Melanonychia
| Melanonychia | |
|---|---|
 | |
| Causes | Racial, skin cancer, infection, medications, lichen planus[1] |
| Risk factors | Dark skin[2] |
| Diagnostic method | Appearance, biopsy[2] |
| Differential diagnosis | Subungal melanoma |
| Frequency | Common,[3] males=females[1] |
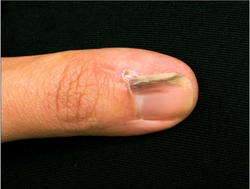
Melanonychia, a type of chromonychia, describes a black or brown discoloration of finger or toenails.[3][4] It typically appears as long vertical bands, but can be transverse, running horizontally across the nail, or involve the whole nail.[2] The bands can vary in width and number.[3] When a single longitudinal melanonychia dark band or mark suddenly appears in a single previously normal nail, a diagnosis of skin cancer needs ruling out.[5]
Melanonychia is a type of discoloration in the nail.[4] It can be normal or be associated with cancer or direct injury.[1] It can occur in some inherited disorders such as Peutz-Jeghers syndrome, endocrine disease such as Addison's disease, skin diseases such as lichen planus and acanthosis nigricans, and nutritional deficiency such as vitamin B12 deficiency.[2] It may be associated with some treatments such as PUVA therapy, ionizing radiation, and chemotherapy.[2] Medications that cause discoloration of nails include antimalarials, minocycline, and antivirals such as zidovudine.[2] Fungal nail infection can present with melanonychia.[2]
Diagnosis is usually by appearance.[2] A biopsy is required if there is a single new band in one nail, and may be required if the band is triangular where it is narrower near the nail fold, if the band border is blurred, if the discoloration is not uniform, if the band is wider than 6mm, or there is pigment of the periungal skin.[2] It may appear similar to subungal melanoma.[6]
It is common, occurs in all ages, and males and females are affected equally.[1] Between 77 and 96% of black people and 11% of Asian people have longitudinal melanonychia.[2]
Definition and signs
Melanonychia is the term used to describe the black or brown discoloration of finger or toenails.[3] It typically appears as longitudinal bands, but can be transverse or involve the whole nail.[2]
-
Melanonychia (longitudinal)
-
Melanonychia (transverse)
-
Melanonychia (whole nail)
Causes
Melanonychia can be normal or be associated with cancer or direct injury.[1] It can occur in some inherited disorders such as Peutz-Jeghers syndrome, endocrine disease such as Addison's disease, skin diseases such as lichen planus and acanthosis nigricans, and nutritional deficiency such as vitamin B12 deficiency.[2] It may be associated with some treatments such as PUVA therapy, ionizing radiation, and chemotherapy.[2] Medications that cause discoloration of nails include antimalarials, minocycline, and antivirals such as zidovudine.[2] Fungal nail infection can present with melanonychia.[2] It can also occur in pregnancy and graft-vs-host disease.[5]
Depending on the cause, the number and width of the coloured bands vary.[3] Drug exposure, skin diseases, and racial pigmentation characteristically involve multiple nails, and cancer tends to present with discolouration in one nail.[3]
Racial
Melanonychia is usually a normal finding in people with dark skin, Fitzpatrick skin type V and VI.[1]
-
Racial melanonychia (multiple longitudinal bands of several nails)
Cancer
-
Melanonychia in Bowen's disease
Infectious
-
Melanonychia due to pseudomonas
Drug-induced
-
Melanonychia with Imitimib
-
Nail colour changes due to dithranol
-
Melanonychia from longterm use of hydroxycarbamide
Other
-
Melanonychia in lichen planus
-
Laugier-Hunziker Syndrome melanonychia
Diagnosis
Diagnosis is usually by appearance.[2] A biopsy is required to rule out skin cancer if a single longitudinal melanonychia dark band or mark suddenly appears in a single previously normal nail, if there is a personal or family history of melanoma, or if the band darkens, grows wider, becomes raised with blurry borders, and if the nail folds exhibits pigment.[5]
Epidemiology
It is common, occurs in all ages, and males and females are affected equally.[1] Between 77 and 96% of black people and 11% of Asian people have longitudinal melanonychia.[2] Almost all Afro-Caribbean people will have some brownish nail discolouration by age 50.[1]
See also
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 Hiu-Kan Ip, Ken. "Melanonychia | DermNet NZ". dermnetnz.org. Archived from the original on 12 April 2022. Retrieved 12 April 2022.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 2.13 2.14 2.15 2.16 James, William D.; Elston, Dirk; Treat, James R.; Rosenbach, Misha A.; Neuhaus, Isaac (2020). "33. Diseases of the skin appendages". Andrews' Diseases of the Skin: Clinical Dermatology (13th ed.). Edinburgh: Elsevier. pp. 789–790. ISBN 978-0-323-54753-6. Archived from the original on 2023-07-01. Retrieved 2023-05-31.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 Singal, Archana; Bisherwal, Kavita (13 January 2020). "Melanonychia: Etiology, Diagnosis, and Treatment". Indian Dermatology Online Journal. 11 (1): 1–11. doi:10.4103/idoj.IDOJ_167_19. ISSN 2229-5178. PMID 32055501. Archived from the original on 6 February 2021. Retrieved 12 April 2022.
- ↑ 4.0 4.1 Cao, Lei; Shi, Ren-lin; Tan, Cheng; Bi, Xin Ling; Zang, Ru-Zhi; Chen, Liu-Qing; Yuan, Shan; Rigopoulos, Dimitris; Ma, Dong-Lai; Zhu, Wen-Yuan; Li, Heng-Jin; Yin, Zhi-Quiang (2018). "20. Disorders of skin appendages". In Zhu, Wen-Yuan; Tan, Cheng; Zhang, Ru-zhi (eds.). Atlas of Skin Disorders: Challenging Presentations of Common to Rare Conditions. Singapore: Springer. pp. 303–305. ISBN 978-981-10-8036-4. Archived from the original on 2023-06-30. Retrieved 2023-06-02.
- ↑ 5.0 5.1 5.2 Leung, Alexander K. C.; Lam, Joseph M.; Leong, Kin Fon; Sergi, Consolato M. (November 2019). "Melanonychia striata: clarifying behind the Black Curtain. A review on clinical evaluation and management of the 21st century". International Journal of Dermatology. 58 (11): 1239–1245. doi:10.1111/ijd.14464. ISSN 1365-4632. PMID 31006857. Archived from the original on 2021-10-31. Retrieved 2022-04-15.
- ↑ Onalaja, Amanda A.; Taylor, Susan C. (2021). "1. Defining skin color". In Li, Becky S.; Maibach, Howard I. (eds.). Ethnic Skin and Hair and Other Cultural Considerations. Switzerland: Springer. pp. 8–9. ISBN 978-3-030-64829-9. Archived from the original on 2022-09-15. Retrieved 2022-08-29.