CDKL5 deficiency disorder
| CDKL5 deficiency disorder | |
|---|---|
| Other names: CDKL5-related epileptic encephalopathy[1] | |
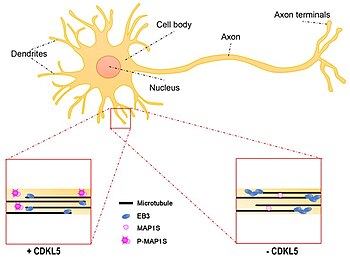 | |
| Effect of CDKL5 deficiency on dendritic microtubule dynamics | |
| Symptoms | Refractory epilepsy, Hypotonia, developmental, intellectual, and motor disabilities with little or no speech, and cortical visual impairment |
| Causes | Pathogenic variants in the gene CDKL5 |
| Diagnostic method | Genetic testing |
| Treatment | Antiseizure medications (ASMs) |
| Frequency | 1 in 42,000 live births |
CDKL5 deficiency disorder (CDD) is a rare genetic disorder caused by pathogenic variants in the gene CDKL5.
Signs and symptoms
The symptoms of CDD include early infantile onset refractory epilepsy; hypotonia; developmental, intellectual, and motor disabilities, with little or no speech; and cortical visual impairment.[2] Patients usually present first with seizures within the first months of life, followed by infantile spasms which progress to epileptic seizures that are largely refractory to treatment.[3][4] Development of gross motor skills, such as sitting, standing, and walking, is severely delayed, along with restricted fine motor skills.[1] About one-third of affected individuals can ambulate with assistance,[3] but most CDD patients rely on wheelchairs. Additional features include repetitive hand movements (stereotypies), such as clapping, hand licking, and hand sucking; tooth grinding (bruxism); disrupted sleep; feeding difficulties; gastrointestinal problems including constipation and gastroesophageal reflux. Some patients show irregular breathing.[1]
Cause
CDD is caused by pathogenic variants in the gene CDKL5. This gene provides instructions for making a protein (cyclin-dependent kinase-like 5) that is essential for normal brain development and function.[1] The CDKL5 protein is widely expressed in the brain, predominantly in nerve cells (neurons), with roles in cell proliferation, neuronal migration, axonal outgrowth, dendritic morphogenesis, and synapse development.[2] Inheritance Pattern: the CDKL5 gene is located on the X chromosome but nearly all known pathogenic mutations are de novo, rather than being inherited from an affected mother or father; the profound neurodevelopmental disabilities of CDD patients makes it extremely unlikely they would have children. There is one reported case of an inherited CDKL5 mutation; a mother carried a CDKL5 mutation on one X chromosome, but was high functioning and showed only mild cognitive impairment. The mother's mutant CDKL5 allele was skewed in its X-inactivation, being expressed in only 20% of circulating lymphoblasts. However, her daughter, who was diagnosed with CDD, expressed the mutant in 50% of her circulating lymphoblasts.[5] Females: a mutation in one of the two copies of the CDKL5 gene in each cell causes the disorder. Males: a mutation in the only copy of the gene causes the disorder.[6]
Diagnosis

For the clinical diagnosis of CDKL5 Deficiency Disorder, minimal diagnostic criteria have been established, including motor and cognitive delays, epilepsy with onset within the first year of life, and the presence of a pathogenic or likely-pathogenic mutation of the CDKL5 gene.[7]
While initial diagnosis is based mostly on clinical suspicion, definitive diagnosis requires confirmation by genetic testing. The first presentation of epileptic seizures within the first few months of life would suggest a possible diagnosis of CDD. Initial clinical testing for differential diagnosis may include MRI and CSF testing for structural or infectious etiologies; however, CDKL5 is now widely included in DNA sequence-based molecular diagnostic gene panels or infantile epilepsy for more rapid and precise diagnosis. Note: many adolescents and young adults may have CDD but were never tested since such tests were not available when they were infants. Therefore, epilepsy panels for CDD and other genes should be considered in such individuals.[8]
A diagnostic ICD-10 code has been assigned to CDKL5 deficiency disorder: G40.42 (since 2020).[9]
Treatment
Antiseizure medications (ASMs) are used to manage seizures; however, in most cases, control is partial or transient.[10] Commonly used ASMs include valproic acid, clobazam, vigabatrin, felbamate, steroids, and lamotrigine for seizures,[11] although comprehensive data are limited for the efficacy and safety of ASMs in CDD; medications for infantile spasms include ACTH, prednisolone, and vigabatrin for infantile spasms. Clinical trials support the efficacy some new ASMs.[12] Currently, there are no specifically approved therapeutics for the symptoms of CDD, although clinical trials for the treatment of CDD symptoms are currently underway, as both phase 2 and phase 3 studies. Medications to control GI and sleep disturbances are often prescribed. Therapies, including physical, occupational, and vision therapy, are recommended. Specialized diets, such as the ketogenic diet, have been reported to help manage seizures, though the effect is often partial and transitory.[13]
Prognosis
The long-term prognosis for patients with CDD is not fully known, as the disorder was identified approximately ten years ago.[14] Clinical research on the natural history of CDD is required but some CDD patients are over 60 years of age. The average life expectancy for CDD patients remains unknown.[15]
Epidemiology
The incidence rate of CDD is ~1 in 42,000 live births[16][17] This is based on both the calculated incidence rate for CDKL5 pathogenic mutations in a study population,[18] as well as comparison studies in genetic testing cohorts, in which the frequency of CDKL5 mutations is compared to that of genes whose associated disorders have more robust incidence estimates, such as SCN1A for Dravet syndrome.[19][20]
History
CDD is a rare condition although >1,000 cases have been reported worldwide; 80-90% of the cases are female[1] While originally classified as an atypical variant of Rett syndrome, CDKL5 Deficiency Disorder (CDD) is an independent disorder and results from a pathogenic variant in a different gene (CDKL5 in CDD; MECP2 in Rett). The FDA accepted the indication and approved the first pivotal trials specifically for CDD[21] and in 2019, a diagnostic ICD-10 code was issued for CDD by the World Health Organization: G40.42.[22]
Research
The goal of understanding the genetics and molecular biology of CDD is to establish effective therapies for CDD, targeting the underlying biologic pathways. Novel therapeutics may include small molecules or genetic or genomic therapies. Several efforts are underway to develop small molecule therapeutics to better control seizures, as well as provide management of other non-seizure symptoms, in CDD patients. These efforts include phase 2 and phase 3 trials already underway or completed, and others in earlier stages of development. If successful, these clinical studies may result in better symptomatic treatments that can provide significant benefit to patients and families in the short term.[23] In the long term, several independent efforts are advancing truly disease-modifying therapeutics, which are directed at the causative CDKL5 mutation itself. These disease-modifying therapies are hoped to provide broader and more durable therapeutic benefit, and even eventual cures. These include publicly announced clinical and pre-clinical programs in AAV-based gene replacement; genome targeting approaches such as base editing; and inactive X chromosome reactivation.[24]
- Clinical trials
- Small molecule therapeutic development
- Phase 3 clinical trial in CDD with ganaxolone (Marinus)[25]
- On June 29, 2017, Marinus Pharmaceuticals announced that the US Food and Drug Administration had granted Orphan Drug Designation to their small molecule, ganaxolone, for the treatment of CDKL5 Deficiency Disorder.[26]
- On November 13, 2019, ganaxolone was also awarded Orphan Designation by the European Commission for treatment of CDKL5 Deficiency Disorder[27]
- Phase 2 clinical trial in CDD with soticlestat (Ovid), a novel medication that modulates an enzyme which is thought to impact the N-methyl-D-aspartate receptor system[28]
- open-label phase 2 clinical trial in CDD with cannabidiol (Epidiolex®)[29]
- New Phase 2 clinical trial in CDD with fenfluramine[21]
- Gene therapy
- Amicus announced a collaboration around a new AAV (gene therapy)-based technology to complement their enzyme-replacement therapy in development for CDD[21]
- Several public presentations have been made on pre-clinical AAV-based gene therapy programs from Ultragenyx and UPenn Gene Therapy Program (see abstracts of American Society of Gene and Cell Therapy, May 2020:[30]
- Small molecule therapeutic development
- Molecular biology of CDD is revealing further opportunities in precision therapy[2]
- Nonsense mutations in the CDKL5 gene could be suppressed by compounds such as ataluren;[31] (PTC Therapeutics), or similar next-generation translation stop readthrough compounds.
- Genome editing: Pre-clinical programs in Prime-Editing-directed correction of mutations in the CDKL5 gene have been reported (CDKL5 Forum 2020:[32]
- X reactivation: in female patients heterozygous for the CDKL5 mutation, each cell expressing the mutant protein also carries a fully functional, but silent, CDKL5 gene copy on the inactivated X chromosome. One strategy for treatment of girls with CDD is thus to re-activate the silent, inactivated CDKL5 gene on the inactivated X chromosome. This approach is currently in pre-clinical development.
Studies of molecular pathway abnormalities in CDD rodent models may suggest additional possible therapies, such as protein substitution.[33] Within the research community, the Loulou Foundation's annual meetings with scientists and drug developers have become the largest conference focusing on CDD biology and therapeutic development. Contribution to research and therapeutic development by companies Takeda and Ovid Therapeutics[21] is also vital, which was recognized by the Loulou Foundation providing Company Making a Difference Award for initiation of the Phase 2 ARCADE trial with OV935/TAK-935 to these companies.[34]
References
- ↑ 1.0 1.1 1.2 1.3 1.4 "CDKL5 deficiency disorder". MedlinePlus. Archived from the original on 27 September 2020. Retrieved 21 June 2021.
- ↑ 2.0 2.1 2.2 Olson, Heather E.; Demarest, Scott T.; Pestana-Knight, Elia M.; Swanson, Lindsay C.; Iqbal, Sumaiya; Lal, Dennis; Leonard, Helen; Cross, J. Helen; Devinsky, Orrin; Benke, Tim A. (2019). "Cyclin-Dependent Kinase-Like 5 Deficiency Disorder: Clinical Review". Pediatric Neurology. 97: 18–25. doi:10.1016/j.pediatrneurol.2019.02.015. PMC 7120929. PMID 30928302.
- ↑ 3.0 3.1 "MalaCards integrated aliases for Cdkl5 Deficiency Disorder". MalaCards. Archived from the original on 24 June 2021. Retrieved 21 June 2021.
- ↑ Bahi-Buisson, Nadia (2008). "The three stages of epilepsy in patients with CDKL5 mutations". Epilepsia. Hoboken, NJ: Wiley Online Library. 49 (6): 1027–1037. doi:10.1111/j.1528-1167.2007.01520.x. PMID 18266744. S2CID 25784794. Archived from the original on 9 November 2020. Retrieved 21 June 2021.
- ↑ Allou, L. (2016). "Rett‐like phenotypes: expanding the genetic heterogeneity to the KCNA2 gene and first familial case of CDKL5‐related disease". Clinical Genetics. Hoboken, NJ: Wiley Online Library. 91 (3): 431–440. doi:10.1111/cge.12784. PMID 27062609. S2CID 22625690. Archived from the original on 24 June 2021. Retrieved 21 June 2021.
- ↑ "CDKL5 deficiency disorder". Medlineplus. Archived from the original on 7 June 2021. Retrieved 22 June 2021.
- ↑ Olson, Heather E. (2019). Cyclin-dependent kinase-like 5 (CDKL5) deficiency disorder: clinical review (PDF). CDKL5 Alliance Francophone. Archived (PDF) from the original on 24 June 2021. Retrieved 21 June 2021.
- ↑ "LAE Classification & Definition of Epilepsy Syndromes in the Neonate and Infant: Position Statement by the ILAE Task Force on Nosology and Definitions" (PDF). Ilae. Archived (PDF) from the original on 24 June 2021. Retrieved 22 June 2021.
- ↑ "ICD-10 Coordination and Maintenance Committee Meeting" (PDF). Cdc. Archived (PDF) from the original on 24 June 2021. Retrieved 22 June 2021.
- ↑ "Initial treatment of epilepsy". Uptodate. Archived from the original on 24 June 2021. Retrieved 22 June 2021.
- ↑ Morelli, Jim. "Seizure medications". RxList. Archived from the original on 24 June 2021. Retrieved 22 June 2021.
- ↑ Glauser, Tracy. "Infantile Spasm (West Syndrome) Treatment & Management". Archived from the original on 24 June 2021. Retrieved 22 June 2021.
- ↑ d'Andrea Meira, I.; Romão, T. T.; Pires Do Prado, H. J.; Krüger, L. T.; Pires, M. E.; Da Conceição, P. O. (2019). "Ketogenic Diet and Epilepsy: What We Know So Far". Frontiers in Neuroscience. 13: 5. doi:10.3389/fnins.2019.00005. PMC 6361831. PMID 30760973.
- ↑ Fehr, Stephanie (2013). The CDKL5 disorder is an independent clinical entityassociated with early-onset encephalopathy (PDF). European Journal of Human Genetics. pp. 21, 266–273. Archived (PDF) from the original on 24 February 2022. Retrieved 21 June 2021.
- ↑ "CDKL5-deficiency disorder". Orpha.net. Archived from the original on 24 June 2021. Retrieved 22 June 2021.
- ↑ "Abcam and Loulou Foundation form CDKL5 deficiency disorder partnership". PharmaTimes. 22 January 2019. Archived from the original on 24 June 2021. Retrieved 21 June 2021.
- ↑ Brackley, Paul (26 January 2019). "Abcam collaborates with Loulou Foundation to accelerate research into CDKL5 deficiency disorder". Cambridge Independent. Archived from the original on 24 June 2021. Retrieved 21 June 2021.
- ↑ Symonds, Joseph D. (2019). Incidence and phenotypes of childhood-onset genetic epilepsies: a prospective population-based national cohort. Brain: A Journal of Neurology. Vol. 142. Watermark Silverchair. pp. 2303–2318. doi:10.1093/brain/awz195. PMC 6658850. PMID 31302675.
- ↑ Lindy, Amanda S. (14 April 2018). "Diagnostic outcomes for genetic testing of 70 genes in 8565 patients with epilepsy and neurodevelopmental disorders". Epilepsia. Hoboken, NJ: Wiley Online Library. 59 (5): 1062–1071. doi:10.1111/epi.14074. PMID 29655203. S2CID 4869906.
- ↑ Kathur, Kavitha (2018). Diagnostic yield of targeted massively parallel sequencing in children with epileptic encephalopathy. p. Seizure 2018, 59:132–140. Retrieved 21 June 2021.
- ↑ 21.0 21.1 21.2 21.3 "Main lessons from the 2018 CDKL5 Forum". Dracaena Consulting. 25 October 2018. Archived from the original on 24 June 2021. Retrieved 21 June 2021.
- ↑ Mingorance, Ana (30 January 2020). "CDKL5 Deficiency Disorder Added to WHO International Classification of Diseases". Neurologylive. Archived from the original on 24 June 2021. Retrieved 22 June 2021.
- ↑ "Marinus Pharmaceuticals Receives Positive Response from FDA on Sufficiency of One Phase 3 Clinical Trial for Filing of New Drug Application (NDA) for the Use of Ganaxolone in CDKL5 Deficiency Disorder (CDD)". Biospace. Archived from the original on 24 June 2021. Retrieved 22 June 2021.
- ↑ Green, Michael. "Discovery of Therapeutically Targetable Pathways in Cancer and Other Diseases". Umassmed. Archived from the original on 24 June 2021. Retrieved 22 June 2021.
- ↑ "Study of Adjunctive Ganaxolone Treatment in Children and Young Adults With CDKL5 Deficiency Disorder". ClinicalTrials.gov. Archived from the original on 24 June 2021. Retrieved 21 June 2021.
- ↑ "Orphan Drug Designations and Approvals". U.S. Food & Drug Administration. Archived from the original on 24 June 2021. Retrieved 21 June 2021.
- ↑ "EU/3/19/2224". European Medicines Agency. 13 February 2020. Archived from the original on 22 June 2021. Retrieved 21 June 2021.
- ↑ "A Multicenter, Open-label, Pilot Study of Soticlestat (TAK-935/OV935) in Participants With 15Q Duplication Syndrome (Dup 15q) or Cyclin-Dependent Kinase-Like 5 (CDKL5) Deficiency Disorder". ClinicalTrials.gov. Archived from the original on 24 June 2021. Retrieved 21 June 2021.
- ↑ Devinsky, Orrin (2018). Open-label use of Highly* purified CBD (Epidiolex®) in patients withCDKL5 deficiency disorder and Aicardi, Dup15q, and Doose syndromes (PDF). Magyar Orvosi Kannabisz Egyesület. p. Epilepsy & Behavior 86:131. Archived (PDF) from the original on 24 June 2021. Retrieved 21 June 2021.
- ↑ "Gene Therapy for the Special Senses". American Society of Gene + Cell Therapy. Archived from the original on 19 October 2023. Retrieved 21 June 2021.
- ↑ "Ataluren for Nonsense Mutation in CDKL5 and Dravet Syndrome". ClinicalTrials.gov. Archived from the original on 24 June 2021. Retrieved 21 June 2021.
- ↑ "Main lessons from the 2020 CDKL5 Forum". Dracaena Consulting. 20 October 2020. Archived from the original on 24 June 2021. Retrieved 21 June 2021.
- ↑ "CDKL5 protein substitution therapy rescuesneurological phenotypes of a mouse model of CDKL5 disorder".
{{cite journal}}: Cite journal requires|journal=(help) - ↑ "Ovid Therapeutics Receives "Company Making a Difference Award" from CDKL5 Deficiency Disorder Community". Ovid Therapeutics. Archived from the original on 24 June 2021. Retrieved 21 June 2021.
External links
| Classification |
|---|