Gestational hypertension
| Gestational hypertension | |
|---|---|
| Other names: Pregnancy-induced hypertension; transient hypertension of pregnancy; chronic hypertension identified in the latter half of pregnancy[1] | |
 | |
| Micrograph showing hypertrophic decidual vasculopathy, the histomorphologic correlate of gestational hypertension. H&E stain. | |
| Specialty | Obstetrics |
| Symptoms | None[2] |
| Complications | Pre-eclampsia, long-term high blood pressure[3] |
| Usual onset | After 20 weeks of pregnancy[3] |
| Causes | Unclear[4] |
| Risk factors | Overweight, anemia, diabetes, older age, first pregnancy, multiple pregnancy[5] |
| Diagnostic method | BP>140/90 mmHg, at least 4 hrs apart, which was previously normal[3][2] |
| Treatment | Frequent checking of blood pressure, blood pressure medication, delivery[3][2] |
| Frequency | 1.8 and 4.4% of pregnancies[5] |
Gestational hypertension, also known as pregnancy-induced hypertension (PIH), is new high blood pressure in pregnancy after 20 weeks' gestation without signs of pre-eclampsia such as protein in the urine.[6][3][2] There are no specific symptoms.[2] Complications can include pre-eclampsia; which occurs in about 30%, otherwise outcomes are generally good.[3][1]
The cause is unclear.[4] Risk factors include being overweight, anemia, diabetes, older age, first pregnancy, and a multiple pregnancy.[5] It is defined as having a blood pressure (BP) greater than 140/90 mmHg on two occasions at least 4 hours apart.[3][2] If greater than 160/110 mmHg, diagnosis can be made based on blood pressures 15 minutes apart.[2][7] If the blood pressure remains high more than 12 weeks after delivery the diagnosis changes to chronic hypertension.[8]
Management involves frequent checking of blood pressure and for signs of pre-eclampsia and deliver at 37 weeks; though in certain cases this may be recommended at 34 weeks.[3][7][9] If BP is greater than 160/110 mmHg active treatment is recommended with labetolol, hydralazine, or nifedipine.[2][7][1] Generally it goes away after birth; though, there remains an increased risk of long-term high blood pressure.[10] It occurs in between 1.8 and 4.4% of pregnancies.[5]
Signs and symptoms
No test exists to predict the likelihood of developing gestational hypertension. High blood pressure is the major sign, with generally no symptoms.[11]
Complications may include pre-eclampsia which may result in:[11]
- Swelling
- Sudden weight gain
- Blurred vision or sensitivity to light
- Nausea and vomiting
- Persistent headaches
Risk factors
Maternal causes
- Obesity
- Mothers under 20 or over 40 years old[12]
- Past history of diabetes mellitus, hypertension (particularly gestational hypertension) and renal disease[12]
- Pre-existing hypertension[12]
- Thrombophilias (anti-phospholipid syndrome, protein C/S deficiency, factor V Leiden)
- Having donated a kidney[13]
Pregnancy
- Multiple gestation (twins or triplets, etc.)[12]
- Placental abnormalities:
- Hyperplacentosis: Excessive exposure to chorionic villi
- Placental ischemia
Family history
Diagnosis
Conditions
There are several hypertensive states of pregnancy:
- Gestational hypertension
- Gestational hypertension is usually defined as having a blood pressure higher than 140/90 measured on two separate occasions, more than 6 hours apart, without the presence of protein in the urine and diagnosed after 20 weeks of gestation.[14]
- Pre-eclampsia
- Pre-eclampsia is gestational hypertension plus proteinuria (>300 mg of protein in a 24-hour urine sample). Severe pre-eclampsia involves a blood pressure greater than 160/110, with additional medical signs and symptoms. HELLP syndrome is a type of pre-eclampsia. It is a combination of three medical conditions: hemolytic anemia, elevated liver enzymes and low platelet count.[citation needed]
- Eclampsia
- This is when tonic-clonic seizures appear in a pregnant woman with high blood pressure and proteinuria.
Pre-eclampsia and eclampsia are sometimes treated as components of a common syndrome.[15]
Treatment
There is often no specific treatment, but is monitored closely to identify pre-eclampsia (HELLP syndrome and eclampsia).
Drug treatment options are limited, as many antihypertensives may negatively affect the fetus. ACE inhibitors, angiotensin receptor blockers, and direct renin inhibitors are contraindicated in pregnancy as they are teratogenic. Methyldopa, hydralazine, nifedipine, and labetalol are most commonly used for severe pregnancy hypertension.[16]
The fetus is at increased risk for a variety of life-threatening conditions, including pulmonary hypoplasia (immature lungs). If the dangerous complications appear after the fetus has reached a point of viability, even though still immature, then an early delivery may be warranted to save the lives of both mother and baby. An appropriate plan for labor and delivery includes selection of a hospital with provisions for advanced life support of newborn babies.[citation needed]
Evolutionary considerations
Gestational hypertension is one of the most common disorders seen in pregnancies.[17] Though relatively benign on its own, in roughly half of the cases it progresses to pre-eclampsia.[18] Gestational hypertension is rare in other animals. It has been the belief of the scientific community that it was relatively unique to humans, although there has been some evidence other primates can develop similar conditions, albeit due to different mechanisms.[17] The underlying cause of gestational hypertension in humans is believed to be an improperly implanted placenta. Humans have evolved to have a very invasive placenta to facilitate better oxygen transfer from the mother to the fetus, to support the growth of its large brain.[19]
Origins of the placenta
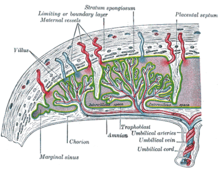
The origins of gestational hypertension may lie with the development of humans' hemochorial placenta. A hemochorial placenta optimizes the amount of oxygen and nutrients that can be absorbed into the fetal blood supply, while at the same time ensuring rapid diffusion of wastes away from the fetus. This hemochorial placenta differs from lower primates' epitheliochorial placentae in the way that it allows the fetal tissues to interact directly with the mother's blood. The hemochorial placenta thereby promotes more rapid diffusion to and from the fetal blood supply.[20]
In animals with epitheliochorial placentae such as horses and pigs, the greatest resistance to maternal blood flow in the vascular system was found within the placenta. However, in animals with hemochorial placental structures such as rodents and primates, the vascular resistance in the placenta was low, leading scientists to the conclusion that the greatest resistance to maternal blood flow is found elsewhere in the maternal vascular system.[21] The high vascular resistance outside of the placenta leads to higher maternal blood pressure throughout the body.[citation needed]
The fetal cells that implant into the uterine wall are known as the trophoblast. The hemochorial placenta bathes the fetal trophoblast in maternal blood by forming lacunae, or lakes, of the mother's blood that surround fetal tissue. The lacunae are filled by the spiral arteries, which means that the mother's blood pressure is the driving force behind the introduction of new blood, which contains both oxygen and food for the fetus, to the system.[22] It is thought that humans need the increased diffusion provided by the hemochorial placenta in order to grow the large brains compared to their body size that distinguish them from other primates.[23]
Incorrect placental implantation
It is thought that "failings" in normal hemochorial placental structure lead to pre-eclampsia and gestational hypertension.[24] The human placenta implants "earlier, deeper, and more extensively" into the uterine wall, which can potentially lead to many problems that are found in human pregnancies, but not as much in other animals. Miscarriage and pre-eclampsia are both very rare in other species, but are two of the most common pregnancy-related diseases in humans.[25] The genetic roots of gestational hypertension and pre-eclampsia are certain, as women with a family history of the condition are three times more likely to develop it when they are pregnant.[26]
One of the potential causes of gestational hypertension and pre-eclampsia is when the trophoblast does not invade far enough into the uterine lining.[27] When the fetus's trophoblast does not fully extend into the uterine wall, the spiral arteries do not become fully converted into low-resistance channels.[25] It has been found that this incomplete conversion of spiral arteries increases the resistance to uterine blood flow during pregnancy, and that this occurrence was associated with gestational hypertension.[28] One potential cause of this incomplete breach of the spiral arteries that leads to gestational hypertension is a mistaken immune response by the maternal tissue, reaction to the alien fetal tissue.[29] Therefore, it is clear that the complication of gestational hypertension has roots in the early implantation of the fetus in the uterine wall, an implantation technique that is unique to humans.[citation needed]
The highly invasive placenta that is found in humans is thought to be linked to humans' high circulating levels of the hormones CG and hCG. It has been shown that the higher the levels of these hormones, the deeper the trophoblast's invasion into the uterine wall. Instances of gestational hypertension and pre-eclampsia have been shown to occur when the invasion of the uterine wall is not deep enough, because of lower CG and hCG levels in the mother.[30]
Evolutionary tradeoff
Despite these risks for gestational hypertension, the hemochorial placenta has been favored because of its advantages in the way that it aids in diffusion from mother to fetus later in pregnancy. The bipedal posture that has allowed humans to walk upright has also led to a reduced cardiac output, and it has been suggested that this is what necessitated humans' aggressive early placental structures.[31] Increased maternal blood pressure can attempt to make up for lower cardiac output, ensuring that the fetus's growing brain receives enough oxygen and nutrients.[30] The benefits of being able to walk upright and run on land have outweighed the disadvantages that come from bipedalism, including the placental diseases of pregnancy, such as gestational hypertension. Similarly, the advantages of having a large brain size have outweighed the deleterious effects of having a placenta that does not always convert the spiral arteries effectively, leaving humans vulnerable to contracting gestational hypertension. It is speculated that this was not the case with Neanderthals, and that they died out because their cranial capacity increased too much, and their placentae were not equipped to handle the fetal brain development, leading to widespread pre-eclampsia and maternal and fetal death.[32]
Gestational hypertension in the early stages of pregnancy (trimester 1) has been shown to improve the health of the child both in its first year of life, and its later life.[33] However, when the disease develops later in the pregnancy (subsequent trimesters), or turns into pre-eclampsia, there begin to be detrimental health effects for the fetus, including low birth-weight.[18] It has been proposed that fetal genes designed to increase the mother's blood pressure are so beneficial that they outweigh the potential negative effects that can come from pre-eclampsia.[33] It has also been suggested that gestational hypertension and pre-eclampsia have remained active traits due to the cultural capacity of humans, and the tendency for midwives or helpers to aid in delivering babies.[34]
Relevance of evolutionary history
It is the goal of evolutionary medicine to find treatments for diseases that are informed by the evolutionary history of a disease. It has been suggested that gestational hypertension is linked to insulin resistance during pregnancy.[35] Both the increase in blood sugar that can lead to gestational diabetes and the increase in blood pressure that can lead to gestational hypertension are mechanisms that mean to optimize the amount of nutrients that can be passed from maternal tissue to fetal tissue. It has been suggested that techniques used to combat insulin insensitivity might also prove beneficial to those with gestational hypertension.[35] Measures to avoid insulin resistance include avoiding obesity before pregnancy, minimizing weight gain during pregnancy, eating foods with low glycemic indices, and exercising.[35]
References
- ↑ 1.0 1.1 1.2 "Hypertension and Pregnancy: Overview, Chronic Hypertension, Differential Diagnosis". 18 July 2022. Archived from the original on 4 April 2019. Retrieved 16 March 2024.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 Luger, RK; Kight, BP (January 2024). "Hypertension In Pregnancy". StatPearls. PMID 28613589. Archived from the original on 31 March 2023. Retrieved 14 March 2024.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 "Preeclampsia and High Blood Pressure During Pregnancy". www.acog.org. Archived from the original on 8 March 2024. Retrieved 14 March 2024.
- ↑ 4.0 4.1 "Gestational Hypertension". healthlibrary.uwmedicine.org. Archived from the original on 3 February 2023. Retrieved 16 March 2024.
- ↑ 5.0 5.1 5.2 5.3 Umesawa, M; Kobashi, G (March 2017). "Epidemiology of hypertensive disorders in pregnancy: prevalence, risk factors, predictors and prognosis". Hypertension research : official journal of the Japanese Society of Hypertension. 40 (3): 213–220. doi:10.1038/hr.2016.126. PMID 27682655.
- ↑ "40". Williams obstetrics (24th ed.). McGraw-Hill Professional. 2014. ISBN 9780071798938.
- ↑ 7.0 7.1 7.2 "Gestational Hypertension and Preeclampsia: ACOG Practice Bulletin Summary, Number 222". Obstetrics and gynecology. 135 (6): 1492–1495. June 2020. doi:10.1097/AOG.0000000000003892. PMID 32443077.
- ↑ Wilkerson, RG; Ogunbodede, AC (May 2019). "Hypertensive Disorders of Pregnancy". Emergency medicine clinics of North America. 37 (2): 301–316. doi:10.1016/j.emc.2019.01.008. PMID 30940374.
- ↑ Leeman, L; Dresang, LT; Fontaine, P (15 January 2016). "Hypertensive Disorders of Pregnancy". American family physician. 93 (2): 121–7. PMID 26926408.
- ↑ "High Blood Pressure During Pregnancy". Centers for Disease Control and Prevention. 19 June 2023. Archived from the original on 8 March 2024. Retrieved 14 March 2024.
- ↑ 11.0 11.1 "Gestational Hypertension". www.stanfordchildrens.org. Stanford Medicine Children's Health. Archived from the original on 2023-12-06. Retrieved 2023-10-07.
- ↑ 12.0 12.1 12.2 12.3 "Gestational Hypertension". Stanford Children's Health. Archived from the original on 2017-12-01. Retrieved 2017-11-30.
- ↑ Garg AX, Nevis IF, McArthur E, Sontrop JM, Koval JJ, Lam NN, Hildebrand AM, Reese PP, Storsley L, Gill JS, Segev DL, Habbous S, Bugeja A, Knoll GA, Dipchand C, Monroy-Cuadros M, Lentine KL (January 2015). "Gestational hypertension and preeclampsia in living kidney donors". N. Engl. J. Med. 372 (2): 124–33. doi:10.1056/NEJMoa1408932. PMC 4362716. PMID 25397608.
- ↑ Lo, JO; Mission, JF; Caughey, AB (April 2013). "Hypertensive disease of pregnancy and maternal mortality". Current Opinion in Obstetrics and Gynecology. 25 (2): 124–32. doi:10.1097/gco.0b013e32835e0ef5. PMID 23403779. S2CID 246228.
- ↑ "preeclampsia/eclampsia" at Dorland's Medical Dictionary
- ↑ Brown CM, Garovic VD (March 2014). "Drug Treatment of Hypertension in Pregnancy". Drugs. 74 (3): 283–296. doi:10.1007/s40265-014-0187-7. PMC 4558097. PMID 24554373.
- ↑ 17.0 17.1 Abrams ET, Rutherford JN (2011). "Framing postpartum hemorrhage as a consequence of human placental biology: an evolutionary and comparative perspective". American Anthropologist. 113 (3): 417–30. doi:10.1111/j.1548-1433.2011.01351.x. PMC 3168987. PMID 21909154.
- ↑ 18.0 18.1 Barton JR, O'brien JM, Bergauer NK, Jacques DL, Sibai BM (April 2001). "Mild gestational hypertension remote from term: progression and outcome". Am. J. Obstet. Gynecol. 184 (5): 979–83. doi:10.1067/mob.2001.112905. PMID 11303208.
- ↑ Rosenberg KR, Trevathan WR (December 2007). "An anthropological perspective on the evolutionary context of preeclampsia in humans". J. Reprod. Immunol. 76 (1–2): 91–7. doi:10.1016/j.jri.2007.03.011. PMID 17499857.
- ↑ Campbell, Bernard Grant. "Reproduction and the Placenta." Human Evolution: An Introduction to Man's Adaptations. New York: Aldine De Gruyter, 1998. 317-20.
- ↑ Moll W, Künzel W (January 1973). "The blood pressure in arteries entering the placentae of guinea pigs, rats, rabbits, and sheep". Pflügers Arch. 338 (2): 125–31. doi:10.1007/bf00592748. PMID 4734441. S2CID 24904753.
- ↑ Ahokas RA, McKinney ET (2009). "Development and Physiology of the Placenta and Membranes". The Global Library of Women's Medicine. doi:10.3843/GLOWM.10101. ISSN 1756-2228.
- ↑ Martin RD (August 2003). "Human reproduction: a comparative background for medical hypotheses". J. Reprod. Immunol. 59 (2): 111–35. doi:10.1016/s0165-0378(03)00042-1. PMID 12896817.
- ↑ Cross JC (2003). "The Genetics of Pre-eclampsia: A Feto-placental or Maternal Problem?". Clinical Genetics. 64 (2): 96–103. doi:10.1034/j.1399-0004.2003.00127.x. PMID 12859402. S2CID 23691148.
- ↑ 25.0 25.1 Jauniaux E, Poston L, Burton GJ (2006). "Placental-related diseases of pregnancy: Involvement of oxidative stress and implications in human evolution". Hum. Reprod. Update. 12 (6): 747–55. doi:10.1093/humupd/dml016. PMC 1876942. PMID 16682385.
- ↑ Duckitt K, Harrington D (March 2005). "Risk factors for pre-eclampsia at antenatal booking: systematic review of controlled studies". BMJ. 330 (7491): 565. doi:10.1136/bmj.38380.674340.E0. PMC 554027. PMID 15743856.
- ↑ Norwitz ER (October 2006). "Defective implantation and placentation: laying the blueprint for pregnancy complications". Reprod. Biomed. Online. 13 (4): 591–9. doi:10.1016/s1472-6483(10)60649-9. PMID 17007686.
- ↑ Olofsson P, Laurini RN, Marsál K (May 1993). "A high uterine artery pulsatility index reflects a defective development of placental bed spiral arteries in pregnancies complicated by hypertension and fetal growth retardation". Eur. J. Obstet. Gynecol. Reprod. Biol. 49 (3): 161–8. doi:10.1016/0028-2243(93)90265-e. PMID 8405630.
- ↑ Robertson WB, Brosens I, Dixon G (1976). "Maternal uterine vascular lesions in the hypertensive complications of pregnancy". Perspect Nephrol Hypertens. 5: 115–27. PMID 1005030.
- ↑ 30.0 30.1 Cole LA (November 2009). "hCG and hyperglycosylated hCG in the establishment and evolution of hemochorial placentation". J. Reprod. Immunol. 82 (2): 112–18. doi:10.1016/j.jri.2009.04.007. PMID 19560212.
- ↑ Rockwell LC, Vargas E, Moore LG (2003). "Human physiological adaptation to pregnancy: inter- and intraspecific perspectives". Am. J. Hum. Biol. 15 (3): 330–41. doi:10.1002/ajhb.10151. PMID 12704709. S2CID 19806255.
- ↑ Chaline J (August 2003). "Increased cranial capacity in hominid evolution and preeclampsia". J. Reprod. Immunol. 59 (2): 137–52. doi:10.1016/s0165-0378(03)00043-3. PMID 12896818.
- ↑ 33.0 33.1 Hollegaard B, Byars SG, Lykke J, Boomsma JJ (2013). "Parent-offspring conflict and the persistence of pregnancy-induced hypertension in modern humans". PLOS ONE. 8 (2): e56821. Bibcode:2013PLoSO...856821H. doi:10.1371/journal.pone.0056821. PMC 3581540. PMID 23451092.
- ↑ Rosenberg Karen R.; Trevathan Wenda R. (2007). "An Anthropological Perspective on the Evolutionary Context of Preeclampsia in Humans". Journal of Reproductive Immunology. 76 (1–2): 91–97. doi:10.1016/j.jri.2007.03.011. PMID 17499857.
- ↑ 35.0 35.1 35.2 Solomon CG, Seely EW (February 2001). "Brief review: hypertension in pregnancy : a manifestation of the insulin resistance syndrome?". Hypertension. 37 (2): 232–9. doi:10.1161/01.hyp.37.2.232. PMID 11230277.
| Classification | |
|---|---|
| External resources |