Epidermodysplasia verruciformis
| Epidermodysplasia verruciformis | |
|---|---|
| Other names: Lewandowsky–Lutz dysplasia, treeman syndrome | |
 | |
| Pityriasis versicolor-like pale spots and small bumps in typical epidermodysplasia verruciformis | |
| Specialty | Dermatology |
| Symptoms | Scaly warty spots and small bumps, chiefly on the hands, feet, face, neck[1] |
| Complications | Disfigurement, squamous cell skin cancer[1] |
| Usual onset | Children, young adults[1] |
| Duration | Lifelong |
| Types | Typical, atypical, acquired[2] |
| Causes | Inherited most commonly by autosomal recessive trait, acquired immunodeficiency[2] |
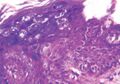
| Diagnostic method | Visualisation, skin biopsy, molecular analysis[3] |
| Prevention | Sun protection to prevent skin cancer[1] |
| Treatment | Surgery, ALA-PDT (photodynamic therapy with aminolevulinic acid)[1] |
| Medication | Applying 5-FU or imiquimod, retinoids by mouth[1] |
| Prognosis | Recurs on stopping treatment[1] |
| Frequency | Rare[1] |
Epidermodysplasia verruciformis (EV) is a skin condition characterised by warty skin lesions.[1] It results from an abnormal susceptibility to HPV infection (HPV) and is associated with a high lifetime risk of squamous cell carcinomas in skin.[1] It generally presents with scaly spots and small bumps particularly on the hands, feet, face and neck; typically beginning in childhood or in a young adult.[1] The bumps tend to be flat, grow in number and then merge to form plaques.[1] On the trunk, it typically appears like pityriasis versicolor; lesions there being slightly scaly and tan, brown, red or looking pale.[1] On the elbows, it may appear like psoriasis.[1] On the forehead, neck and trunk, the lesions may appear like seborrheic keratosis.[1]
It is most frequently inherited as an autosomal recessive trait, with some reports of autosomal dominant and X-linked inheritance.[1][2] Other types include atypical EV which develops due to gene mutations that cause an impaired immune system, and acquired EV which occurs due to acquired immunodeficiency.[2][4] It is characterized by an inability to protect against HPV infection of skin.[3][5] HPV types 5 and 8 are detected in around 90% of skin cancers in people with EV.[1] Other types that are associated with EV include 3, 4, 5, 8, 9, 10, 12, 14, 15 and 17, 19-25, 36-38, and 47.[1] In rare cases, the warts may develop into giant horns resulting in treeman syndrome.[6]
Diagnosis is based on clinical findings, appearance of histopathology from skin biopsy, and molecular analysis.[3] Prevention of skin cancer requires sun protection.[1] Treatment typically involves surgery; sometimes with the addition of skin grafting.[1] Medications used to treat the lesions include ALA-PDT (photodynamic therapy with aminolevulinic acid), applying 5-FU, imiquimod, and retinoids by mouth.[1] The lesions tend to recur on stopping treatment.[1]
The condition is rare.[1] The lesions have been noted to occur at a younger age in warmer climates.[1] EV associated skin cancer develops less frequently in Africans.[1] The condition was first described by Felix Lewandowsky and Wilhelm Lutz in 1922.[7]
Signs and symptoms
It generally presents with scaly spots and small bumps particularly on the hands, feet, face and neck; typically beginning in childhood or in a young adult.[1] The bumps tend to be flat, grow in number and then merge to form plaques.[1] On the trunk, it typically appears like pityriasis versicolor; lesions there being slightly scaly and tan, brown, red or looking pale.[1] On the elbows, it may appear like psoriasis.[1] On the forehead, neck and trunk, the lesions may appear like seborrheic keratosis.[1]
-
Epidermodysplasia verruciformis in a young man with HIV
-
Epidermodysplasia verruciformis in a young man with HIV
Cause
Genetics
The cause of the condition is an inactivating PH mutation in either the EVER1 or EVER2 genes, which are located adjacent to one another on chromosome 17.[7] These genes play a role in regulating the distribution of zinc in the cell nuclei. Zinc is a necessary cofactor for many viral proteins, and the activity of EVER1/EVER2 complex appears to restrict the access of viral proteins to cellular zinc stores, limiting their growth.[8]
Other genes have also rarely been associated with this condition. These include the ras homolog gene family member H.[9]
Diagnosis
Diagnosis is based on clinical findings, appearance of histopathology from skin biopsy, and molecular analysis.[3]
Treatment

Prevention of skin cancer requires sun protection.[1] Treatment typically involves surgery; sometimes with the addition of skin grafting.[1] Medications used to treat the lesions include ALA-PDT (photodynamic therapy with aminolevulinic acid), applying 5-FU, imiquimod, and retinoids by mouth.[1] The lesions tend to recur on stopping treatment.[1]
Zinc therapy has also been effective in the treatment of those individuals affected by Epidermodysplasia verruciformis[10]
History
The condition was first described by Felix Lewandowsky and Wilhelm Lutz in 1922.[7][11] In 1939 Sullivan and Ellis noted the association between EV and a high risk of skin cancer.[7]
Other images
-
Abul Bajandar from Bangladesh
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 1.18 1.19 1.20 1.21 1.22 1.23 1.24 1.25 1.26 1.27 1.28 1.29 1.30 1.31 1.32 1.33 James, William D.; Elston, Dirk; Treat, James R.; Rosenbach, Misha A.; Neuhaus, Isaac (2020). "19. Viral diseases: epidermodysplasia verruciformis". Andrews' Diseases of the Skin: Clinical Dermatology (13th ed.). Edinburgh: Elsevier. pp. 411–412. ISBN 978-0-323-54753-6. Archived from the original on 2023-03-19. Retrieved 2023-03-19.
- ↑ 2.0 2.1 2.2 2.3 Shimizu, Akira; Yamaguchi, Reimon; Kuriyama, Yuko (March 2023). "Recent advances in cutaneous HPV infection". The Journal of Dermatology. 50 (3): 290–298. doi:10.1111/1346-8138.16697. ISSN 1346-8138. PMID 36601717. Archived from the original on 2023-03-19. Retrieved 2023-03-19.
- ↑ 3.0 3.1 3.2 3.3 Myers, David J.; Kwan, Eddie; Fillman, Eric P. (2022). "Epidermodysplasia Verruciformis". StatPearls. StatPearls Publishing. PMID 30480937.
- ↑ Moore, Stephen; Rady, Peter; Tyring, Stephen (November 2022). "Acquired epidermodysplasia verruciformis: clinical presentation and treatment update". International Journal of Dermatology. 61 (11): 1325–1335. doi:10.1111/ijd.15857. ISSN 1365-4632. Archived from the original on 2023-03-19. Retrieved 2023-03-19.
- ↑ Mogensen, Trine H. (November 2022). "Genetic susceptibility to viral disease in humans". Clinical Microbiology and Infection: The Official Publication of the European Society of Clinical Microbiology and Infectious Diseases. 28 (11): 1411–1416. doi:10.1016/j.cmi.2022.02.023. ISSN 1469-0691. PMID 35218976. Archived from the original on 2022-12-04. Retrieved 2023-03-19.
- ↑ Uitto, Jouni; Saeidian, Amir Hossein; Youssefian, Leila; Saffarian, Zahra; Casanova, Jean-Laurent; Béziat, Vivien; Jouanguy, Emmanuelle; Vahidnezhad, Hassan (May 2022). "Recalcitrant Warts, Epidermodysplasia Verruciformis, and the Tree-Man Syndrome: Phenotypic Spectrum of Cutaneous Human Papillomavirus Infections at the Intersection of Genetic Variability of Viral and Human Genomes". The Journal of Investigative Dermatology. 142 (5): 1265–1269. doi:10.1016/j.jid.2021.10.029. ISSN 1523-1747. PMID 34843682. Archived from the original on 2023-03-20. Retrieved 2023-03-20.
- ↑ 7.0 7.1 7.2 7.3 Emsen, IM; Kabalar, ME (2010). "Epidermodysplasia verruciformis: An early and unusual presentation". The Canadian journal of plastic surgery = Journal canadien de chirurgie plastique. 18 (1): 21–4. PMID 21358870. Archived from the original on 2021-05-19. Retrieved 2023-03-21.
- ↑ Lazarczyk M, Favre M (December 2008). "Role of Zn2+ ions in host-virus interactions". Journal of Virology. 82 (23): 11486–94. doi:10.1128/JVI.01314-08. PMC 2583646. PMID 18787005.
- ↑ Crequer, Amandine; Troeger, Anja; Patin, Etienne; Ma, Cindy; Picard, Capucine; Pedergnana, Vincent; Fieschi, Claire; Lim, Annick; Abhyankar, Avinash; Gineau, Laure; Mueller-Fleckenstein, Ingrid; Schmidt, Monika; Taieb, Alain; Krueger, James; Abel, Laurent; Tangye, Stuart; Orth, Gérard; Williams, David; Casanova, Jean-Laurent; Jouanguy, Emmanuelle (2012-08-01). "Human RHOH deficiency causes T cell defects and susceptibility to EV-HPV infections". The Journal of Clinical Investigation. 122 (9): 3239–3247. doi:10.1172/JCI62949. PMC 3428089. PMID 22850876.
- ↑ Lebwohl, Mark G.; Heymann, Warren R.; Berth-Jones, John; Coulson, Ian (2017). "Epidermodysplasia verruciformis". Treatment of Skin Disease: Comprehensive Therapeutic Strategies. Elsevier. p. 225. ISBN 978-0-7020-6913-0. Archived from the original on 2023-03-21. Retrieved 2023-03-21.
- ↑ Lewandowsky F, Lutz W (October 1922). "Ein Fall einer bisher nicht beschriebenen Hauterkrankung (Epidermodysplasia verruciformis)". Archiv für Dermatologie und Syphilis (in Deutsch). 141 (2): 193–203. doi:10.1007/BF01938833. S2CID 8585441. Archived from the original on 2021-09-23. Retrieved 2021-07-14.
External links
| Classification | |
|---|---|
| External resources |