepared in 1876 by German chemist Heinrich Caro.[46]
Its use in the treatment of malaria was pioneered by Paul Guttmann and Paul Ehrlich in 1891. During this period before the first World War, researchers like Ehrlich believed that drugs and dyes worked in the same way, by preferentially staining pathogens and possibly harming them. Changing the cell membrane of pathogens is in fact how various drugs work, so the theory was partially correct although far from complete. Methylene blue continued to be used in the second World War, where it was not well liked by soldiers, who observed, "Even at the loo, we see, we pee, navy blue." Antimalarial use of the drug has recently been revived.[47] It was discovered to be an antidote to carbon monoxide poisoning and cyanide poisoning in 1933 by Matilda Brooks.[48]
The blue urine was used to monitor psychiatric patients' compliance with medication regimes. This led to interest - from the 1890s to the present day - in the drug's antidepressant and other psychotropic effects. It became the lead compound in research leading to the discovery of chlorpromazine.[49]
Names
The International Nonproprietary Name (INN) of methylene blue is methylthioninium chloride.[50][51]
Research
Malaria
Methylene blue was identified by Paul Ehrlich about 1891 as a possible treatment for malaria.[52] It disappeared as an anti-malarial during the Pacific War in the tropics, since American and Allied soldiers disliked its two prominent, but reversible side effects: turning the urine blue or green, and the sclera (the whites of the eyes) blue. Interest in its use as an anti-malarial has recently been revived,[49] especially due to its low price. Several clinical trials are in progress, trying to find a suitable drug combination. According to studies on children in Africa, it appears to have efficacy against malaria, but the attempts to combine methylene blue with chloroquine were disappointing.[53]
Alzheimer's
A Phase 3 clinical trial of LMTM (TauRx0237 or LMT-X), a derivative of methylene blue, failed to show any benefit against cognitive or functional decline in people with mild to moderate Alzheimer's disease. Disease progression for both the drug and the placebo were practically identical.[54][55]
Bipolar disorder
Methylene blue has been studied as an adjunctive medication in the treatment of bipolar disorder.[56]
Infectious diseases
It has been studied in AIDS-related Kaposi's sarcoma,[57] West Nile virus,[58] and to inactivate staphylococcus aureus,[59] and HIV-1.[60] Phenothiazine dyes and light have been known to have virucidal properties for over 70 years.[61]
See also
References
- ↑ Hamilton, Richart (2015). Tarascon Pocket Pharmacopoeia 2015 Deluxe Lab-Coat Edition. Jones & Bartlett Learning. p. 471. ISBN 9781284057560.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 British national formulary : BNF 69 (69 ed.). British Medical Association. 2015. p. 34. ISBN 9780857111562.
- ↑ Lillie, Ralph Dougall (1977). H. J. Conn's Biological stains (9th ed.). Baltimore: Williams & Wilkins. pp. 692p.
- ↑ 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 4.10 4.11 4.12 4.13 "Methylene Blue". The American Society of Health-System Pharmacists. Archived from the original on 10 May 2017. Retrieved 8 January 2017.
- ↑ 5.0 5.1 "WHOCC - ATC/DDD Index". www.whocc.no. Archived from the original on 30 October 2020. Retrieved 14 September 2020.
- ↑ Ahmad, Iqbal; Aqil, Farrukh (2008). New Strategies Combating Bacterial Infection. John Wiley & Sons. p. 91. ISBN 9783527622948. Archived from the original on 2017-09-18.
- ↑ World Health Organization (2019). World Health Organization model list of essential medicines: 21st list 2019. Geneva: World Health Organization. hdl:10665/325771. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- ↑ "Provayblue Prices, Coupons & Patient Assistance Programs - Drugs.com". www.drugs.com. Archived from the original on 16 January 2017. Retrieved 12 January 2017.
- ↑ Manual of Clinical Hematology Archived 2017-09-18 at the Wayback Machine, Joseph Mazza
- ↑ 10.0 10.1 Brent J. (2005). Critical care toxicology: diagnosis and management of the critically poisoned patient. Elsevier Health Sciences.
- ↑ Salah M.; Samy N.; Fadel M. (January 2009). "Methylene blue mediated photodynamic therapy for resistant plaque psoriasis". J. Drugs Dermatol. 8 (1): 42–9. PMID 19180895.
- ↑ "Prosed DS (Methenamine, Salicylate, Methylene Blue, Benzoic Acid Atropine and Hyoscyamine) Drug Information: Description, User Reviews, Drug Side Effects, Interactions - Prescribing Information at RxList". RxList. Archived from the original on 2011-11-02.
- ↑ 13.0 13.1 Matilda Moldenhauer Brooks (1936). "Methylene blue as an antidote for cyanide and carbon monoxide poisoning". The Scientific Monthly. 43 (6): 585–586. Bibcode:1936SciMo..43..585M. JSTOR 16280.
- ↑ Hanzlik, P. J. (4 February 1933). "Methylene Blue As Antidote for Cyanide Poisoning". JAMA. 100 (5): 357. doi:10.1001/jama.1933.02740050053028.
- ↑ Dako Education Guide - Special Stains and H & E " second edition Chapter 19: On Chemical Reactions and Staining Mechanisms by John A. Kiernan, Subsection What is Giemsa's stain and how does it color blood cells, bacteria and chromosomes? p172 Archived 2012-05-13 at the Wayback Machine
- ↑ Wilson TM (1907). "On the Chemistry and Staining Properties of Certain Derivatives of the Methylene Blue Group when Combined with Eosin". J Exp Med. 9 (6): 645–70. doi:10.1084/jem.9.6.645. PMC 2124692. PMID 19867116.
- ↑ Dacie and Lewis Practical Haematology 10th ed, p61
- ↑ Ehrlich, P. (1887) Biol. Centralblatt 6: 214, cited from Baker JR (1958) Principles of Biological Microtechnique (Reprinted 1970, with corrections). Methuen, London.
- ↑ Wilson JG (1910) Intra vitam staining with methylene blue. Anatomical Record 4: 267-277.
- ↑ Schabadasch A (1930) Untersuchungen zur Methodik der Methylenblaufarbung des vegetativen Nervensystems. Zeitschrift für Zellforschung 10: 221-243.
- ↑ Zacks Zacks SI (1973) The Motor Endplate, 2nd ed. Huntington, NY: Krieger
- ↑ Kiernan JA (1974) Effects of metabolic inhibitors on vital staining with methylene blue. Histochemistry 40: 51-57.
- ↑ Novella Steve. "The ethics of deception in medicine". Science Based Medicine. Archived from the original on 2008-01-29. Retrieved 2008-01-24.
- ↑ "Methylene blue for cognitive dysfunction in bipolar disorder". United States National Library of Medicine. September 20, 2005. Archived from the original on January 15, 2009. Retrieved 2009-02-15.
- ↑ Alici-Evcimen Y.; Breitbart W.S. (October 2007). "Ifosfamide neuropsychiatric toxicity in patients with cancer". Psychooncology. 16 (10): 956–960. doi:10.1002/pon.1161. PMID 17278152.
- ↑ Patel P.N. (2006). "Methylene blue for management of ifosfamide induced encephalopathy". Annals of Pharmacotherapy. 40 (2): 266–303. doi:10.1345/aph.1G114. PMID 16391008.
- ↑
Dufour C.; Grill J.; Sabouraud P.; et al. (February 2006). "Ifosfamide induced encephalopathy: 15 observations". Arch. Pediatr. (in French). 13 (2): 140–145. doi:10.1016/j.arcped.2005.10.021. PMID 16364615.
{{cite journal}}: CS1 maint: unrecognized language (link) - ↑ Aeschlimann T.; Cerny, T; Küpfer, A (1996). "Inhibition of (mono)amine oxidase activity and prevention of ifosfamide encephalopathy by methylene blue". Drug Metab. Dispos. 24 (12): 1336–1339. PMID 8971139.
- ↑ Jang, DH; Nelson, LS; Hoffman, RS (September 2013). "Methylene blue for distributive shock: a potential new use of an old antidote". Journal of Medical Toxicology. 9 (3): 242–9. doi:10.1007/s13181-013-0298-7. PMC 3770994. PMID 23580172.
- ↑ Paciullo, CA; McMahon Horner, D; Hatton, KW; Flynn, JD (July 2010). "Methylene blue for the treatment of septic shock". Pharmacotherapy. 30 (7): 702–15. doi:10.1592/phco.30.7.702. PMID 20575634.
- ↑ Hosseinian L, Weiner M, Levin MA, Fischer GW (January 2016). "Methylene Blue: Magic Bullet for Vasoplegia?". Anesth. Analg. 122 (1): 194–201. doi:10.1213/ANE.0000000000001045. PMID 26678471.
- ↑ Levin RL, Degrange MA, Bruno GF, Del Mazo CD, Taborda DJ, Griotti JJ, Boullon FJ (February 2004). "Methylene blue reduces mortality and morbidity in vasoplegic patients after cardiac surgery". Ann Thorac Surg. 77 (2): 496–9. doi:10.1016/S0003-4975(03)01510-8. PMID 14759425. Archived from the original on 2019-12-08. Retrieved 2013-11-17.
- ↑ "BestBets: Is Methylene Blue of benefit in treating adult patients who develop vasoplegic syndrome during Cardiac Surgery". Archived from the original on 2014-07-28.
- ↑ Stawicki SP, Sims C, Sarani B, Grossman MD, Gracias VH (May 2008). "Methylene blue and vasoplegia: who, when, and how?". Mini Rev Med Chem. 8 (5): 472–90. doi:10.2174/138955708784223477. PMID 18473936. Archived from the original on 2017-09-18. Retrieved 2020-04-01.
- ↑ Mokhlesi B.; Leikin J.B.; Murray P.; Corbridge T.C. (March 2003). "Adult toxicology in critical care: Part II: specific poisonings". Chest. 123 (3): 897–922. doi:10.1378/chest.123.3.897. PMID 12628894. Archived from the original on 2021-08-28. Retrieved 2020-01-14.
- ↑ Harvey J.W.; Keitt A.S. (May 1983). "Studies of the efficacy and potential hazards of methylene blue therapy in aniline-induced methaemoglobinaemia". Br. J. Haematol. 54 (1): 29–41. doi:10.1111/j.1365-2141.1983.tb02064.x. PMID 6849836.
- ↑ Ramsay RR; Dunford, C.; Gillman, C.K. (August 2007). "Methylene blue and serotonin toxicity: inhibition of monoamine oxidase A (MAO A) confirms a theoretical prediction". Br J Pharmacol. 152 (6): 946–951. doi:10.1038/sj.bjp.0707430. PMC 2078225. PMID 17721552.
- ↑ Gillman P.K. (October 2006). "Methylene blue implicated in potentially fatal serotonin toxicity". Anaesthesia. 61 (10): 1013–4. doi:10.1111/j.1365-2044.2006.04808.x. PMID 16978328.
- ↑ Horst Berneth (2012). "Azine Dyes". Ullmann's Encyclopedia of Industrial Chemistry. Weinheim: Wiley-VCH. doi:10.1002/14356007.a03_213.pub3. ISBN 978-3527306732.
- ↑ J. Cenens; R. A. Schoonheydt (1988). "Visible spectroscopy of methylene blue on hectorite, laponite B, and barasym in aqueous suspension". Clays and Clay Minerals. 36 (3): 214–224. Bibcode:1988CCM....36..214C. doi:10.1346/ccmn.1988.0360302.
- ↑ H Jakubowski (2016) Biochemistry, CHAPTER 8 - OXIDATION/PHOSPHORYLATION B: OXIDATIVE ENZYMES https://employees.csbsju.edu/hjakubowski/classes/ch331/oxphos/oloxidativeenzymes.html Archived 2020-10-27 at the Wayback Machine
- ↑ "Analytik und Probenvorbereitung". Archived from the original on 2007-03-15.
- ↑ "ASTM C1777 - 15 Standard Test Method for Rapid Determination of the Methylene Blue Value for Fine Aggregate or Mineral Filler Using a Colorimeter". Archived from the original on 2014-02-28.
- ↑ Construction Standard CS3:2013 – Aggregates for Concrete Archived 2014-06-02 at the Wayback Machine
- ↑ [1] Archived 2016-01-10 at the Wayback Machine
- ↑ Badische Anilin- und Sodafabrik [BASF] (Mannheim, Germany), "Verfahren zur Darstellung blauer Farbstoffe aus Dimethylanilin und anderen tertiaren aromatischen Monaminen" (Method for preparation of blue dyes from dimethylaniline and other tertiary aromatic monoamines), Deutsches Reich Patent no. 1886 (December 15, 1877). Available on-line at: P. Friedlaender, Fortschritte der Theerfarbenfabrikation und verwandter Industriezweige (Progress of the manufacture of coal-tar dyes and related branches of industry), volume 1 (Berlin, Germany: Julius Springer, 1888), pages 247-249. Archived 2015-03-21 at the Wayback Machine
- ↑ Coulibaly, Boubacar; Zoungrana, Augustin; Mockenhaupt, Frank P.; Schirmer, R. Heiner; Klose, Christina; Mansmann, Ulrich; Meissner, Peter E.; Müller, Olaf (2009). "Strong Gametocytocidal Effect of Methylene Blue-Based Combination Therapy against Falciparum Malaria: A Randomised Controlled Trial". PLOS ONE. 4 (5): e5318. Bibcode:2009PLoSO...4.5318C. doi:10.1371/journal.pone.0005318. PMC 2673582. PMID 19415120.
- ↑ Brooks, Matilda Moldenhauer (1933). "Methylene Blue As Antidote for Cyanide and Carbon Monoxide Poisoning". JAMA. 100: 59. doi:10.1001/jama.1933.02740010061028.
- ↑ 49.0 49.1 Schirmer H.; Coulibaly B.; Stich A.; et al. (2003). "Methylene blue as an antimalarial agent—past and future". Redox Rep. 8 (5): 272–276. doi:10.1179/135100003225002899. PMID 14962363.
- ↑ Adams V.; Marley J.; McCarroll C. (November 2007). "Prilocaine induced methaemoglobinaemia in a medically compromised patient. Was this an inevitable consequence of the dose administered?". Br. Dent. J. 203 (10): 585–7. doi:10.1038/bdj.2007.1045. PMID 18037845.
- ↑ Linz A.J.; Greenham R.K.; Fallon L.F. (May 2006). "Methemoglobinemia: an industrial outbreak among rubber molding workers". J. Occup. Environ. Med. 48 (5): 523–8. doi:10.1097/01.jom.0000201815.32098.99. PMID 16688009.
- ↑ Guttmann, P. and Ehrlich. P. (1891) "Über die Wirkung des Methylenblau bei Malaria" Archived 2017-02-17 at the Wayback Machine (On the effect of methylene blue on malaria), Berliner Klinische Wochenschrift, 28 : 953-956.
- ↑ Meissner P.E.; Mandi G.; Coulibaly B.; et al. (2006). "Methylene blue for malaria in Africa: results from a dose-finding study in combination with chloroquine". Malaria Journal. 5: 84. doi:10.1186/1475-2875-5-84. PMC 1617109. PMID 17026773.
- ↑ "Tau Drug Flops in Study". Archived from the original on 2017-10-10. Retrieved 2017-10-09.
- ↑ "In First Phase 3 Trial, the Tau Drug LMTM Did Not Work. Period". Archived from the original on 2020-02-20. Retrieved 2017-10-09.
- ↑ Alda, Martin; McKinnon, Margaret; Blagdon, Ryan; Garnham, Julie; MacLellan, Susan; O'Donovan, Claire; Hajek, Tomas; Nair, Cynthia; Dursun, Serdar (2017-01-01). "Methylene blue treatment for residual symptoms of bipolar disorder: randomised crossover study". The British Journal of Psychiatry. 210 (1): 54–60. doi:10.1192/bjp.bp.115.173930. ISSN 1472-1465. PMID 27284082.
- ↑ Tardivo J.P.; Del Giglio A.; Paschoal L.H.; Baptista M.S. (August 2006). "New photodynamic therapy protocol to treat AIDS-related Kaposi's sarcoma". Photomedical Laser Surg. 24 (4): 528–31. doi:10.1089/pho.2006.24.528. PMID 16942436.
- ↑ Papin J.F.; Floyd R.A.; Dittmer D.P. (November 2005). "Methylene blue photoinactivation abolishes West Nile virus infectivity in vivo". Antiviral Res. 68 (2): 84–7. doi:10.1016/j.antiviral.2005.07.001. PMID 16118025.
- ↑ Zolfaghari P.S.; Packer S.; Singer M.; Nair S.P.; Bennett J.; Street C.; Wilson M. (2009). "In vivo killing of Staphylococcus aureus using a light-activated antimicrobial agent". BMC Microbiol. 9: 27. doi:10.1186/1471-2180-9-27. PMC 2642833. PMID 19193212.
- ↑ Floyd R.A.; Schneider J.E.; Dittmer D.P. (March 2004). "Methylene blue photoinactivation of RNA viruses". Antiviral Res. 61 (3): 141–51. doi:10.1016/j.antiviral.2003.11.004. PMID 15168794.
- ↑ Wagner S.J.; Skripchenko A.; Robinette D.; Mallory D.A.; Hirayama J.; Cincotta L.; Foley J. (2000). "The use of dimethylmethylene blue for virus photoinactivation of red cell suspensions". Dev. Biol. (Basel). 102: 125–9. PMID 10794099.
External links
| Identifiers: |
|
|---|
- "Methylene blue". Drug Information Portal. U.S. National Library of Medicine. Archived from the original on 2020-04-11. Retrieved 2020-04-11.
- "Methylene blue test". MedlinePlus. Archived from the original on 2020-04-11. Retrieved 2020-04-11.
- Pages using duplicate arguments in template calls
- Webarchive template wayback links
- CS1 maint: unrecognized language
- Articles with hatnote templates targeting a nonexistent page
- Drugs with non-standard legal status
- Chemical articles with unknown parameter in Infobox drug
- Chemical articles without CAS registry number
- Articles without EBI source
- Chemical pages without ChemSpiderID
- Chemical pages without DrugBank identifier
- Articles without KEGG source
- Articles without UNII source
- Drugs missing an ATC code
- All articles with unsourced statements
- Articles with unsourced statements from April 2018
- Articles with invalid date parameter in template
- Antidotes
- Histology
- Redox indicators
- Thiazine dyes
- Vital stains
- World Health Organization essential medicines
- Monoamine oxidase inhibitors
- Phenothiazines
- Chlorides
- RTT
- Dimethylamino compounds
