Eosinophilic folliculitis
| Eosinophilic folliculitis | |
|---|---|
| Other names: Eosinophilic pustular folliculitis, Sterile eosinophilic pustulosis"[1] | |
| Specialty | Dermatology |
Eosinophilic folliculitis is an itchy rash with an unknown cause that is most common among individuals with HIV, though it can occur in HIV-negative individuals where it is known by the eponym Ofuji disease.[2] EF consists of itchy red bumps (papules) centered on hair follicles and typically found on the upper body, sparing the abdomen and legs. The name eosinophilic folliculitis refers to the predominant immune cells associated with the disease (eosinophils) and the involvement of the hair follicles.
Pathophysiology
The cause of EF is unknown. A variety of microorganisms have been implicated, including the mite Demodex,[3] the yeast Pityrosporum,[4] and bacteria.[5] An autoimmune process has what is this also been investigated.[6]
-
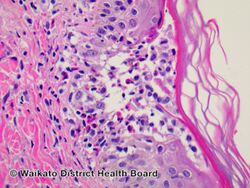
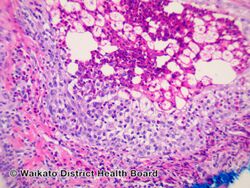
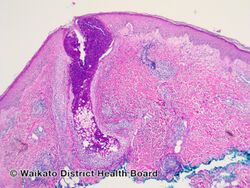
Eosinophilic folliculitis/pathology
-
Eosinophilic folliculitis/pathology
-
Eosinophilic folliculitis/pathology
-
Eosinophilic folliculitis/pathology
Diagnosis
Eosinophilic folliculitis may be suspected clinically when an individual with HIV exhibits the classic symptoms. The diagnosis can be supported by the finding of eosinophilia but a skin biopsy is necessary to establish it. Skin biopsies reveal lymphocytic and eosinophilic inflammation around the hair follicles.
Treatment
Treatment of eosinophilic folliculitis in people with HIV typically begins with the initiation of Highly Active Anti-Retroviral Therapy in order to help reconstitute the immune system. Direct treatment of the EF itself focuses on decreasing the inflammation and itching. Topical corticosteroids and oral antihistamines can alleviate the itching and decrease the size and number of lesions. Treatment with the antifungal drug itraconazole, the antibiotic metronidazole, and the anti-mite drug permethrin may lead to some improvement of symptoms. Other therapies include PUVA, topical tacrolimus, and isotretinoin.[7]
Epidemiology
Eosinophilic folliculitis associated with HIV infection typically affects individuals with advanced HIV and low T helper cell counts.[8] It affects both men and women as well as children with HIV and is found throughout the world.
EF may also affect individuals with hematologic disease such as leukemia and lymphoma.[9] It may also affect otherwise normal infants in a self-limited form.[10] HIV-negative individuals can also develop EF — this is more common in Japan.[11]
Additional images
-
Eosinophilic folliculitis
-
Eosinophilic folliculitis
-
Eosinophilic folliculitis
See also
References
- ↑ James, William D.; Elston, Dirk; Treat, James R.; Rosenbach, Misha A.; Neuhaus, Isaac (2020). "10. Seborrheic dermatitis, psoriasis, recalcitrant palmopustular eruptions, pustular dermatitis, and erythroderma". Andrews' Diseases of the Skin: Clinical Dermatology (13th ed.). Edinburgh: Elsevier. p. 202. ISBN 978-0-323-54753-6. Archived from the original on 2022-06-11. Retrieved 2022-06-02.
- ↑ Ofuji, S; Ogino, A; Horio, T; Oseko, T; Uehara, M (1970). "Eosinophilic pustular folliculitis". Acta Dermato-venereologica. 50 (3): 195–203. PMID 4193219.
- ↑ Bodokh, I; Lacour, JP; Perrin, C; Bourdet, JF; Ortonne, JP (1994). "Papular eruption in AIDS: role of demodectic mites?". Acta Dermato-venereologica. 74 (4): 320–2. doi:10.2340/0001555574320322 (inactive 31 May 2021). PMID 7976100.
{{cite journal}}: CS1 maint: DOI inactive as of May 2021 (link) - ↑ Ferrándiz, C; Ribera, M; Barranco, JC; Clotet, B; Lorenzo, JC (1992). "Eosinophilic pustular folliculitis in patients with acquired immunodeficiency syndrome". International Journal of Dermatology. 31 (3): 193–5. doi:10.1111/j.1365-4362.1992.tb03934.x. PMID 1568818. S2CID 1196523.
- ↑ Smith, KJ; Skelton, HG; Yeager, J; Ruiz, N; Wagner, KF (1995). "Metronidazole for eosinophilic pustular folliculitis in human immunodeficiency virus type 1-positive patients". Archives of Dermatology. 131 (9): 1089–91. doi:10.1001/archderm.131.9.1089. PMID 7661619.
- ↑ Fearfield, LA; Rowe, A; Francis, N; Bunker, CB; Staughton, RC (1999). "Itchy folliculitis and human immunodeficiency virus infection: clinicopathological and immunological features, pathogenesis and treatment". The British Journal of Dermatology. 141 (1): 3–11. doi:10.1046/j.1365-2133.1999.02914.x. PMID 10417509. S2CID 12727217.
- ↑ Ellis, E; Scheinfeld, N (2004). "Eosinophilic pustular folliculitis: a comprehensive review of treatment options". American Journal of Clinical Dermatology. 5 (3): 189–97. doi:10.2165/00128071-200405030-00007. PMID 15186198. S2CID 72079927.
- ↑ Parker, SR; Parker, DC; McCall, CO (2006). "Eosinophilic folliculitis in HIV-infected women: case series and review". American Journal of Clinical Dermatology. 7 (3): 193–200. doi:10.2165/00128071-200607030-00006. PMID 16734507. S2CID 71615655.
- ↑ Patrizi, A; Chieregato, C; Visani, G; Morrone, P; Patrone, P (2004). "Leukaemia-associated eosinophilic folliculitis (Ofuji's disease)". Journal of the European Academy of Dermatology and Venereology. 18 (5): 596–8. doi:10.1111/j.1468-3083.2004.00982.x. PMID 15324404. S2CID 45311563.
- ↑ Buckley, DA; Munn, SE; Higgins, EM (2001). "Neonatal eosinophilic pustular folliculitis". Clinical and Experimental Dermatology. 26 (3): 251–5. doi:10.1046/j.1365-2230.2001.00807.x. PMID 11422167. S2CID 36497326.
- ↑ Teraki, Y; Nishikawa, T (2005). "Skin diseases described in Japan 2004". Journal der Deutschen Dermatologischen Gesellschaft. 3 (1): 9–25. doi:10.1046/j.1439-0353.2005.04076.x. PMID 16353745. S2CID 26787648.
External links
| External resources |
|---|