Common variable immunodeficiency
| Common variable immunodeficiency | |
|---|---|
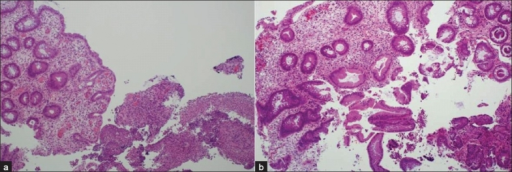 | |
| a)Colitis in common variable immunodeficiency showing acutely inflamed colonic tissue b) Chronic colonic crypt damage | |
Common variable immunodeficiency (CVID) is an immune disorder characterized by recurrent infections and low antibody levels, specifically in immunoglobulin (Ig) types IgG, IgM and IgA.[1] Generally symptoms include high susceptibility to foreign invaders, chronic lung disease, and inflammation and infection of the gastrointestinal tract.[1] However, symptoms vary greatly between people. "Variable" refers to the heterogeneous clinical manifestations of this disorder, which include recurrent bacterial infections, increased risk for autoimmune disease and lymphoma, as well as gastrointestinal disease.[2] CVID is a lifelong disease.
The cause of CVID is poorly understood. Deletions in genes that encode cell surface proteins and cytokine receptors, such as CD19, CD20, CD21, and CD80, is a likely cause.[3] A deletion is a mutation in which part of the chromosome is lost during DNA replication which may include several genes, or as few as a single base pair. Additionally, the disease is defined by T cell defects, namely reduced proliferative capacity.[4] The disease is hard to diagnose, taking on average 6–7 years after onset.[3][5] CVID is a primary immunodeficiency.[3]
Treatment options are limited, and usually include lifelong immunoglobulin replacement therapy.[5] This therapy is thought to help reduce bacterial infections. This treatment alone is not wholly effective, and many people still experience other symptoms like lung disease and noninfectious inflammatory symptoms.
CVID was first diagnosed over 60 years ago, and since has emerged as the predominant class of primary antibody deficiencies. CVID is formally diagnosed by levels of IgG and IgA more than two standard deviations below the norm, and no other cause for hypogammaglobulinemia, an abnormally low level of immunoglobulins in the blood. It is thought to affect between 1 in 25,000 to 1 in 50,000 people worldwide.
Signs and symptoms
The symptoms of CVID vary between people affected. Its main features are hypogammaglobulinemia and recurrent infections. Hypogammaglobulinemia manifests as a significant decrease in the levels of IgG antibodies, usually alongside IgA antibodies; IgM antibody levels are also decreased in about half of people.[6] Infections are a direct result of the low antibody levels in the circulation, which do not adequately protect them against pathogens. The microorganisms that most frequently cause infections in CVID are bacteria Haemophilus influenzae, Streptococcus pneumoniae, and Staphylococcus aureus. Pathogens less often isolated from people include Neisseria meningitidis, Pseudomonas aeruginosa, and Giardia lamblia. Infections mostly affect the respiratory tract (nose, sinuses, bronchi, lungs) and the ears; they can also occur at other sites, such as the eyes, skin, and gastrointestinal tract. These infections respond to antibiotics but can recur upon discontinuation of antibiotics. Bronchiectasis can develop when severe, recurrent pulmonary infections are left untreated.
In addition to infections, people with CVID can develop complications. These include:
- autoimmune manifestations, e.g. pernicious anemia, autoimmune haemolytic anemia (AHA), idiopathic thrombocytopenic purpura (ITP), psoriasis, vitiligo, rheumatoid arthritis, primary hypothyroidism, atrophic gastritis. Autoimmunity is the main type of complication in people with CVID, appearing in some form in up to 50% of individuals;
- malignancies, particularly Non-Hodgkin's lymphoma and gastric carcinoma;
- enteropathy, which manifests with a blunting of intestinal villi and inflammation, and is usually accompanied by symptoms such as abdominal cramps, diarrhea, constipation, and, in some cases, malabsorption and weight loss. Symptoms of CVID enteropathy are similar to those of celiac disease, but don't respond to a gluten-free diet. Infectious causes must be excluded before a diagnosis of enteropathy can be made, as people with CVID are more susceptible to intestinal infections, e.g. by Giardia lamblia;
- lymphocytic infiltration of tissues, which can cause enlargement of lymph nodes (lymphadenopathy), of the spleen (splenomegaly) and of the liver (hepatomegaly), as well as the formation of granulomas. In the lung this is known as Granulomatous–lymphocytic interstitial lung disease.
Anxiety and depression can occur as a result of dealing with the other symptoms.[7]
CVID patients generally complain of severe fatigue.[8]
Causes
The underlying causes of CVID are largely obscure.[5] Genetic mutations can be identified as the cause of disease in about 10% of people, while familial inheritance accounts for 10-25% of cases.[9] Rather than arising from a single genetic mutation, CVID seems to result from variety of mutations that all contribute to a failure in antibody production.
Mutations in the genes encoding ICOS, TACI, CD19, CD20, CD21, CD80 and BAFFR have been identified as causative of CVID.[9][10][11] Susceptibility to CVID may also be linked to the Major Histocompatibility Complex (MHC) of the genome, particularly to DR-DQ haplotypes.[12] A mutation in the NFKB2 gene has recently been shown to cause CVID-like symptoms in a murine model. The frequency of this NFKB2 mutation in the CVID population is, however, yet to be established.[13]
Diagnosis
According to a European registry study, the mean age at onset of symptoms was 26.3 years old.[14] As per the criteria laid out by ESID (European Society for Immunodeficiencies) and PAGID (Pan-American Group for Immunodeficiency), CVID is diagnosed if:[15]
- the person presents with a marked decrease of serum IgG levels (<4.5 g/L) and a marked decrease below the lower limit of normal for age in at least one of the isotypes IgM or IgA;
- the person is four years of age or older;
- the person lacks antibody immune response to protein antigens or immunization.
Diagnosis is chiefly by exclusion, i.e. alternative causes of hypogammaglobulinemia, such as X-linked agammaglobulinemia, must be excluded before a diagnosis of CVID can be made.
Diagnosis is difficult because of the diversity of phenotypes seen in people with CVID. For example, serum immunoglobulin levels in people with CVID vary greatly. Generally, people can be grouped as follows: no immunoglobulin production, immunoglobulin (Ig) M production only, or both normal IgM and IgG production.[3] Additionally, B cell numbers are also highly variable. 12% of people have no detectable B cells, 12% have reduced B cells, and 54% are within the normal range.[15] In general, people with CVID display higher frequencies of naive B cells and lower frequencies of class-switched memory B cells. Frequencies of other B cell populations, such as IgD memory B cells, transitional B cells, and CD21 B cells, are also affected, and are associated with specific disease features. Although CVID is often thought of as a serum immunoglobulin and B cell-mediated disease, T cells can display abnormal behavior. Affected individuals typically present with low frequencies of CD4+, a T-cell marker, and decreased circulation of regulatory T cells and iNKT cell. Notably, approximately 10% of people display CD4+ T cell counts lower than 200 cells/mm3; this particular phenotype of CVID has been named LOCID (Late Onset Combined Immunodeficiency), and has a poorer prognosis than classical CVID.
Types
| Type | OMIM | Gene |
|---|---|---|
| CVID1 | 607594 | ICOS |
| CVID2 | 240500 | TACI |
| CVID3 | 613493 | CD19 |
| CVID4 | 613494 | TNFRSF13C |
| CVID5 | 613495 | CD20 |
| CVID6 | 613496 | CD81 |
The following types of CVID have been identified, and correspond to mutations in different gene segments.
Treatment
Treatment consists of immunoglobulin replacement therapy, which replenishes Ig subtypes that the person lacks. This treatment is given at frequent intervals for life, and is thought to help reduce bacterial infections and boost immune function.[16] Before therapy begins, plasma donations are tested for known blood-borne pathogens, then pooled and processed to obtain concentrated IgG samples. Infusions can be administered in three different forms: intravenously (IVIg):,[17] subcutaneously (SCIg), and intramuscularly (IMIg).
The administration of intravenous immunoglobulins requires the insertion of a cannula or needle in a vein, usually in the arms or hands. Because highly concentrated product is used, IVIg infusions take place every 3 to 4 weeks. Subcutaneous infusions slowly release the Ig serum underneath the skin, again through a needle, and takes place every week.[18] Intramuscular infusions are no longer widely used, as they can be painful and are more likely to cause reactions.
People often experience adverse side effects to immunoglobulin infusions, including:
- swelling at the insertion site (common in SCIG)
- chills
- headache
- nausea (common in IVIG)
- fatigue (common in IVIG)
- muscle aches and pain, or joint pain
- fever (common in IVIG and rare in SCIG)
- hives (rare)
- thrombotic events (rare)
- aseptic meningitis (rare, more common in people with SLE)
- anaphylactic shock (very rare)
In addition to Ig replacement therapy, treatment may also involve immune suppressants, to control autoimmune symptoms of the disease, and high dose steroids like corticosteroids.[15] In some cases, antibiotics are used to fight chronic lung disease resulting from CVID.[19] The outlook for people varies greatly depending on their level of lung and other organ damage prior to diagnosis and treatment.
Epidemiology
CVID has an estimated prevalence of about 1:50,000 in caucasians.[20] The disease seems to be less prevalent amongst Asians and African-Americans. Males and females are equally affected; however, among children, boys predominate.[3] A recent study of people in European with primary immunodeficiencies found that 30% had CVID, as opposed to a different immunodeficiency.[9] 10-25% of people inherited the disease, typically through autosomal-dominant inheritance. Given the rarity of the disease, it is not yet possible to generalize on disease prevalence among ethnic and racial groups. CVID shortens the life-span; but no study currently has a median age recorded. One study suggests the median age of death for men and women is 42 and 44 years old, respectively but most patients involved in the study are still alive. [5] Those people with accompanying disorders had the worst prognosis and those people with CVID only had frequent infections had the longest survival rates, with life expectancy almost equalling that of the general UK population.[21] Additionally, people with CVID with one or more noninfectious complications have an 11 times higher risk of death as compared to people with only infections.
History
[15] Charles Janeway Sr. is generally credited with the first description of a case of CVID in 1953.[22] The case involved a 39-year-old who had recurrent infections, bronchiectasis, and meningitis.[9] Though described in 1953, there was no standard definition for CVID until the 1990s, which caused widespread confusion during diagnosis. During the 1990s, the European Society for Immunodeficiency (ESID) and Pan-American Group for Immunodeficiency (PAGID) developed diagnostic criteria, including minimum age of diagnosis and the need to exclude other conditions, to describe the disease. These criteria were published in 1999 and since that time, some aspects, like increasing the minimum age, have been changed.
Research
Current research is aimed at studying large cohorts of people with CVID in an attempt to better understand age of onset, as well as mechanism, genetic factors, and progression of the disease.[3]
Funding for research in the US is provided by the National Institutes of Health. Key research in the UK was previously funded by the Primary Immunodeficiency Association (PiA) until its closure in January 2012,[23] and funding is raised through the annual Jeans for Genes campaign. Current efforts are aimed at studying the following:[15]
- Causes of complications. Little is known about why such diverse complications arise during treatment
- Underlying genetic factors. Though many polymorphisms and mutations have been identified, their respective roles in CVID development are poorly understood, and not represented in all people with CVID.
- Finding new ways to study CVID. Given that CVID arises from more than one gene, gene knock-out methods are unlikely to be helpful. It is necessary to seek out disease related polymorphisms by screening large populations of people with CVID, but this is challenging given the rarity of the disease.
References
- ↑ 1.0 1.1 "Common Variable Immune Deficiency". Genetics Home Reference. Archived from the original on 24 September 2020. Retrieved 8 February 2016.
- ↑ Cunningham-Rundles, C. Clinical manifestations, epidemiology, and diagnosis of common variable immunodeficiency in adults. In: UpToDate, Notarangelo, LD, Feldweg, AM (Eds), UpToDate, Waltham, MA, 2020. Retrieved April 08, 2020.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 Abbott, Jordan K.; Gelfand, Erwin W. (2015). "Common Variable Immunodeficiency: Diagnosis, Management, and Treatment". Immunol Allergy Clin N Am. 35 (4): 637–658. doi:10.1016/j.iac.2015.07.009. PMID 26454311.
- ↑ Strober, Warren; Chua, Kevin (2000). "Common Variable Immunodeficiency". Clinical Reviews in Allergy and Immunology. 19 (2): 157–181. doi:10.1385/criai:19:2:157. PMID 11107500. S2CID 32349345. Archived from the original on 2021-06-02. Retrieved 2021-10-27.
- ↑ 5.0 5.1 5.2 5.3 Resnick, Elena S.; Cunningham-Rundles, Charlotte (2012). "The many faces of the clinical picture of common variable immune deficiency". Current Opinion in Allergy and Clinical Immunology. 12 (6): 595–601. doi:10.1097/aci.0b013e32835914b9. PMID 23026770. S2CID 205435779.
- ↑ Herriot R, Sewell WA (2008). "Antibody deficiency". Journal of Clinical Pathology. 61 (9): 994–1000. doi:10.1136/jcp.2007.051177. PMID 18755724. S2CID 25106807.
- ↑ Sanger, David E. "An Investigation of Coping and Psychosocial Functioning in Persons with Common Variable Immunodeficiency (CVID)" Archived 2003-07-28 at archive.today, Barts and The London NHS Trust, 2003, accessed August 7, 2011.
- ↑ "PatientsLikeMe - Symptoms". www.patientslikeme.com. Archived from the original on 14 April 2018. Retrieved 14 April 2018.
- ↑ 9.0 9.1 9.2 9.3 Park, Miguel A; Ti, James T; Hagan, John B; Maddox, Daniel E; Abraham, Roshini S (2008). "Common variable immunodeficiency: a new look at an old disease". The Lancet. 372 (9637): 9–15. doi:10.1016/s0140-6736(08)61199-x. PMID 18692715. S2CID 205951889.
- ↑ Salzer U, Neumann C, Thiel J, et al. (2008). "Screening of functional and positional candidate genes in families with common variable immunodeficiency". BMC Immunol. 9 (1): 3. doi:10.1186/1471-2172-9-3. PMC 2268914. PMID 18254984.
- ↑ Blanco-Quirós A, Solís-Sánchez P, Garrote-Adrados JA, Arranz-Sanz E (2006). "Common variable immunodeficiency. Old questions are getting clearer". Allergol Immunopathol (Madr). 34 (6): 263–75. doi:10.1157/13095875. hdl:10261/71519. PMID 17173844. Archived from the original on 2009-05-21. Retrieved 2008-03-01.
- ↑ O Olerup, O; Smith, CI; Björkander, J; Hammarström, L (Nov 15, 1992). "Shared HLA class II-associated genetic susceptibility and resistance, related to the HLA-DQB1 gene, in IgA deficiency and common variable immunodeficiency". PNAS. 89 (22): 10653–10657. Bibcode:1992PNAS...8910653O. doi:10.1073/pnas.89.22.10653. PMC 50399. PMID 1438261.
- ↑ Chen, Karin; Emily M. Coonrod; Attila Kumánovics; Zechariah F. Franks; Jacob D. Durtschi; Rebecca L. Margraf; Wilfred Wu; Nahla M. Heikal; Nancy H. Augustine; Perry G. Ridge; Harry R. Hill; Lynn B. Jorde; Andrew S. Weyrich; Guy A. Zimmerman; Adi V. Gundlapalli; John F. Bohnsack; Karl V. Voelkerding (17 October 2013). "Germline Mutations in NFKB2 Implicate the Noncanonical NF-κB Pathway in the Pathogenesis of Common Variable Immunodeficiency". The American Journal of Human Genetics. 93 (5): 812–24. doi:10.1016/j.ajhg.2013.09.009. PMC 3824125. PMID 24140114.
- ↑ Bonilla, Francisco A.; Geha, Raif S. (2009). "Common Variable Immunodeficiency". Pediatric Research. 65 (5): 13R–19R. doi:10.1203/pdr.0b013e31819dbf88. PMID 19190529. S2CID 9361175.
- ↑ 15.0 15.1 15.2 15.3 15.4 Chapel, Helen; Cunningham-Rundles, Charlotte (2009). "Update in understanding common variable immunodeficiency disorders (CVIDs) and the management of patients with these conditions". British Journal of Haematology. 145 (6): 709–727. doi:10.1111/j.1365-2141.2009.07669.x. PMC 2718064. PMID 19344423.
- ↑ "Primary immunodeficiency". Mayo Clinic. Archived from the original on 18 February 2019. Retrieved 17 February 2016.
- ↑ Pourpak Z, Aghamohammadi A, Sedighipour L, et al. (2006). "Effect of regular intravenous immunoglobulin therapy on prevention of pneumonia in patients with common variable immunodeficiency". J Microbiol Immunol Infect. 39 (2): 114–20. PMID 16604243. Archived from the original (abstract) on 2008-09-29. Retrieved 2008-03-01.
- ↑ Schwartz, Robert A; Modak, Rohit; Modak, Prema. "Common Variable Immunodeficiency Treatment and Management". Medscape. Archived from the original on 4 March 2016. Retrieved 17 February 2016.
- ↑ "Common Variable Immune Deficiency". Immune Deficiency Foundation. Archived from the original on 10 February 2016. Retrieved 16 February 2016.
- ↑ Common Variable Immunodeficiency : Article by Robert A Schwartz at eMedicine
- ↑ Chapel, Helen; Cunningham-Rundles, Charlotte (2009-06-01). "Update in understanding common variable immunodeficiency disorders (CVIDs) and the management of patients with these conditions". British Journal of Haematology. 145 (6): 709–727. doi:10.1111/j.1365-2141.2009.07669.x. ISSN 1365-2141. PMC 2718064. PMID 19344423.
- ↑ Janeway CA, Apt L, Gitlin D (1953). "Agammaglobulinemia". Trans Assoc Am Physicians. 66: 200–2. PMID 13136263.
- ↑ "Archived copy". Archived from the original on 2012-09-13. Retrieved 2012-10-26.
{{cite web}}: CS1 maint: archived copy as title (link)
- Moris G.; Garcia-Monco JC (1999). "The Challenge of Drug-Induced Aseptic Meningitis". Archives of Internal Medicine. 159 (11): 1185–1194. doi:10.1001/archinte.159.11.1185. PMID 10371226. (IVIG and Aseptic Meningitis, association with SLE)
External links
| Classification | |
|---|---|
| External resources |