Chorionic hematoma
| Chorionic hematoma | |
|---|---|
| Other names: Chorionic hemorrhage, chorionic bleed | |
| Ultrasound showing a subchorionic hemorrhage[1] | |
| Specialty | Obstetrics |
| Symptoms | None, vaginal bleeding, abdominal cramps[2] |
| Complications | Pregnancy loss, preterm delivery, preterm rupture of membranes[3][2] |
| Usual onset | 10 to 20 wks gestational age[2] |
| Causes | Unclear[2] |
| Risk factors | Miscarriage, uterine malformation, pelvic infections[2] |
| Diagnostic method | Ultrasound[2] |
| Differential diagnosis | Ectopic pregnancy, twins, miscarriage, implantation bleeding, placental abruption, placenta previa, gestational trophoblastic disease[2][4] |
| Treatment | Depends on symptoms and Rh status[2] |
| Frequency | 1 to 18% of pregnancies[5] |
Chorionic hematoma is the pooling of blood between the chorion, a membrane surrounding the embryo, and the uterine wall.[2][4] Symptoms may vary from none to vaginal bleeding.[2] There is generally no pain, though some may have cramps.[2] Large areas of bleeding are associated with pregnancy loss.[2] Other complications may include preterm delivery and preterm rupture of membranes.[3]
The cause is unclear.[2] Risk factors include previous miscarriage, uterine malformation, and pelvic infections.[2] The underlying mechanism is believed to involved detachment of the chorion from the uterus.[2] Diagnosis is by ultrasound.[2]
Treatment depends on the severity of symptoms.[2] In those who are RhD negative it should include anti-D immune globulin.[2] The risk of miscarriage, when a heart beat is present, is about 10%.[4]
Chorionic hematoma occurs in about 1 to 18% of pregnancies.[5] They most commonly present between 10 and 20 weeks of gestational age.[2] They were first described in 1981.[2]
Signs and symptoms
Most people with a small subchorionic hematoma are asymptomatic.[6] Symptoms include vaginal bleeding, abdominal pain, premature labor and threatened abortion.[7]
Pathophysiology
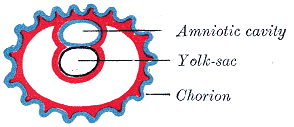
Chorionic hematomas are due to a separation of the chorion from the endometrium (inner membrane of the uterus).
Diagnosis
Ultrasonography is the preferred method of diagnosis.[8] A chorionic hematoma appears on ultrasound as a hypoechoic crescent adjacent to the gestational sac. The hematoma is considered small if it is under 20% of the size of the sac and large if it is over 50%.
Hematomas are classified by their location between tissue layers:[9]
- Subchorionic hematomas, the most common type, are between the chorion and endometrium.
- Retroplacental hematomas are entirely behind the placenta and not touching the gestational sac.
- Subamniotic or preplacental hematomas are contained within amnion and chorion. Rare.
Prognosis and treatment
The presence of subchorionic bleeding around the gestational sac is not association with miscarriage overall.[10][11] However, the case of intrauterine hematoma observed before 9 weeks of gestational age has been associated with an increased risk of miscarriage.[12] In one study women who complied with instructions for bed rest for the duration of bleeding had a lower rate of miscarriage and a higher rate of term pregnancy than non-compliant women. The study had several limitations; results were severely confounded by inherent differences between compliant and non-compliant women. [13]
References
- ↑ "UOTW #3 Answer - Ultrasound of the Week". Ultrasound of the Week. Archived from the original on 10 November 2015. Retrieved 27 May 2017.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 2.13 2.14 2.15 2.16 2.17 2.18 2.19 Bondick, CP; M Das, J; Fertel, H (January 2021). "Subchorionic Hemorrhage". PMID 32644443.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ 3.0 3.1 Tuuli, MG; Norman, SM; Odibo, AO; Macones, GA; Cahill, AG (May 2011). "Perinatal outcomes in women with subchorionic hematoma: a systematic review and meta-analysis". Obstetrics and gynecology. 117 (5): 1205–1212. doi:10.1097/AOG.0b013e31821568de. PMID 21508763.
- ↑ 4.0 4.1 4.2 Deutchman, M; Tubay, AT; Turok, D (1 June 2009). "First trimester bleeding". American family physician. 79 (11): 985–94. PMID 19514696.
- ↑ 5.0 5.1 Rumack, Carol M.; Levine, Deborah (2017). Diagnostic Ultrasound E-Book. Elsevier Health Sciences. p. 1069. ISBN 978-0-323-52963-1. Archived from the original on 28 August 2021. Retrieved 8 May 2021.
- ↑ Trop I, Levine D. Hemorrhage during pregnancy: sonography and MR imaging. AJR Am J Roentgenol. Mar 2001;176(3):607-15.
- ↑ Hodgson DT, Lotfipour S, Fox JC. Vaginal bleeding before 20 weeks gestation due to placental abruption leading to disseminated intravascular coagulation and fetal loss after appearing to satisfy criteria for routine threatened abortion: a case report and brief review of the literature. J Emerg Med. May 2007;32(4):387-92
- ↑ Abu-Yousef MM, Bleicher JJ, Williamson RA, Weiner CP. Subchorionic hemorrhage: sonographic diagnosis and clinical significance. AJR Am J Roentgenol. Oct 1987;149(4):737-40.
- ↑ Trop, Isabelle and Levine, Deborah. Hemorrhage During Pregnancy: Sonography and MR Imaging [1] Archived 2009-10-29 at the Wayback Machine. Amer J Roentgenology 2001; 176:607-615.
- ↑ "Miscarriage risk is not increased with subchorionic hematoma". www.mdedge.com. Archived from the original on 2019-11-12. Retrieved 2019-11-12.
- ↑ N. Stamatopoulos; C. Lu; F. Infante; U. Menakaya; I. Casikar; S. Reid; M. Mongelli; G. Condous (2013). "OP03.03: Does the presence of subchorionic haematoma increase the risk of miscarriage?". Ultrasound in Obstetrics & Gynecology. 42 (s1): 54. doi:10.1002/uog.12736.
- ↑ Maso, G.; Dʼottavio, G.; De Seta, F.; Sartore, A.; Piccoli, M.; Mandruzzato, G. (2005). "First-Trimester Intrauterine Hematoma and Outcome of Pregnancy". Obstetrics & Gynecology. 105 (2): 339–44. doi:10.1097/01.AOG.0000152000.71369.bd. PMID 15684162. S2CID 12502344.
- ↑ Ben-Haroush A, Yogev Y, Mashiach R, Meizner I. Pregnancy outcome of threatened abortion with subchorionic hematoma: possible benefit of bed-rest? Journal Isr Med Assoc J. 2003 Jun;5(6):422-4