Leishmania braziliensis
| Leishmania braziliensis | |
|---|---|
| Scientific classification | |
| Domain: | Eukaryota |
| Phylum: | Euglenozoa |
| Class: | Kinetoplastea |
| Order: | Trypanosomatida |
| Genus: | Leishmania |
| Species: | L. braziliensis
|
| Binomial name | |
| Leishmania braziliensis Vianna, 1911
| |
Leishmania braziliensis is a Leishmania species.[1]
It is associated with leishmaniasis.Geographical distribution is to the countries of South and central America. The forms (stages) are amastigote in the human cells body and animals.
Biology
Leishmania braziliensis, like other species of Leishmania rely on asexual reproduction in the intermediate mammalian host to greatly increase population density. Such reproduction is often witnessed in mononuclear phagocytes (dendritic cells, monocytes, neutrophils) of the mammalian host, with the macrophages being the target white blood cell of the parasite.[2] Recently, it has been hypothesized through two studies[3] that certain members of Leishmania genus (e.g. L. braziliensis) are capable of sexual reproduction in the gut of the sand-fly vector. More work is needed to establish a clear pattern of sexual reproduction in the genus.[4]
The reproduction of Leishmania braziliensis vector, the sandfly, is dependent on environmental conditions. Environmental conditions such as high humidity, higher temperatures, deforestation add an increased risk because it causes increased reproduction of the parasite carrying sandflies.[5] These environmental changes put more people at risk with the vector and cause a greater geographic distribution of the sandfly and, consequently, the infectious disease.
Epidemiology
Ceará, Brazil
Historical Introduction into Brazil
Leishmania braziliensis is a species of leishmania or leishmaniasis that has emerged in Northeast Brazil. It is an infectious disease that is spread by a parasite in sandflies that use domestic dogs as hosts.[6] The emergence of leishmaniasis in Brazil, specifically the Northeast state of Ceará, is theorized to date back to the Great Drought of the 19th century Brazil.
The Grande Seca of 1877 to 1878 led to the mass migration of approximately 55 thousand Brazilians from Ceará to the Amazon for employment on rubber plantations.[7] The disease is easily and mostly transmitted on plantations in which the people live and work.[8]Direct and primary evidence of Leishmaniasis' existence is extremely minimal as the disease was not known to the Northeast and therefore was not identified and labeled until 1895 in Bahia.[9] But, even though there was a lack of name-calling evidence, there are still reports of a disease that matches the descriptions of Leishmania braziliensis. In 1827, before the Great Drought, Rabello cites reports from missionaries in the Amazon region seeing people with skin lesions that fit the description of the disease. In 1909, the newly graduated medical student at the time of the drought, Studart, reported a skin condition that has the potential of being Leishmaniasis.[10] It is also possible that in combination with a lack of general information and knowledge of the disease to the public plus the mass deaths and burials that occurred from 1877 to 1879, that people were dying of Leishmaniasis without knowing the true cause of their death.
On December 10th of 1879, Studart reported seeing more than a thousand people die in one day.[10] It is very possible that a portion of those could have died because of Leishmaniasis. An unknown disease is also mentioned by Herbert Huntington Smith, to which he attributes the death of 430 thousand people out of half a million who died, crediting the cause of death for the remaining 70 thousand to "various diseases".[7] Because not many primary sources were preserved, as stated candidly by drought writer Joao Eudes da Costa, it is very difficult to find sources during this time that directly point to the presence of Leishmaniasis during the Great Drought. Regardless, there is evidence of the disease before and after the drought, so it is highly likely that it was present and exacerbated during the Grande Seca. After contracting and spreading the disease within the plantations, workers later left the Amazon and returned to the Northeast carrying the parasite and introducing the first cases of leishmaniasis to the state.[citation needed]
Contemporary
The environmental conditions and the socio-economic factors of the drought-stricken Ceará made the area perfect and the people vulnerable to the spread of leishmaniasis. The migrants and those that remained in Ceará were malnourished, immunocompromised, and suffered from poor or even lack of sanitation and housing. In addition to the fact that the state is a semiarid region, the condition of Ceará after the Grande Seca made it a breeding ground for leishmaniasis infections that resulted in the disease being cemented into the state.
Visceral Leishmaniasis, which is the most common in the Northeast region of Brazil, causes the infected to have fever, skin lesions, skin tumors, loss in weight, spleen and liver enlargement, and if left untreated, death.[8] Environmental conditions, socio-economic status, demographic and human behaviors are what pose major risks to humans as well as manmade risks like migration, deforestation, urbanization, climate change, and immunosuppression.[8] Environmental conditions such as high humidity, higher temperatures, and deforestation add an increased risk because they cause increased reproduction and geographic distribution of the parasite-carrying sandflies and, consequently, of the infectious disease.[5]Leishmaniasis has made its appearance in 1981 to 1985 in Teresina; it reached epidemic levels in 1992 with a peak in 1994.[6] These epidemics were preceded by long and severe droughts in the region. From 1986 to 2005, Ceará has had more than 49 thousand new cases of Leishmania braziliensis; this estimate is like an underestimate since it is difficult to report the number of cases in rural areas. Those suffering from the disease are living the same lifestyle and with the same vulnerabilities as the Brazilians with leishmaniasis directly after the Great Drought. The diseased in modern-day Ceará are commonly poor teenagers aged 15 to 19, working in agriculture, and are male.[11]
Leishmania braziliensis is usually referred to as a rural problem since the increased risk factors are common in rural areas of Ceará. The people of the Northeast are still the most vulnerable. The drivers of the disease target those that live in crowded and underdeveloped housing near rubbish, sewage, and polluted water sources.[5] Though the disease targets Ceará the hardest because of its conditions, migration has spread the disease to larger cities, as more droughts, famine, and lack of usable farmland have led to large migrations from rural areas to cities.[6]This massive influx of people creates a space for the disease to spread and infect easily. Leishmaniasis is found more commonly in favelas or “shanty towns” as the residents have increased risks and live in “overcrowded conditions with inadequate housing and sanitary facilities,” (Arias, J R et al.). In addition, domestic stray dogs are the “principal animal reservoir” for the disease,[6] which makes urban areas like the favelas at an even greater risk because strays are common in these areas.[12]
Infection
Signs and symptoms
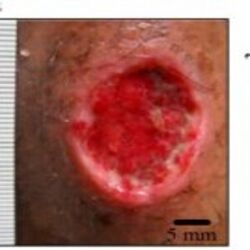
Within a few months of infection, an ulcer forms. After healing there is an asymptomatic phase for three to twenty years. At this time, the parasite causes oral and nasal lesions causing severe damage to the mucus membranes.
Visceral Leishmaniasis causes the infected to have a fever, skin lesions, skin tumors, loss in weight, spleen and liver enlargement, and if left untreated, death.[13]
Treatment
Pentostam, Liposomal and lipid complex preparations of Amphotericin B, or paromomycin can be given.
In Brazil, Currently, the most common treatment for humans to cure Leishmaniasis is the drug pentavalent antimony.[11] The treatment is expensive, toxic, and only “variably effective.” Although 80 percent of patients respond successfully to the drug, only 40 percent are successfully cured of the disease after one treatment. Most patients undergo multiple treatments that last 60 days each time.[11]
References
- ↑ Vargas-Inchaustegui, Diego A.; Xin, Lijun; Soong, Lynn (1 June 2008). "Leishmania braziliensis Infection Induces Dendritic Cell Activation, ISG15 Transcription, and the Generation of Protective Immune Responses". The Journal of Immunology. 180 (11): 7537–7545. doi:10.4049/jimmunol.180.11.7537. PMC 2641013. PMID 18490754.
- ↑ Peters, Nathan C.; Egen, Jackson G.; Secundino, Nagila; Debrabant, Alain; Kimblin, Nicola; Kamhawi, Shaden; Lawyer, Phillip; Fay, Michael P.; Germain, Ronald N.; Sacks, David (15 August 2008). "In vivo imaging reveals an essential role for neutrophils in Leishmaniasis transmitted by sand flies". Science. 321 (5891): 970–974. Bibcode:2008Sci...321..970P. doi:10.1126/science.1159194. PMC 2606057. PMID 18703742.
- ↑ Rougeron, Virginie; De Meeûs, Thierry; Hide, Mallorie; Waleckx, Etienne; Bermudez, Herman; Arevalo, Jorge; Llanos-Cuentas, Alejandro; Dujardin, Jean-Claude; De Doncker, Simone; Le Ray, Dominique; Ayala, Francisco J.; Bañuls, Anne-Laure (23 June 2009). "Extreme inbreeding in Leishmania braziliensis". Proceedings of the National Academy of Sciences of the United States of America. 106 (25): 10224–10229. Bibcode:2009PNAS..10610224R. doi:10.1073/pnas.0904420106. PMC 2700931. PMID 19497885.
- ↑ Rougeron, Virginie; De Meeûs, Thierry; Kako Ouraga, Sandrine; Hide, Mallorie; Bañuls, Anne-Laure (19 August 2010). "'Everything You Always Wanted to Know about Sex (but Were Afraid to Ask)' in Leishmania after Two Decades of Laboratory and Field Analyses". PLOS Pathogens. 6 (8): e1001004. doi:10.1371/journal.ppat.1001004. PMC 2924324. PMID 20808896.
- ↑ 5.0 5.1 5.2 Oryan, A.; Akbari, M. (October 2016). "Worldwide risk factors in leishmaniasis". Asian Pacific Journal of Tropical Medicine. 9 (10): 925–932. doi:10.1016/j.apjtm.2016.06.021. PMID 27794384.
- ↑ 6.0 6.1 6.2 6.3 Arias, Jorge (June 1996). "The Reemergence of Visceral Leishmaniasis in Brazil". Emerging Infectious Diseases. 2 (2): 145–146. doi:10.3201/eid0202.960213. PMC 2639817. PMID 8903218.
- ↑ 7.0 7.1 Smith, Herbert Huntington (1879). "Ceará and the Drought". Brazil, the Amazons and the Coast. C. Scribner's Sons. pp. 398–435. Archived from the original on 2023-07-03. Retrieved 2023-07-03.
- ↑ 8.0 8.1 8.2 Schriefer, Albert; Guimarães, Luiz H.; Machado, Paulo R.L.; Lessa, Marcus; Lessa, Hélio A.; Lago, Ednaldo; Ritt, Guilherme; Góes-Neto, Aristóteles; Schriefer, Ana L.F.; Riley, Lee W.; Carvalho, Edgar M. (June 2009). "Geographic Clustering of Leishmaniasis in Northeastern Brazil1". Emerging Infectious Diseases. 15 (6): 871–876. doi:10.3201/eid1506.080406. PMC 2727348. PMID 19523284.
- ↑ Moreira, Juliano (1895). "Existe na Bahia o botão de Biskra" [Biskra button exists in Bahia]. Gaz Méd Bahia (in português): 254–8.
- ↑ 10.0 10.1 Studart, Guilherme Studart (1997). Climatologia, epidemias e endemias do Ceará [Climatology, epidemics and endemics in Ceará] (in português). Fundação Waldemar Alcântara. OCLC 44549307.[page needed]
- ↑ 11.0 11.1 11.2 Turetz, Meredith L.; Machado, Paulo R.; Ko, Albert I.; Alves, Fábio; Bittencourt, Achiléa; Almeida, Roque P.; Mobashery, Niloufar; Johnson, Jr., Warren D.; Carvalho, Edgar M. (15 December 2002). "Disseminated Leishmaniasis: A New and Emerging Form of Leishmaniasis Observed in Northeastern Brazil". The Journal of Infectious Diseases. 186 (12): 1829–1834. doi:10.1086/345772. PMID 12447770.
- ↑ Rondon, F.C.M.; Bevilaqua, C.M.L.; Franke, C.R.; Barros, R.S.; Oliveira, F.R.; Alcântara, A.C.; Diniz, A.T. (August 2008). "Cross-sectional serological study of canine Leishmania infection in Fortaleza, Ceará state, Brazil". Veterinary Parasitology. 155 (1–2): 24–31. doi:10.1016/j.vetpar.2008.04.014. PMID 18565676.
- ↑ "About Leishmaniasis". DNDi. 12 September 2019. Archived from the original on 10 May 2020. Retrieved 18 April 2022.
Further reading
- Alcazar, Wilmer; López, Adrian Silva; Alakurtti, Sami; Tuononen, Maija-Liisa; Yli-Kauhaluoma, Jari; Ponte-Sucre, Alicia (November 2014). "Betulin derivatives impair Leishmania braziliensis viability and host–parasite interaction". Bioorganic & Medicinal Chemistry. 22 (21): 6220–6226. doi:10.1016/j.bmc.2014.08.023. PMID 25240731.