Factor H
| CFH | |||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
 | |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| Identifiers | |||||||||||||||||||||||||||||||||||||||||||||||||||
| Aliases | CFH, AHUS1, AMBP1, ARMD4, ARMS1, CFHL3, FH, FHL1, HF, HF1, HF2, HUS, complement factor H | ||||||||||||||||||||||||||||||||||||||||||||||||||
| External IDs | OMIM: 134370 MGI: 88385 HomoloGene: 20086 GeneCards: CFH | ||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| Wikidata | |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
Factor H (FH) is a member of the regulators of complement activation family and is a complement control protein. It is a large (155 kilodaltons), soluble glycoprotein that circulates in human plasma (at typical concentrations of 200–300 micrograms per milliliter[5][6][7]). Its principal function is to regulate the alternative pathway of the complement system, ensuring that the complement system is directed towards pathogens or other dangerous material and does not damage host tissue. Factor H regulates complement activation on self cells and surfaces by possessing both cofactor activity for Factor I–mediated C3b cleavage, and decay accelerating activity against the alternative pathway C3-convertase, C3bBb. Factor H exerts its protective action on self cells and self surfaces but not on the surfaces of bacteria or viruses. There are however, important exceptions, such as for example the bacterial pathogen, Neisseria meningitidis (also called the meningococcus). This human pathogen has evolved mechanisms to recruit human FH and down-regulate the alternative pathway.[8] Binding of FH permits the bacteria to proliferate in the bloodstream and cause disease.[9]
The ability of Factor H to exert its protective action on self cells and self surfaces is thought to be the result of Factor H having the ability to adopt conformations with lower or higher activities as a cofactor for C3 cleavage or decay accelerating activity.[10] The lower activity conformation is the predominant form in solution and is sufficient to control fluid phase amplification. The more active conformation is thought to be induced when Factor H binds to glycosaminoglycans (GAGs) and or sialic acids that are generally present on host cells but not, normally, on pathogen surfaces ensuring that self surfaces are protected whilst complement fixation proceeds unabated on foreign surfaces.[11][12]
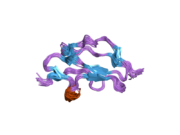
Structure
The molecule is made up of 20 complement control protein (CCP) modules (also referred to as Short Consensus Repeats or sushi domains) connected to one another by short linkers (of between three and eight amino acid residues) and arranged in an extended head to tail fashion. Each of the CCP modules consists of around 60 amino acids with four cysteine residues disulfide bonded in a 1–3 2–4 arrangement, and a hydrophobic core built around an almost invariant tryptophan residue. The CCP modules are numbered from 1–20 (from the N-terminus of the protein); CCPs 1–4 and CCPs 19–20 engage with C3b while CCPs 7 and CCPs 19–20 bind to GAGs and sialic acid.[13] To date atomic structures have been determined for CCPs 1–3,[14] CCP 5,[15] CCP 7,[16] CCPs 10–11 and CCPs 11–12,[17] CCPs 12–13,[18] CCP 15, CCP 16,[19] CCPs 15–16,[20] CCPs 18–20,[21] and CCPs 19–20.[22][23] The atomic structure for CCPs 6–8 bound to the GAG mimic sucrose octasulfate,[24] CCPs 1–4 in complex with C3b[25] and CCPs 19–20 in complex with C3d (that corresponds to the thioester domain of C3b)[26][27] have also been determined. Although an atomic resolution structure for intact factor H has not yet been determined, low resolution techniques indicate that it may be bent back in solution.[28] Information available to date indicates that CCP modules 1–4 is responsible for the cofactor and decay acceleration activities of factor H, whereas self/non-self discrimination occurs predominantly through GAG binding to CCP modules 7 and/or GAG or sialic acid binding to 19–20.[28][29]
Clinical significance
Due to the central role that factor H plays in the regulation of complement, there are a number of clinical implications arising from aberrant factor H activity. Overactive factor H may result in reduced complement activity on pathogenic cells – increasing susceptibility to microbial infections. Underactive factor H may result in increased complement activity on healthy host cells – resulting in autoimmune diseases. It is not surprising, therefore, that rare mutations or common single nucleotide polymorphisms (SNPs) in the complement factor H gene (CFH) often result in pathologies. Moreover, the complement inhibitory activities of factor H, and other complement regulators, are often used by pathogens to increase virulence.
In 2005, several independent research groups identified an SNP in CFH, which results in the protein change p.Y402H, as a risk factor for AMD present in around a third of Europeans.[30] Although its allele frequency varies considerably between different populations, Y402H has been consistently associated with AMD onset and progression.[30] Homozygous individuals have an approximately seven-fold greater odds of association with AMD while heterozygotes have a two-to-three-fold greater odds of association with the disease.[30] This SNP, located in CCP module 7 of factor H, has been shown to affect the ability of factor H protein to localise to sites of inflammation in retinal tissues (e.g. by polyanions and pentraxins) and to regulate the activation of complement and immune cells.[30] The SNP has also been shown to affect the function of factor H-like protein 1, an alternatively spliced version of factor H consisting of CCPs 1 to 7 only, which is thought to have a greater role in intraocular complement regulation.[30] However, the genetic variants in CFH with the greatest effect on an individual's risk of AMD have been shown to affect CCPs 1 to 4, which are involved in dampening the effects of the alternative pathway of complement.[30] A rare functional coding change, p.R1210C, in CFH results in a functional deficiency in factor H and leads to a substantially higher risk of macular degeneration as well as complement-mediated renal conditions.[30][31]
Variation in other genes of the regulators of complement activation locus, such as complement factor H-related genes, as well as in other complement proteins (e.g. factor I, C2/factor B, and C3) have also been associated with greater AMD risk.[30] The current theory is that complement dysregulation is a key driver of chronic inflammation in AMD.[30]
Atypical hemolytic uremic syndrome
Hemolytic uremic syndrome (HUS) is a disease associated with microangiopathic hemolytic anemia, thrombocytopenia, and acute renal failure. It can be either acquired (e.g. following infection with shigatoxigenic Escherichia coli), or inherited (also known as atypical hemolytic uremic syndrome, aHUS). aHUS has been strongly linked to mutations in genes of the complement system, especially factor H.[30] In contrast to AMD and C3 glomerulopathy (another complement-mediated renal disorder) which are mainly associated with variation in the N-terminus (CCPs 1 to 4), predisposing mutations in factor H mainly affect the C-terminus of the protein (CCP modules 19 and 20),[30] which has been shown to be responsible for adherence to renal tissues and the regulation of complement components and their downstream effectors.[30][32][33]
Schizophrenia
Alterations in the immune response are involved in pathogenesis of many neuropsychiatric disorders including schizophrenia. Recent studies indicated alterations in the complement system, including those which may result in the overactivation of the alternative complement pathway, may predispose to schizophrenia. For example, the CFH SNP rs424535 (2783-526T>A) was positively associated with schizophrenia.[34]
Ischemic stroke
It was found that rs800292(184G >A) SNP was positively associated with stroke and rs800912 minor allele of the CFH gene might be considered as a risk factor for ischemic stroke.[34]
Recruitment by pathogens
Given the central role of factor H in protecting cells from complement, it is not surprising that several important human pathogens have evolved mechanisms for recruiting factor H. This recruitment of factor H by pathogens provides significant resistance to complement attack, and therefore increased virulence. Pathogens that have been shown to recruit factor H include: Aspergillus spp.; Borrelia burgdorferi; B. duttonii; B. recurrentis; Candida albicans;[35] Francisella tularensis; Haemophilus influenzae; Neisseria gonorrhoeae;[36] N. meningitidis; Streptococcus pneumoniae;[10] and Streptococcus pyogenes. The Gram-negative bacterium B. burgdorferi has five Factor H binding proteins: CRASP-1, CRASP-2, CRASP-3, CRASP-4 and CRASP-5.[37] Each CRASP protein also binds plasminogen.[37] It is possible that the allele frequency of CFH variants across the globe reflects selective pressure from infectious diseases.[30]
Interactions
Factor H has been shown to interact with complement component 3, amongst other complement proteins and factors, leading to regulation of the alternative pathway of complement in particular.[30][38][39]
Recombinant production
Biologically active Factor H has been produced by Ralf Reski and coworkers in the moss bioreactor,[40] in a process called molecular farming. Large quantities of biologically active human Factor H, potentially suitable for therapeutic purposes, were produced using a synthetic codon-optimised gene expressed in the yeast expression host, Pichia pastoris.[41]
Potential use as a therapeutic drug
Gemini Therapeutics Inc. is a Massachusetts based precision medicine company focused on the development of new therapies through a deeper understanding of disease. Based on the biological activity of human factor H, Gemini is developing a recombinant human factor H protein, GEM103, for the treatment of dry AMD. Gemini recently announced the completion of enrollment in a Phase 2a Trial of GEM103 in Dry Age-Related Macular Degeneration (AMD) in Patients with High-Risk Genetic Variants. Top line data are expected in 1H 2021.
References
- ^ a b c GRCh38: Ensembl release 89: ENSG00000000971 – Ensembl, May 2017
- ^ a b c GRCm38: Ensembl release 89: ENSMUSG00000026365 – Ensembl, May 2017
- ^ "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ Sofat R, Mangione PP, Gallimore JR, Hakobyan S, Hughes TR, Shah T, et al. (April 2013). "Distribution and determinants of circulating complement factor H concentration determined by a high-throughput immunonephelometric assay". Journal of Immunological Methods. 390 (1–2): 63–73. doi:10.1016/j.jim.2013.01.009. PMID 23376722.
- ^ Hakobyan S, Harris CL, Tortajada A, Goicochea de Jorge E, García-Layana A, Fernández-Robredo P, et al. (May 2008). "Measurement of factor H variants in plasma using variant-specific monoclonal antibodies: application to assessing risk of age-related macular degeneration". Investigative Ophthalmology & Visual Science. 49 (5): 1983–1990. doi:10.1167/iovs.07-1523. hdl:10261/56608. PMID 18436830.
- ^ Scholl HP, Charbel Issa P, Walier M, Janzer S, Pollok-Kopp B, Börncke F, et al. (July 2008). "Systemic complement activation in age-related macular degeneration". PLOS ONE. 3 (7): e2593. Bibcode:2008PLoSO...3.2593S. doi:10.1371/journal.pone.0002593. PMC 2440421. PMID 18596911.
- ^ Lewis LA, Carter M, Ram S (May 2012). "The relative roles of factor H binding protein, neisserial surface protein A, and lipooligosaccharide sialylation in regulation of the alternative pathway of complement on meningococci". Journal of Immunology. 188 (10): 5063–5072. doi:10.4049/jimmunol.1103748. PMC 3345070. PMID 22504643.
- ^ Vu DM, Shaughnessy J, Lewis LA, Ram S, Rice PA, Granoff DM (February 2012). Bliska JB (ed.). "Enhanced bacteremia in human factor H transgenic rats infected by Neisseria meningitidis". Infection and Immunity. 80 (2): 643–650. doi:10.1128/IAI.05604-11. PMC 3264313. PMID 22104107.
- ^ a b Herbert AP, Makou E, Chen ZA, Kerr H, Richards A, Rappsilber J, Barlow PN (November 2015). "Complement Evasion Mediated by Enhancement of Captured Factor H: Implications for Protection of Self-Surfaces from Complement". Journal of Immunology. 195 (10): 4986–4998. doi:10.4049/jimmunol.1501388. PMC 4635569. PMID 26459349.
- ^ Pangburn MK (August 2000). "Host recognition and target differentiation by factor H, a regulator of the alternative pathway of complement". Immunopharmacology. 49 (1–2): 149–157. doi:10.1016/S0162-3109(00)80300-8. PMID 10904114.
- ^ Rodríguez de Córdoba S, Esparza-Gordillo J, Goicoechea de Jorge E, Lopez-Trascasa M, Sánchez-Corral P (June 2004). "The human complement factor H: functional roles, genetic variations and disease associations". Molecular Immunology. 41 (4): 355–367. doi:10.1016/j.molimm.2004.02.005. PMID 15163532.
- ^ Schmidt CQ, Herbert AP, Kavanagh D, Gandy C, Fenton CJ, Blaum BS, et al. (August 2008). "A new map of glycosaminoglycan and C3b binding sites on factor H". Journal of Immunology. 181 (4): 2610–2619. doi:10.4049/jimmunol.181.4.2610. PMID 18684951.
- ^ Hocking HG, Herbert AP, Kavanagh D, Soares DC, Ferreira VP, Pangburn MK, et al. (April 2008). "Structure of the N-terminal region of complement factor H and conformational implications of disease-linked sequence variations". The Journal of Biological Chemistry. 283 (14): 9475–9487. doi:10.1074/jbc.M709587200. PMC 2276370. PMID 18252712.
- ^ Barlow PN, Norman DG, Steinkasserer A, Horne TJ, Pearce J, Driscoll PC, et al. (April 1992). "Solution structure of the fifth repeat of factor H: a second example of the complement control protein module". Biochemistry. 31 (14): 3626–3634. doi:10.1021/bi00129a011. PMID 1533152.
- ^ Herbert AP, Deakin JA, Schmidt CQ, Blaum BS, Egan C, Ferreira VP, et al. (June 2007). "Structure shows that a glycosaminoglycan and protein recognition site in factor H is perturbed by age-related macular degeneration-linked single nucleotide polymorphism". The Journal of Biological Chemistry. 282 (26): 18960–18968. doi:10.1074/jbc.M609636200. PMID 17360715.
- ^ Makou E, Mertens HD, Maciejewski M, Soares DC, Matis I, Schmidt CQ, et al. (December 2012). "Solution structure of CCP modules 10-12 illuminates functional architecture of the complement regulator, factor H". Journal of Molecular Biology. 424 (5): 295–312. doi:10.1016/j.jmb.2012.09.013. PMC 4068365. PMID 23017427.
- ^ Schmidt CQ, Herbert AP, Mertens HD, Guariento M, Soares DC, Uhrin D, et al. (January 2010). "The central portion of factor H (modules 10-15) is compact and contains a structurally deviant CCP module". Journal of Molecular Biology. 395 (1): 105–122. doi:10.1016/j.jmb.2009.10.010. PMC 2806952. PMID 19835885.
- ^ Norman DG, Barlow PN, Baron M, Day AJ, Sim RB, Campbell ID (June 1991). "Three-dimensional structure of a complement control protein module in solution". Journal of Molecular Biology. 219 (4): 717–725. doi:10.1016/0022-2836(91)90666-T. PMID 1829116.
- ^ Barlow PN, Steinkasserer A, Norman DG, Kieffer B, Wiles AP, Sim RB, Campbell ID (July 1993). "Solution structure of a pair of complement modules by nuclear magnetic resonance". Journal of Molecular Biology. 232 (1): 268–284. doi:10.1006/jmbi.1993.1381. PMID 8331663.
- ^ Morgan HP, Mertens HD, Guariento M, Schmidt CQ, Soares DC, Svergun DI, et al. (2012). "Structural analysis of the C-terminal region (modules 18-20) of complement regulator factor H (FH)". PLOS ONE. 7 (2): e32187. Bibcode:2012PLoSO...732187M. doi:10.1371/journal.pone.0032187. PMC 3289644. PMID 22389686.
- ^ Herbert AP, Uhrín D, Lyon M, Pangburn MK, Barlow PN (June 2006). "Disease-associated sequence variations congregate in a polyanion recognition patch on human factor H revealed in three-dimensional structure". The Journal of Biological Chemistry. 281 (24): 16512–16520. doi:10.1074/jbc.M513611200. PMID 16533809.
- ^ Jokiranta TS, Jaakola VP, Lehtinen MJ, Pärepalo M, Meri S, Goldman A (April 2006). "Structure of complement factor H carboxyl-terminus reveals molecular basis of atypical haemolytic uremic syndrome". The EMBO Journal. 25 (8): 1784–1794. doi:10.1038/sj.emboj.7601052. PMC 1440827. PMID 16601698.
- ^ Prosser BE, Johnson S, Roversi P, Herbert AP, Blaum BS, Tyrrell J, et al. (October 2007). "Structural basis for complement factor H linked age-related macular degeneration". The Journal of Experimental Medicine. 204 (10): 2277–2283. doi:10.1084/jem.20071069. PMC 2118454. PMID 17893204.
- ^ Wu J, Wu YQ, Ricklin D, Janssen BJ, Lambris JD, Gros P (July 2009). "Structure of complement fragment C3b-factor H and implications for host protection by complement regulators". Nature Immunology. 10 (7): 728–733. doi:10.1038/ni.1755. PMC 2713992. PMID 19503104.
- ^ Morgan HP, Schmidt CQ, Guariento M, Blaum BS, Gillespie D, Herbert AP, et al. (April 2011). "Structural basis for engagement by complement factor H of C3b on a self surface". Nature Structural & Molecular Biology. 18 (4): 463–470. doi:10.1038/nsmb.2018. PMC 3512577. PMID 21317894.
- ^ Kajander T, Lehtinen MJ, Hyvärinen S, Bhattacharjee A, Leung E, Isenman DE, et al. (February 2011). "Dual interaction of factor H with C3d and glycosaminoglycans in host-nonhost discrimination by complement". Proceedings of the National Academy of Sciences of the United States of America. 108 (7): 2897–2902. Bibcode:2011PNAS..108.2897K. doi:10.1073/pnas.1017087108. PMC 3041134. PMID 21285368.
- ^ a b Aslam M, Perkins SJ (June 2001). "Folded-back solution structure of monomeric factor H of human complement by synchrotron X-ray and neutron scattering, analytical ultracentrifugation and constrained molecular modelling". Journal of Molecular Biology. 309 (5): 1117–1138. doi:10.1006/jmbi.2001.4720. PMID 11399083.
- ^ Kirkitadze MD, Barlow PN (April 2001). "Structure and flexibility of the multiple domain proteins that regulate complement activation". Immunological Reviews. 180: 146–161. doi:10.1034/j.1600-065X.2001.1800113.x. PMID 11414356. S2CID 25095717.
- ^ a b c d e f g h i j k l m n Tzoumas N, Hallam D, Harris CL, Lako M, Kavanagh D, Steel DH (November 2020). "Revisiting the role of factor H in age-related macular degeneration: Insights from complement-mediated renal disease and rare genetic variants". Survey of Ophthalmology. 66 (2): 378–401. doi:10.1016/j.survophthal.2020.10.008. PMID 33157112. S2CID 226274874.
- ^ Raychaudhuri S, Iartchouk O, Chin K, Tan PL, Tai AK, Ripke S, et al. (October 2011). "A rare penetrant mutation in CFH confers high risk of age-related macular degeneration". Nature Genetics. 43 (12): 1232–1236. doi:10.1038/ng.976. PMC 3225644. PMID 22019782.
- ^ Atkinson JP, Goodship TH (June 2007). "Complement factor H and the hemolytic uremic syndrome". The Journal of Experimental Medicine. 204 (6): 1245–1248. doi:10.1084/jem.20070664. PMC 2118604. PMID 17548524.
- ^ de Jorge EG, Macor P, Paixão-Cavalcante D, Rose KL, Tedesco F, Cook HT, et al. (January 2011). "The development of atypical hemolytic uremic syndrome depends on complement C5". Journal of the American Society of Nephrology. 22 (1): 137–145. doi:10.1681/ASN.2010050451. PMC 3014042. PMID 21148255.
- ^ a b Boyajyan A, Ghazaryan H, Stepanyan A, Zakharyan R (December 2013). "Genetic polymorphisms of complement factor H in schizophrenia and ischemic stroke". Mol. Immunol. 56 (3): 294. doi:10.1016/j.molimm.2013.05.154.
- ^ Luo S, Poltermann S, Kunert A, Rupp S, Zipfel PF (December 2009). "Immune evasion of the human pathogenic yeast Candida albicans: Pra1 is a Factor H, FHL-1 and plasminogen binding surface protein". Molecular Immunology. 47 (2–3): 541–550. doi:10.1016/j.molimm.2009.07.017. PMID 19850343.
- ^ Ram, S.; Sharma, A. K.; Simpson, S. D.; Gulati, S.; McQuillen, D. P.; Pangburn, M. K.; Rice, P. A. (1998-03-02). "A novel sialic acid binding site on factor H mediates serum resistance of sialylated Neisseria gonorrhoeae". The Journal of Experimental Medicine. 187 (5): 743–752. doi:10.1084/jem.187.5.743. PMC 2212180. PMID 9480984.
- ^ a b Zipfel PF, Hallström T, Riesbeck K (December 2013). "Human complement control and complement evasion by pathogenic microbes—tipping the balance". Molecular Immunology. 56 (3): 152–160. doi:10.1016/j.molimm.2013.05.222. PMID 23810413. S2CID 207007297.
- ^ Soames CJ, Sim RB (September 1997). "Interactions between human complement components factor H, factor I and C3b". The Biochemical Journal. 326 (Pt 2): 553–561. doi:10.1042/bj3260553. PMC 1218704. PMID 9291131.
- ^ Jokiranta TS, Westin J, Nilsson UR, Nilsson B, Hellwage J, Löfås S, et al. (March 2001). "Complement C3b interactions studied with surface plasmon resonance technique". International Immunopharmacology. 1 (3): 495–506. doi:10.1016/S1567-5769(00)00042-4. PMID 11367533.
- ^ Büttner-Mainik A, Parsons J, Jérôme H, Hartmann A, Lamer S, Schaaf A, et al. (April 2011). "Production of biologically active recombinant human factor H in Physcomitrella". Plant Biotechnology Journal. 9 (3): 373–383. doi:10.1111/j.1467-7652.2010.00552.x. PMID 20723134.
- ^ Schmidt CQ, Slingsby FC, Richards A, Barlow PN (April 2011). "Production of biologically active complement factor H in therapeutically useful quantities". Protein Expression and Purification. 76 (2): 254–263. doi:10.1016/j.pep.2010.12.002. PMC 4067574. PMID 21146613.
Further reading
- Bradley DT, Zipfel PF, Hughes AE (June 2011). "Complement in age-related macular degeneration: a focus on function". Eye. 25 (6): 683–693. doi:10.1038/eye.2011.37. PMC 3178140. PMID 21394116.
- Kardys I, Klaver CC, Despriet DD, Bergen AA, Uitterlinden AG, Hofman A, et al. (April 2006). "A common polymorphism in the complement factor H gene is associated with increased risk of myocardial infarction: the Rotterdam Study". Journal of the American College of Cardiology. 47 (8): 1568–1575. doi:10.1016/j.jacc.2005.11.076. PMID 16630992.
- Pío R, Elsasser TH, Martínez A, Cuttitta F (April 2002). "Identification, characterization, and physiological actions of factor H as an adrenomedullin binding protein present in human plasma". Microscopy Research and Technique. 57 (1): 23–27. doi:10.1002/jemt.10047. PMID 11921353. S2CID 37608883.
- Walport MJ (April 2001). "Complement. First of two parts". The New England Journal of Medicine. 344 (14): 1058–1066. doi:10.1056/NEJM200104053441406. PMID 11287977.
- Walport MJ (April 2001). "Complement. Second of two parts". The New England Journal of Medicine. 344 (15): 1140–1144. doi:10.1056/NEJM200104123441506. PMID 11297706.
External links
- GeneReviews/NCBI/NIH/UW entry on Atypical Hemolytic-Uremic Syndrome
- GeneReviews/NCBI/NIH/UW entry on Dense Deposit Disease/Membranoproliferative Glomerulonephritis Type II
- OMIM entries on Atypical Hemolytic-Uremic Syndrome
- Complement+Factor+H at the U.S. National Library of Medicine Medical Subject Headings (MeSH)