Granulomatous amoebic encephalitis
| Granulomatous amoebic encephalitis | |
|---|---|
 | |
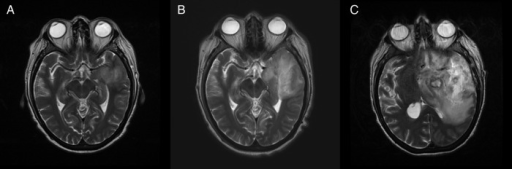
| T2-weighted MRI showing liquefied, necrotic brain tissue as a result of GAE caused by an infection of Acanthamoeba, genotype T18 | |
| Specialty | Infectious disease |
| Symptoms | Fever, headaches, personality changes[1] |
| Complications | Seizures, coma |
| Causes | Acanthamoeba, Balamuthia mandrillaris, and Sappinia pedata |
Granulomatous amoebic encephalitis (GAE) is a rare, usually fatal, subacute-to-chronic central nervous system disease caused by certain species of free-living amoebae[2] of the genera Acanthamoeba, Balamuthia and Sappinia pedata.[3][4] The term is most commonly used with Acanthamoeba. In more modern references, the term "balamuthia amoebic encephalitis" (BAE) is commonly used when Balamuthia mandrillaris is the cause.[5][6][7][8]
Signs and symptoms
GAE starts slowly, with symptoms like headache, nausea, dizziness, irritability and a low-grade fever. The CNS symptoms depend on the part of the brain that is infected. Changes in behavior are an important sign. Other CNS signs may include seizures, focal neurologic signs, diplopia (double vision), cranial nerve palsies, ataxia, confusion, and personality changes.[1]
Some of the symptoms may mimic glioma (especially brainstem glioma), or other brain diseases, which may hamper timely diagnosis. The symptoms are caused by inflammatory necrosis of brain tissue brought on by compounds released from the organisms.[citation needed]
Risk factors
Factors that may increase the risk of Granulomatous Amebic Encephalitis are the following:[9]
- Excessive use of antibiotics
- Cancer
- Lupus
- Liver cirrhosis
Diagnosis
The condition can be difficult for doctors to diagnose, because it is a rare disease.[10] A brain biopsy will reveal the presence of infection by pathogenic amoebas. In GAE, these present as general inflammation and sparse granules. On microscopic examination, infiltrates of amoebic cysts and/or trophozoites will be visible.[citation needed]
-
Image of granulomatous amoebic encephalitis caused by Acanthamoeba
-
A: T2-weighted MRI showing liquefied, necrotic brain tissue as a result of GAE caused by Balamuthia mandrillaris
B: T1-weighted MRI showing expansion and addition of necrotic areas 4 days later
Treatment
Acanthamoeba
Antifungal drugs including ketoconazole, miconazole, 5-flucytosine and pentamidine have been shown to be effective against Acanthamoeba in vitro.[11]
Balamuthia
Like with Acanthamoeba, infection of the brain with this organism rapidly turns fatal in most cases.[12] However some survivors have been reported:[citation needed]
Two patients survived after being successfully treated with a therapy consisting of flucytosine, pentamidine, fluconazole, sulfadiazine, and azithromycin. Thioridazine or trifluoperazine was also given. Successful treatment in these cases was credited to "awareness of Balamuthia as the causative agent of encephalitis and early initiation of antimicrobial therapy."[13]
In one case, cloxacillin, ceftriaxone, and amphotericin B were tried, but this treatment protocol did not prove effective.[14]
Prognosis
Even with treatment, CNS infection with Acanthamoeba is often fatal, and there are very few recorded survivors, almost all of whom had permanent neurocognitive deficits.[11] The prognosis is largely influenced by the time of diagnosis, how virulent and sensitive the Acanthamoeba strain is, and, most crucially, the immune status of the affected person. Due to it commonly being an opportunistic infection, the prognosis is generally poor, with a mortality rate approaching 90%.[1]
Sappinia pedata can cause GAE, however only one case of GAE due to S. pedata infection has ever been reported, and the patient survived without any long-term consequences.[15]
See also
- Naegleriasis, an almost invariably fatal infection of the brain by the percolozoan Naegleria fowleri
References
- ↑ 1.0 1.1 1.2 Duggal, Shalini Dewan; Rongpharpi, Sharon Rainy; Duggal, Ashish Kumar; Kumar, Avinash; Biswal, Indu (2018-01-22). "Role of Acanthamoeba in Granulomatous Encephalitis: A Review". Journal of Infectious Diseases & Immune Therapies. 2017.
- ↑ "Amebic Meningoencephalitis: Overview - eMedicine". 2018-07-24. Archived from the original on 2021-04-11. Retrieved 2022-06-30.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ Guarner, J.; Bartlett, J.; Shieh, W.; Paddock, C.; Visvesvara, G.; Zaki, S. (2007). "Histopathologic spectrum and immunohistochemical diagnosis of amebic meningoencephalitis". Modern Pathology. 20 (12): 1230–1237. doi:10.1038/modpathol.3800973. PMID 17932496.
- ↑ Jayasekera, S.; Sissons, J.; Tucker, J.; Rogers, C.; Nolder, D.; Warhurst, D.; Alsam, S.; White, J. M.; Higgins, E. M.; Khan, N. A. (2004). "Post-mortem culture of Balamuthia mandrillaris from the brain and cerebrospinal fluid of a case of granulomatous amoebic meningoencephalitis, using human brain microvascular endothelial cells". Journal of Medical Microbiology. 53 (Pt 10): 1007–1012. doi:10.1099/jmm.0.45721-0. PMID 15358823.
- ↑ Da Rocha-Azevedo, B.; Tanowitz, H.; Marciano-Cabral, F. (2009). "Diagnosis of infections caused by pathogenic free-living amoebae". Interdisciplinary Perspectives on Infectious Diseases. 2009: 1–14. doi:10.1155/2009/251406. PMC 2719787. PMID 19657454.
- ↑ Matin, A.; Siddiqui, R.; Jung, S.; Kim, K.; Stins, M.; Khan, N. (2007). "Balamuthia mandrillaris interactions with human brain microvascular endothelial cells in vitro". Journal of Medical Microbiology. 56 (Pt 8): 1110–1115. doi:10.1099/jmm.0.47134-0. PMID 17644721.
- ↑ Siddiqui, R.; Khan, N. (2008). "Balamuthia amoebic encephalitis: an emerging disease with fatal consequences". Microbial Pathogenesis. 44 (2): 89–97. doi:10.1016/j.micpath.2007.06.008. PMID 17913450.
- ↑ Schuster, F.; Yagi, S.; Gavali, S.; Michelson, D.; Raghavan, R.; Blomquist, I.; Glastonbury, C.; Bollen, A.; Scharnhorst, D.; Reed, S. L.; Kuriyama, S.; Visvesvara, G. S.; Glaser, C. A. (2009). "Under the radar: balamuthia amebic encephalitis". Clinical Infectious Diseases. 48 (7): 879–887. doi:10.1086/597260. PMID 19236272.
- ↑ "CDC - Acanthamoeba Infection - Epidemiology & Risk Factors". www.cdc.gov. 29 December 2021. Archived from the original on 6 June 2022. Retrieved 5 August 2022.
- ↑ Matsui, Takahiro; Maeda, Tetsuo; Kusakabe, Shinsuke; Arita, Hideyuki; Yagita, Kenji; Morii, Eiichi; Kanakura, Yuzuru (2018-05-10). "A case report of granulomatous amoebic encephalitis by Group 1 Acanthamoeba genotype T18 diagnosed by the combination of morphological examination and genetic analysis". Diagnostic Pathology. 13 (1): 27. doi:10.1186/s13000-018-0706-z. ISSN 1746-1596. PMC 5943995. PMID 29747695.
- ↑ 11.0 11.1 "Final Diagnosis - Case 156". Archived from the original on 2020-08-11. Retrieved 2022-06-30.
- ↑ Akpek, G; Uslu, A (August 2011). "Granulomatous amebic encephalitis: an under-recognized cause of infectious mortality after hematopoietic stem cell transplantation". Transpl Infect Dis. 13 (4): 366–373. doi:10.1111/j.1399-3062.2011.00612.x. PMID 21338461. S2CID 31162954. Archived from the original on December 9, 2021. Retrieved December 9, 2021.
- ↑ Deetz TR, Sawyer MH, Billman G, Schuster FL, Visvesvara GS (2003). "Successful treatment of Balamuthia amoebic encephalitis: presentation of 2 cases". Clinical Infectious Diseases. 37 (10): 1304–12. doi:10.1086/379020. PMID 14583863.
- ↑ Intalapaporn P, Suankratay C, Shuangshoti S, Phantumchinda K, Keelawat S, Wilde H (1 June 2004). "Balamuthia mandrillaris meningoencephalitis: the first case in southeast Asia". Am. J. Trop. Med. Hyg. 70 (6): 666–9. doi:10.4269/ajtmh.2004.70.666. PMID 15211011.
- ↑ "CDC - Sappinia - Frequently Asked Questions (FAQs)". Archived from the original on 2011-10-18.
External links
| Classification |
|---|