Ectopic thymus
| Ectopic thymus | |
|---|---|
| Specialty | Otorhinolaryngology |
| Symptoms | neck mass, sometimes hoarse voice, stridor, shortness of breath, dysphagia |
| Causes | embryological defect of movement of thymus tissue |
| Diagnostic method | ultrasound, magnetic resonance imaging |
| Differential diagnosis | thyroglossal cyst, branchial cleft cyst, dermoid cyst, lymphadenitis, tumours |
| Treatment | surgery if symptoms, watch and wait if no symptoms |
| Prognosis | good |
| Frequency | unknown |
Ectopic thymus is a condition where thymus tissue is found in an abnormal location. It usually does not cause symptoms, but may leads to a mass in the neck that may compress the trachea and the esophagus. It is thought to be the result of either a failure of descent or a failure of involution of normal thymus tissue. It may be diagnosed with radiology, such as an ultrasound or magnetic resonance imaging. If it causes illness, surgery can be used to remove it. Recurrence after surgery is very unlikely.
Signs and symptoms
Ectopic thymus most often does not cause symptoms.[1] It is most frequently discovered as a soft mass or swelling in the neck of infants and children.[2] However, when symptoms do occur they are most commonly due to compression of nearby structures such as the trachea and esophagus. This can lead to hoarse voice, stridor, difficulty breathing and/or difficulty swallowing.[3][4] Pain is uncommon.[5]
Cause
During embryological development, the thymus is formed from the third and fourth pharyngeal pouches.[1] It descends along a pathway from the mandible to its final resting place of the mediastinum.[2] When the thymus tissue fails to descend appropriately or fails to involute, thymus tissue remains in various locations along this pathway. Locations that solid thymus tissue has been reported include near the thyroid (most common), within the thyroid, the base of the skull, and within the pharynx or trachea.[6][2]
Diagnosis
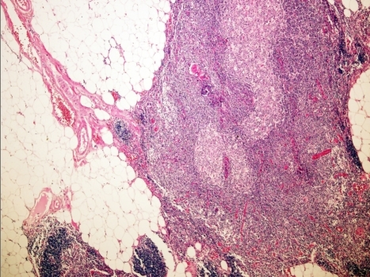
Ultrasound is the recommended diagnostic modality used to diagnose cervical ectopic thymus.[6] The thymus has a unique appearance on ultrasound, which allows for specific diagnosis.[7][8] Ectopic thymus appears hypoechoic, with characteristic linear echogenic foci.[3] Magnetic resonance imaging may be utilized as well to better characterize and identify the location of the ectopic thymus.[2] On MRI, ectopic cervical thymus appears as a homogeneous mass which is isointense to muscle on T1-weighted scans and hyperintense on T2-weighted scans.[3] Biopsy or histological examination upon resection can also be used to make a definitive diagnosis.[6][9] Sometimes, ectopic thymus is found incidentally during neck surgery.[6]
Differential diagnosis
An appropriate differential diagnosis depends upon location of the ectopic thymus. For cervical ectopic thymus, the differential diagnosis should include additional causes of neck masses. This includes common causes of neck masses in children, including:
- thyroglossal duct cyst.[6][10]
- branchial cleft cyst.[10]
- dermoid cyst.[10]
- inflammatory lymphadenitis.[10]
- salivary gland infection.[10]
- sternocleidomastoid tumor of infancy.[10]
- benign tumor.[10]
Rare causes of neck masses in children include:
Treatment
If the patient is asymptomatic and the mass is identified based upon radiologic findings, biopsy and/or resection may be avoided.[6][9] Surgical removal of the mass is the definitive treatment for ectopic thymus tissue that is causing symptoms.[4] It has been reported that the ectopic thymus tissue can transform into cancerous tissue.[4] However, due to most diagnosed ectopic thymus tissue being resected due to this concern, the natural progression is not well explored. The data supporting malignant transformation is limited, and ectopic thymus tissue that is not causing problems can likely be left to involute.[11] Given the thymus's role in the body's adaptive immune system, it should be confirmed that the patient has a mediastinal thymus prior to surgery in order to prevent the potential for future immunodeficiencies.[4]
Prognosis
Following surgical removal of the ectopic thymus, there have been no reported recurrences.[4]
Epidemiology
Because ectopic thymus usually does not cause symptoms, it is hard to determine prevalence.[1] Ectopic thymus is rarely reported in the literature.[2] The prevalence of ectopic thymus reportedly ranges from 1 to 90%. This variation in prevalence is largely dependent upon the method of investigation used and how extensive the workup is.[12] With most ectopic thymus tissue being asymptomatic, it is likely the prevalence is higher than typically reported.[3]
References
- ↑ 1.0 1.1 1.2 Grevellec, Armelle; Tucker, Abigail S. (2010-05-01). "The pharyngeal pouches and clefts: Development, evolution, structure and derivatives". Seminars in Cell & Developmental Biology. Molecular Motors in Mitosis. 21 (3): 325–332. doi:10.1016/j.semcdb.2010.01.022. ISSN 1084-9521. PMID 20144910.
- ↑ 2.0 2.1 2.2 2.3 2.4 Lavini, Corrado; Moran, Cesar A.; Morandi, Uliano; Schoenhuber, Rudolf (2009-05-08). Thymus Gland Pathology: Clinical, Diagnostic and Therapeutic Features. Springer Science & Business Media. ISBN 978-88-470-0828-1.
- ↑ 3.0 3.1 3.2 3.3 Herman, T. E.; Siegel, M. J. (February 2009). "Cervical ectopic thymus". Journal of Perinatology. 29 (2): 173–174. doi:10.1038/jp.2008.89. ISSN 1476-5543. PMID 19177048.
- ↑ 4.0 4.1 4.2 4.3 4.4 Anastasiadis, Kyriakos; Ratnatunga, Chandi (2007-06-07). The Thymus Gland: Diagnosis and Surgical Management. Springer Science & Business Media. ISBN 978-3-540-33426-2.
- ↑ De Foer, B.; Vercruysse, J. Ph.; Mariën, P.; Colpaert, C.; Pilet, B.; Pouillon, M.; Smet, M. H.; Casselman, J. W.; Breysem, L. (2007). "Cervical ectopic thymus presenting as a painless neck mass in a child". Journal of the Belgian Society of Radiology. 90: 281–283.
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 6.6 6.7 Bang, Myung Hoon; Shin, JinShik; Lee, Kwan Seop; Kang, Min Jae (2018-04-06). "Intrathyroidal ectopic thymus in children". Medicine. 97 (14): e0282. doi:10.1097/MD.0000000000010282. ISSN 0025-7974. PMC 5902273. PMID 29620644.
- ↑ Han, Bokyung K.; Yoon, H.-K.; Suh, Yeon-Lim (2001-07-01). "Thymic ultrasound". Pediatric Radiology. 31 (7): 480–487. doi:10.1007/s002470100468. ISSN 1432-1998. PMID 11486800. S2CID 2797344.
- ↑ Yildiz, Adalet Elcin; Ceyhan, Koray; Sıklar, Zeynep; Bilir, Pelin; Yağmurlu, Emin Aydın; Berberoğlu, Merih; Fitoz, Suat (September 2015). "Intrathyroidal Ectopic Thymus in Children: Retrospective Analysis of Grayscale and Doppler Sonographic Features". Journal of Ultrasound in Medicine. 34 (9): 1651–1656. doi:10.7863/ultra.15.14.10041. ISSN 1550-9613. PMID 26269296. S2CID 31698111.
- ↑ 9.0 9.1 Zielke, Anna M.; Swischuk, Leonard E.; Hernandez, J. Alberto (2007-11-01). "Ectopic cervical thymic tissue: can imaging obviate biopsy and surgical removal?". Pediatric Radiology. 37 (11): 1174–1177. doi:10.1007/s00247-007-0598-7. ISSN 1432-1998. PMID 17851657. S2CID 22161921. Archived from the original on 2022-11-15. Retrieved 2021-12-19.
- ↑ 10.00 10.01 10.02 10.03 10.04 10.05 10.06 10.07 10.08 10.09 10.10 Philadelphia, The Children's Hospital of (2016-04-11). "Neck Masses". www.chop.edu. Archived from the original on 2020-04-11. Retrieved 2020-04-11.
- ↑ Schloegel, Luke J.; Gottschall, Joshua A. (2009-03-01). "Ectopic cervical thymus: Is empiric surgical excision necessary?". International Journal of Pediatric Otorhinolaryngology. 73 (3): 475–479. doi:10.1016/j.ijporl.2008.10.031. ISSN 0165-5876. PMID 19117616.
- ↑ Marx, A.; Rüdiger, T.; Rößner, E.; Tzankov, A.; de Montpréville, V. T.; Rieker, R. R.; Ströbel, P.; Weis, C.‑A. (2018-09-01). "Ektopien des Thymus und ektope Thymustumoren". Der Pathologe (in Deutsch). 39 (5): 390–397. doi:10.1007/s00292-018-0485-z. ISSN 1432-1963. PMID 30159601. S2CID 52123197.
| Classification |
|---|