Birth control patch
| Birth control patch | |
|---|---|
 Ortho Evra brand of birth control patch | |
| Background | |
| Type | Hormonal (estrogen + progestin) |
| First use | 2002[1] |
| Failure rates (first year) | |
| Perfect use | 0.3%[2] |
| Typical use | 7%[2] |
| Usage | |
| User reminders | Applied weekly[3] |
| Advantages and disadvantages | |
| STI protection | No[3] |
| Weight | No effect[4] |
| Period advantages | Lighter, though spotting may occur[2] |
| Risks | Slight increase in DVTs (1 in 2,000)[2][5] |
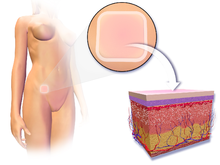
Birth control patch, also known as contraceptive patch or the patch, is a patch applied to the skin to prevent pregnancy.[6] Effectiveness is similar to combined birth control pills.[4] Other benefits include the ability to determine when periods occur, improved acne, and less PMS.[4][2] They are typically used for a week each for three weeks followed by a week off; though may be used for longer durations.[7][4] After stopping fertility returns to normal in about 4 months.[2]
Common side effects include headache, breast tenderness, and nausea.[6] Use is not recommended in those with liver problems, migraines with aura, or at risk of blood clots.[6] Those at risk of blood clots include those over 35 years old who smoke.[3] It works less well in those who weigh more than 90 kilograms (200 lb) or have a BMI ≥ 30 kg/m2.[6][3] They work by releases versions of the hormones estrogen and progestogen, which prevents ovulation and altering cervical mucus.[6]
The birth control patch was approved for medical use in the United States in 2001 and Europe in 2002.[8][6] Types include norelgestromin/ethinyl estradiol (Ortho Evra, Evra, Xulane)[4][6] and levonorgestrel/ethinyl estradiol (Twirla).[4][3] A generic version became available in 2014.[4] They are used by about 0.4% of women not wanting to become pregnant in the United States.[2] In the United States it costs about 35 USD per month as of 2024.[9]
Medical uses
Because the patch works similar to that of birth control pills, many of the benefits are the same. For example, the patch may make periods lighter and more regular. It may also help to clear acne, decrease cramps, and reduce PMS symptoms. Additionally, the patch is associated with an increased protection against iron deficiency anemia, ovarian cysts, pelvic inflammatory disease, and endometrial and ovarian cancer.
The patch is a simple and convenient form of birth control that requires weekly attention. When a woman stops using the patch, the ability to become pregnant returns quickly.[10]
Method of use
The patch is first applied onto the upper outer arm, buttocks, abdomen or thigh on either the first day of the menstrual cycle (day 1) or on the first Sunday following that day, whichever is preferred. The day of application is known from that point as patch change day. Seven days later, when patch change day comes again, the user removes the patch and applies another to one of the approved locations on the body. This process is repeated again on the next patch change day. On the following patch change day, the patch is removed and not replaced. The user waits seven days without a patch in place, and on the next patch change day they apply a new patch. Extended use regimens, where patches are used for several weeks before a patch-free week, have been studied.[11]
The patch should be applied to skin that is clean, dry, and intact. This means if skin is red, irritated, or cut, the patch should not be placed in that area. Additionally, avoid using lotions, powder, or makeup around the area where the patch is or will be placed.[12]
Backup
- If someone chooses to begin with their patch change day as day one of their menstrual cycle, the patch is able to take effect in time to prevent ovulation (see Mechanism of Action below) and no form of backup contraception is needed at all.
- In the case that one wishes to begin using the contraceptive patch following a first trimester abortion or miscarriage, patch application can be done immediately afterwards. This can be considered the same as a day one start above, and no backup contraception is required.
- If a user chooses to begin with their patch change day as the first Sunday following day 1, it is necessary to use a backup form of contraception such as spermicide or condoms for the first week of patch wear.
- If the user is late placing her patch in the first week, or more than two days late placing the patch in the second and third weeks, they should apply the patch immediately, and then use a backup form of barrier protection for a week.[12]
- If someone chooses to begin with their patch change day as day one of their menstrual cycle, the patch is able to take effect in time to prevent ovulation (see Mechanism of Action below) and no form of backup contraception is needed at all.
Side effects
In three large clinical trials involving a total of 3,330 women using the Ortho Evra / Evra patch for up to one year, 12% of users discontinued the patch because of adverse events. The most frequent adverse events leading to patch discontinuation were: nausea and/or vomiting (2.4%), application site reaction (1.9%), breast discomfort, engorgement or pain (1.9%), headache (1.1%), and emotional lability (1.0%).[13]
The most frequent adverse events reported while using the Ortho Evra / Evra patch were: breast discomfort, engorgement or pain (22%), headache (21%), application site reaction (17%), nausea (17%), upper respiratory tract infection (10%), menstrual cramps (10%), and abdominal pain (9%).[13]
Breakthrough bleeding and/or spotting while using the Ortho Evra / Evra patch was reported by: 18% in cycle 1, 12% in cycle 3, 8% in cycle 6 and cycle 13. Breakthrough bleeding (requiring more than one pad or tampon per day) was reported by: 4% in cycle 1, 3% in cycle 3 and cycle 6, and 1% in cycle 13.[14]
Overall, side effects that tend to go away after two or three months include bleeding between periods, breast tenderness, and nausea and vomiting. Symptoms that may last longer include skin irritation around the area where the patch is placed and a change in the woman's sexual desires.
Additional side effect information is provided in the Ortho Evra label information and the Evra Summary of Product Characteristics (SPC) and PIL.[7][15][16]
Interactions
Effectiveness of the patch or any other hormonal contraceptive may be reduced if taken alongside certain antibiotics, antifungals, anticonvulsants, or other drugs that increase metabolism of contraceptive steroids.
Despite the interactions with certain antibiotics, a study showed that tetracycline 500 mg by mouth for three days prior to and seven days during use of Ortho Evra did not reduce effectiveness. This is a factor in the common decision to administer tetracycline-derived antibiotics following an abortion (preventatively) when hormone contraceptives are to be used afterwards.
Drugs containing St. John's wort are also known to decrease the effectiveness of hormonal contraceptives.
It has also been found that the patch is less effective in women who weigh more than 198 pounds (90 kg).
The contraceptive patch and other combination hormonal contraceptives are often not recommended in women older than 35 years who smoke cigarettes.[7]
The patch is also often not recommended in women with a BMI ≥ 30 kg/m2.[7]
Blood clots
All combined hormonal birth control products have a small increased risk of serious or fatal thromboembolic events. There is ongoing research into the thromboembolic risks of Ortho Evra as compared to combined birth control pills. A study found that users of the birth control patch may have a twofold increased risk for non-fatal venous thromboembolic events compared with women who took a norgestimate-containing birth control with 35 µg of estrogen.[17][18] However, a different study found the risk of nonfatal blood clots for the patch is similar to the risk with birth control pills containing 35 µg of ethinylestradiol and norgestimate.[19] The contradiction in findings between the two studies is not easily resolved, as the confidence intervals for the studies are overlapping.
In studies with oral contraceptives, the risk for cardiovascular disease (such as thromboembolism) is significantly increased in women over the age of 35 years who also smoke tobacco.[20] Hence, Ortho Evra's package insert states: "Women who use hormonal contraceptives, including Ortho Evra, should be strongly advised not to smoke."
According to the manufacturer, the patches introduce a 60% higher level of estrogen into the bloodstream as compared to birth control pills; however, the significance of this difference is unknown.
On November 10, 2005, Ortho McNeil, in conjunction with the FDA, revised the label for Ortho Evra, including a new bolded warning about higher exposure to estrogen for women using the weekly patch compared to taking a daily birth control pill containing 35 µg of estrogen, noting that higher levels of estrogen may put some women at increased risk for getting blood clots. The label was again revised in September 2006, and on January 18, 2008, the FDA again updated the label to reflect study results: "The FDA believes that Ortho Evra is a safe and effective method of contraception when used according to the labeling, which recommends that women with concerns or risk factors for serious blood clots talk with their health care provider about using Ortho Evra versus other contraceptive options."[21]
Mechanism of action
Like all combined hormonal contraceptives, Ortho Evra / Evra works primarily by preventing ovulation. A secondary mechanism of action is inhibition of sperm penetration by changes in the cervical mucus. Hormonal contraceptives also have effects on the endometrium that theoretically could affect implantation; however, no scientific evidence indicates that prevention of implantation actually results from their use.[22]
The 20 cm2 Ortho Evra contraceptive patch contains 750 µg ethinylestradiol (an estrogen) and 6000 µg norelgestromin (a progestin).[7] The 20 cm2 Evra contraceptive patch contains 600 µg ethinylestradiol and 6000 µg norelgestromin.[15] The Ortho Evra contraceptive patch and the Evra contraceptive patch are both intended to gradually release into the systemic circulation approximately 20 µg/day of ethinylestradiol and 150 µg/day of norelgestromin.[7][15]
Lawsuits
The parents of a 14-year-old girl from Wisconsin have filed a lawsuit against Johnson & Johnson because they claim that she died from a blood clot that arose from her use of the patch.[23]
References
- ↑ "Ortho Evra patch discontinued — What next? | 2015-02-02 | AHC Media:…". Relias Media. Archived from the original on 2022-01-23. Retrieved 18 February 2024.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 Cason, Patty; Cwiak, Carrie; Kowal, Deborah; Edelman, Alison (26 September 2023). "5". Contraceptive Technology. Jones & Bartlett Learning. pp. 125–163. ISBN 978-1-284-25503-4. Retrieved 18 February 2024.
- ↑ 3.0 3.1 3.2 3.3 3.4 "DailyMed - TWIRLA- levonorgestrel/ethinyl estradiol patch". dailymed.nlm.nih.gov. Archived from the original on 25 October 2022. Retrieved 18 February 2024.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 Cason, Patty; Cwiak, Carrie; Kowal, Deborah; Edelman, Alison (26 September 2023). "12". Contraceptive Technology (22 ed.). Jones & Bartlett Learning. pp. 359–405. ISBN 978-1-284-25503-4. Retrieved 18 February 2024.
- ↑ Lopez, LM; Grimes, DA; Gallo, MF; Stockton, LL; Schulz, KF (30 April 2013). "Skin patch and vaginal ring versus combined oral contraceptives for contraception". The Cochrane database of systematic reviews. 2013 (4): CD003552. doi:10.1002/14651858.CD003552.pub4. PMID 23633314.
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 6.6 "Evra EPAR". European Medicines Agency. 17 September 2018. Archived from the original on 12 November 2020. Retrieved 18 February 2020.
- ↑ 7.0 7.1 7.2 7.3 7.4 7.5 "Xulane- norelgestromin and ethinyl estradiol patch". DailyMed. 19 April 2017. Archived from the original on 6 July 2020. Retrieved 17 February 2020.
- ↑ "Drug Approval Package: Ortho EVRA (Norelgestromin/Ethinyl Estradiol Transdermal System NDA #21-180". U.S. Food and Drug Administration (FDA). Archived from the original on 5 July 2020. Retrieved 4 July 2020.
- ↑ "Xulanegeneric Ortho Evra". GoodRx. Archived from the original on 9 May 2023. Retrieved 18 February 2024.
- ↑ "Birth Control Patch (Ortho Evra)". Planned Parenthood. 3 February 2011. Archived from the original on 11 April 2014. Retrieved 29 January 2023.
- ↑ Stewart FH, Kaunitz AM, Laguardia KD, Karvois DL, Fisher AC, Friedman AJ (June 2005). "Extended use of transdermal norelgestromin/ethinyl estradiol: a randomized trial". Obstetrics and Gynecology. 105 (6): 1389–1396. doi:10.1097/01.AOG.0000160430.61799.f6. PMID 15932834. S2CID 8831803.
- ↑ 12.0 12.1 "Ortho Evra (Contraceptive Patch)". Mayo Clinic. 2010. Archived from the original on 15 October 2012. Retrieved 3 February 2011.
- ↑ 13.0 13.1 Sibai BM, Odlind V, Meador ML, Shangold GA, Fisher AC, Creasy GW (February 2002). "A comparative and pooled analysis of the safety and tolerability of the contraceptive patch (Ortho Evra/Evra)". Fertility and Sterility. 77 (2 Suppl 2): S19–S26. doi:10.1016/S0015-0282(01)03264-2. PMID 11849632.
- ↑ Zieman M, Guillebaud J, Weisberg E, Shangold GA, Fisher AC, Creasy GW (February 2002). "Contraceptive efficacy and cycle control with the Ortho Evra/Evra transdermal system: the analysis of pooled data". Fertility and Sterility. 77 (2 Suppl 2): S13–S18. doi:10.1016/S0015-0282(01)03275-7. PMID 11849631.
- ↑ 15.0 15.1 15.2 "Evra transdermal patch - Summary of Product Characteristics (SmPC)". (emc). 29 November 2018. Archived from the original on 7 November 2017. Retrieved 17 February 2020.
- ↑ Janssen-Cilag (January 26, 2007). "Evra Patient Information Leaflet (PIL)". Archived from the original on September 28, 2007. Retrieved 2007-07-20.
- ↑ Medpage Today. Evidence on Ortho Evra Patch Thrombosis Risk Is Contradictory Archived 2006-03-01 at the Wayback Machine. Published February 17, 2006.
- ↑ Cole JA, Norman H, Doherty M, Walker AM (February 2007). "Venous thromboembolism, myocardial infarction, and stroke among transdermal contraceptive system users". Obstetrics and Gynecology. 109 (2 Pt 1): 339–346. doi:10.1097/01.AOG.0000250968.82370.04. PMID 17267834. S2CID 1572286.
- ↑ Jick S, Kaye JA, Li L, Jick H (July 2007). "Further results on the risk of nonfatal venous thromboembolism in users of the contraceptive transdermal patch compared to users of oral contraceptives containing norgestimate and 35 microg of ethinyl estradiol". Contraception. 76 (1): 4–7. doi:10.1016/j.contraception.2007.03.003. PMID 17586129.
- ↑ Pitsavos C, Stefanadis C, Toutouzas P (2000). "Contraception in women at high risk or with established cardiovascular disease". Annals of the New York Academy of Sciences. 900 (1): 215–227. Bibcode:2000NYASA.900..215P. doi:10.1111/j.1749-6632.2000.tb06233.x. PMID 10818409. S2CID 45035196.
- ↑ FDA Approves Update to Label on Birth Control Patch. FDA. January 18, 2008 Archived May 12, 2009, at the Wayback Machine
- ↑ Rivera R, Yacobson I, Grimes D (November 1999). "The mechanism of action of hormonal contraceptives and intrauterine contraceptive devices". American Journal of Obstetrics and Gynecology. 181 (5 Pt 1): 1263–1269. doi:10.1016/S0002-9378(99)70120-1. PMID 10561657.
- ↑ Schott K, Foley RJ (18 November 2005). "Family sues birth control maker over death of daughter, 14". The La Crosse Tribune. The Associated Press. Archived from the original on 26 October 2008.
External links
- "Ethinyl Estradiol mixture with norelgestromin". Drug Information Portal. U.S. National Library of Medicine. Archived from the original on 2021-02-09. Retrieved 2023-01-29.
- Feminist Women's Health Center
- Planned Parenthood: The Patch Archived 2023-02-05 at the Wayback Machine





