Lower motor neuron lesion
| Lower motor neuron lesion | |
|---|---|
 | |
| Lower motor neuron in red | |
| Types | Neurology |
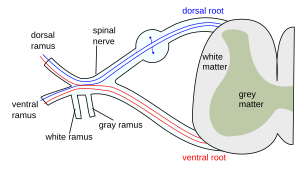
A lower motor neuron lesion is a lesion which affects nerve fibers traveling from the lower motor neuron(s) in the anterior horn/anterior grey column of the spinal cord, or in the motor nuclei of the cranial nerves, to the relevant muscle(s).[1]
One major characteristic used to identify a lower motor neuron lesion is flaccid paralysis – paralysis accompanied by loss of muscle tone. This is in contrast to an upper motor neuron lesion, which often presents with spastic paralysis – paralysis accompanied by severe hypertonia.
Signs and symptoms
- Muscle paresis or paralysis
- Fibrillations
- Fasciculations – caused by increased receptor concentration on muscles to compensate for lack of innervation.
- Hypotonia or atonia – Tone is not velocity dependent.
- Hyporeflexia - Along with deep reflexes even cutaneous reflexes are also decreased or absent.
- Strength – weakness is limited to segmental or focal pattern, Root innervated pattern[clarification needed]
The extensor plantar reflex is usually absent. Muscle paresis/paralysis, hypotonia/atonia, and hyporeflexia/areflexia are usually seen immediately following an insult. Muscle wasting, fasciculations and fibrillations are typically signs of end-stage muscle denervation and are seen over a longer time period. Another feature is the segmentation of symptoms – only muscles innervated by the damaged nerves will be symptomatic.
Causes
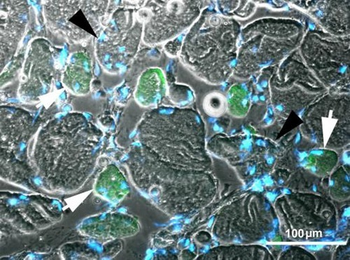
The most common causes of lower motor neuron injuries are trauma to peripheral nerves that serve the axons, and viruses that selectively attack ventral horn cells. Disuse atrophy of the muscle occurs i.e., shrinkage of muscle fibre finally replaced by fibrous tissue (fibrous muscle) Other causes include Guillain–Barré syndrome, West Nile fever, C. botulism, polio, and cauda equina syndrome; another common cause of lower motor neuron degeneration is amyotrophic lateral sclerosis.
Diagnosis
Differential diagnosis
- Myasthenia gravis – synaptic transmission at motor end-plate is impaired
- Amyotrophic lateral sclerosis – causes death of motor neurons, although exact cause is unknown it has been suggested that abnormal build-up of proteins proves toxic for the neurons.
Management
In terms of treatment for Amyotrophic lateral sclerosis, Riluzole has been found to modestly prolong survival by about 2–3 months.[2][3][4] It may have a greater survival benefit for those with bulbar-onset ALS.[3]
See also
References
- ↑ James D. Fix (1 October 2007). Neuroanatomy. Lippincott Williams & Wilkins. pp. 120–. ISBN 978-0-7817-7245-7. Archived from the original on 27 June 2014. Retrieved 17 November 2010.
- ↑ Carlesi C, Pasquali L, Piazza S, Lo Gerfo A, Caldarazzo Ienco E, Alessi R, Fornai F, Siciliano G (March 2011). "Strategies for clinical approach to neurodegeneration in Amyotrophic lateral sclerosis". Archives Italiennes de Biologie. 149 (1): 151–67. doi:10.4449/aib.v149i1.1267. PMID 21412722.
- ↑ 3.0 3.1 Miller, Rg; Mitchell, Jd; Lyon, M; Moore, Dh (22 April 2002). "Riluzole for amyotrophic lateral sclerosis (ALS)/motor neuron disease (MND)". Cochrane Database of Systematic Reviews: CD001447. doi:10.1002/14651858.CD001447. Retrieved 3 September 2022.
- ↑ "Motor Neuron Diseases Fact Sheet | National Institute of Neurological Disorders and Stroke". www.ninds.nih.gov. Archived from the original on 15 September 2022. Retrieved 4 September 2022.
External links
| Classification |
|---|