Colestyramine
 | |
| Names | |
|---|---|
| Pronunciation | /koʊˈlɛstərəmiːn/, /koʊlɪˈstaɪrəmiːn/ |
| Trade names | Questran, Cholybar, Olestyr, others |
| Other names | Cholestyramine |
| Clinical data | |
| Drug class | Bile acid sequestrant[1] |
| Main uses | Biliary obstruction, liver disease, high lipids, chronic diarrhea[1][2] |
| Side effects | Abdominal discomfort, heart burn, nausea, excessive intestinal gas, constipation[1] |
| Pregnancy category |
|
| Routes of use | By mouth |
| External links | |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682672 |
| Legal | |
| Legal status |
|
| Pharmacokinetics | |
| Bioavailability | Low |
| Protein binding | Unknown |
| Metabolism | Bile acids |
| Elimination half-life | 1 hour |
| Excretion | Faecal |
| Chemical and physical data | |
| Molar mass | In average, exceeds 1×106 g/mol |
Colestyramine, sold under the brand name Questran among others, is a medication used to treat biliary obstruction, liver disease, high lipids, and certain types of chronic diarrhea.[1][2] For high lipids it is a second line treatment to statins.[1] In biliary obstruction it is used to improve itching.[3] It is taken by mouth.[3]
Side effects may include abdominal discomfort, heart burn, nausea, excessive intestinal gas, and constipation.[1] Other side effects may include fat soluble vitamin deficiency, osteoporosis, and hyperchloremic acidosis.[3] Safety in pregnancy is unclear.[3] It is a bile acid sequestrant, which binds bile in the gastrointestinal tract to prevent its reabsorption.[1] Low bile acid results in the liver producing less cholesterol.[1]
Cholestyramine was approved for medical use in the United States in 1973.[1] It is available as a generic medication.[1] In the United Kingdom 50 doses of 4 grams costs the NHS about £11 as of 2021.[2] In the United States this amount costs about 20 USD.[4]
Medical uses
Bile acid sequestrants such as colestyramine were first used to treat hypercholesterolemia, but since the introduction of statins, now have only a minor role for this. They can also be used to treat the pruritus, or itching, that often occurs during liver failure and other types of cholestasis where the ability to eliminate bile acids is reduced.
Diarrhea
Colestyramine is commonly used to treat diarrhea resulting from bile acid malabsorption.[5] It was first used for this in people with Crohn's disease who had undergone ileal resection.[6] The terminal portion of the small bowel (ileum) is where bile acids are reabsorbed. When this section is removed, the bile acids pass into the large bowel and cause diarrhea due to stimulation of chloride/fluid secretion by the colonocytes resulting in a secretory diarrhea. Colestyramine prevents this increase in water by making the bile acids insoluble and osmotically inactive.
Colestyramine is also used in the control of other types of bile acid diarrhea. The primary, idiopathic form of bile acid diarrhea is a common cause of chronic functional diarrhea, often misdiagnosed as diarrhea-predominant irritable bowel syndrome (IBS-D), and some respond to colestyramine.[7] It is beneficial in the treatment of postcholecystectomy syndrome chronic diarrhea.[8][9] Colestyramine is also useful in treating post-vagotomy diarrhea.[10][11]
Colestyramine can be helpful in the treatment of Clostridium difficile infections, to absorb toxins A and B, and reduce the diarrhea and the other symptoms these toxins cause. However, because it is not an anti-infective, it is used in concert with vancomycin.[12]
Toxins
It is also used in the "wash out" procedure in people taking leflunomide or teriflunomide to aid drug elimination in the case of drug discontinuation due to side effects caused by leflunomide or teriflunomide.[13]
Dosage
The usual dose is 4 grams, given one to six times per day usually before meals and at bedtime.[1]
Colestyramine is available as powder form, in 4-g packets, or in larger canisters.
Side effects
These side effects have been noted:[14]
- Most frequent: constipation
- Increased plasma triglycerides[15]
Intestinal obstruction has been reported in patients with previous bowel surgery who should use colestyramine cautiously.[16] [17] Cholestyramine-induced hyperchloremic metabolic acidosis has also been reported rarely.[18]
Patients with hypothyroidism, diabetes, nephrotic syndrome, dysproteinemia, obstructive liver disease, kidney disease, or alcoholism should consult their doctor before taking this medication.[14] Other drugs should be taken at least one hour before or four to six hours after colestyramine to reduce possible interference with absorption. Patients with phenylketonuria should consult with a physician before taking Questran Light because that product contains phenylalanine.
Interactions
Interactions with these drugs have been noted:[14]
- Digitalis
- Estrogens and progestins
- Oral diabetes drugs
- Penicillin G
- Phenobarbital
- Spironolactone
- Tetracycline
- Thiazide-type diuretic pills
- Thyroid medication
- Warfarin
- Leflunomide
Most interactions are due to the risk of decreased absorption of these drugs.[17] The duration of treatment is not limited, but the prescribing physician should reassess at regular intervals if continued treatment is still necessary. The principal overdose risk is blockage of intestine or stomach.
Colestyramine may interfere in the absorption of fat-soluble vitamins such as vitamins A, D, E, and K. No special considerations regarding alcohol consumption are made.[14]
Mechanism of action
It is a bile acid sequestrant, which binds bile in the gastrointestinal tract to prevent its reabsorption. It is a strong ion exchange resin, which means it can exchange its chloride anions with anionic bile acids in the gastrointestinal tract and bind them strongly in the resin matrix. The functional group of the anion exchange resin is a quaternary ammonium group attached to an inert styrene-divinylbenzene copolymer. Colestyramine removes bile acids from the body by forming insoluble complexes with bile acids in the intestine, which are then excreted in the feces.[19] As a result of this loss of bile acids, more plasma cholesterol is converted to bile acids in the liver to normalise levels.[19] This conversion of cholesterol into bile acids lowers plasma cholesterol levels.[19]
Society and culture
Cost
The cost of this medication in the U.S. is $69 (USD) for 378 grams (powder)[20]
-
Cholestyramine costs (US)
-
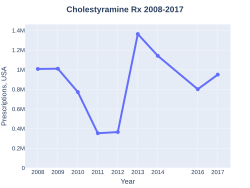
Cholestyramine prescriptions (US)
Research
A case report suggests it may be useful for cyanobacterial (microcystin) poisoning in dogs.[21]
Cholestyramine also binds with oxalate in the GI tract, ultimately reducing urine oxalate and calcium oxalate stone formation.[22]
Rferences
- The Merck Index (12 ed.). p. 2257.
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 "Cholestyramine". Archived from the original on 14 May 2021. Retrieved 4 January 2022.
- ↑ 2.0 2.1 2.2 BNF 81: March-September 2021. BMJ Group and the Pharmaceutical Press. 2021. p. 212. ISBN 978-0857114105.
- ↑ 3.0 3.1 3.2 3.3 "Cholestyramine Monograph for Professionals". Drugs.com. Archived from the original on 28 August 2021. Retrieved 4 January 2022.
- ↑ "Cholestyramine Prices, Coupons & Savings Tips - GoodRx". GoodRx. Archived from the original on 16 August 2021. Retrieved 4 January 2022.
- ↑ Wilcox C, Turner J, Green J (May 2014). "Systematic review: the management of chronic diarrhoea due to bile acid malabsorption". Aliment. Pharmacol. Ther. 39 (9): 923–39. doi:10.1111/apt.12684. PMID 24602022. S2CID 12016216.
- ↑ Hofmann AF, Poley JR (August 1969). "Cholestyramine treatment of diarrhea associated with ileal resection". N. Engl. J. Med. 281 (8): 397–402. doi:10.1056/NEJM196908212810801. PMID 4894463.
- ↑ Wedlake L, A'Hern R, Russell D, Thomas K, Walters JR, Andreyev HJ (October 2009). "Systematic review: the prevalence of idiopathic bile acid malabsorption as diagnosed by SeHCAT scanning in patients with diarrhoea-predominant irritable bowel syndrome". Aliment. Pharmacol. Ther. 30 (7): 707–17. doi:10.1111/j.1365-2036.2009.04081.x. PMID 19570102. S2CID 11327665.
- ↑ Sciarretta G, Furno A, Mazzoni M, Malaguti P (December 1992). "Post-cholecystectomy diarrhea: evidence of bile acid malabsorption assessed by SeHCAT test". Am. J. Gastroenterol. 87 (12): 1852–4. PMID 1449156.
- ↑ Danley T, St Anna L (October 2011). "Clinical inquiry. Postcholecystectomy diarrhea: what relieves it?". J Fam Pract. 60 (10): 632c–d. PMID 21977493.
- ↑ George, J. D.; Magowan, J. (1971). "Diarrhea after total and selective vagotomy". The American Journal of Digestive Diseases. 16 (7): 635–40. doi:10.1007/BF02239223. PMID 5563217. S2CID 45276562.
- ↑ Gorbashko, AI (1992). "The pathogenesis, diagnosis and treatment of postvagotomy diarrhea". Vestnik Khirurgii Imeni I. I. Grekova. 148 (3): 254–62. PMID 8594740.
- ↑ Stroehlein JR (June 2004). "Treatment of Clostridium difficile Infection". Curr Treat Options Gastroenterol. 7 (3): 235–239. doi:10.1007/s11938-004-0044-y. PMID 15149585. S2CID 25356792.
- ↑ Wong SP, Chu CM, Kan CH, Tsui HS, Ng WL (December 2009). "Successful treatment of leflunomide-induced acute pneumonitis with cholestyramine wash-out therapy". J Clin Rheumatol. 15 (8): 389–92. doi:10.1097/RHU.0b013e3181c3f87e. PMID 19955995.
- ↑ 14.0 14.1 14.2 14.3 "Questran". PDRHealth. Archived from the original on April 17, 2012. Retrieved July 7, 2012.
- ↑ MedlinePlus Encyclopedia: Triglyceride level
- ↑ Merten, DF; Grossman, H (1980). "Intestinal obstruction associated with cholestyramine therapy". American Journal of Roentgenology. 134 (4): 827–8. doi:10.2214/ajr.134.4.827. PMID 6767374.
- ↑ 17.0 17.1 Jacobson TA, Armani A, McKenney JM, Guyton JR (2007). "Safety considerations with gastrointestinally active lipid-lowering drugs". Am J Cardiol. 99 (6A): 47C–55C. doi:10.1016/j.amjcard.2006.11.022. PMID 17368279.
- ↑ Kamar, FB; McQuillan, RF (2015). "Hyperchloremic Metabolic Acidosis due to Cholestyramine: A Case Report and Literature Review". Case Reports in Nephrology. 2015: 309791. doi:10.1155/2015/309791. PMC 4573617. PMID 26425378.
- ↑ 19.0 19.1 19.2 http://livertox.nih.gov/Cholestyramine.htm Archived 2016-12-01 at the Wayback Machine, United States National Institutes of Health (page visited on 22 June 2016).
- ↑ "Cholestyramine Prices, Coupons & Patient Assistance Programs". Drugs.com. Archived from the original on 28 August 2021. Retrieved 26 March 2021.
- ↑ Rankin KA, Alroy KA, Kudela RM, Oates SC, Murray MJ, Miller MA (2013). "Treatment of cyanobacterial (microcystin) toxicosis using oral cholestyramine: case report of a dog from Montana". Toxins (Basel). 5 (6): 1051–63. doi:10.3390/toxins5061051. PMC 3717769. PMID 23888515.
- ↑ "Kidney Stones – Medications". The New York Times. Archived from the original on 2013-11-21.
External links
| Identifiers: |
|
|---|
- Pages using duplicate arguments in template calls
- Webarchive template wayback links
- Drugs with non-standard legal status
- Infobox-drug molecular-weight unexpected-character
- Chemical articles with unknown parameter in Infobox drug
- Chemical articles without CAS registry number
- Articles without EBI source
- Chemical pages without ChemSpiderID
- Chemical pages without DrugBank identifier
- Articles without KEGG source
- Articles without InChI source
- Articles without UNII source
- Drugs missing an ATC code
- Drugboxes which contain changes to verified fields
- Chemicals that do not have a ChemSpider ID assigned
- Articles with changed EBI identifier
- Hepatology
- Bile acid sequestrants
- RTT