Central retinal artery occlusion
| Central retinal artery occlusion | |
|---|---|
 | |
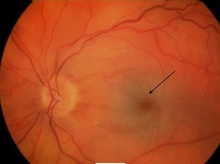
| Cherry red spot in a person with central retinal artery occlusion | |
| Specialty | Ophthalmology |
| Symptoms | Painless loss of vision in one eye[1] |
| Usual onset | Sudden[1] |
| Causes | Atherosclerosis, vasculitis, collagen-vascular disease, hypercoagulable state[2] |
| Differential diagnosis | Anterior ischemic optic neuropathy, retinal detachment, vitreous bleed[2] |
| Treatment | Controversial[3] |
| Prognosis | Permanent vision loss[1] |
| Frequency | 1 in 50,000 people per year[3] |
Central retinal artery occlusion (CRAO) is the sudden blockage of the central retinal artery of the eye.[2] Symptoms include painless loss of vision in one eye.[1] Onset is sudden.[1] Complications can include glaucoma and vitreous bleeding.[1]
Causes may include atherosclerosis, collagen-vascular disease, inflammatory conditions, and hypercoagulable states.[2] It most commonly occurs due to an embolism, possibly from the carotid arteries or heart valves.[2] Other causes include vasculitis related to lupus or temporal arteritis.[1] Risk factors include high blood pressure, smoking, and diabetes.[2] Diagnosis is by funduscopic examination.[1]
Treatment is controversial.[3] Efforts may include decreasing intraocular pressure to try to dislodge the clot.[1] This may be done with the use of timolol eye drops or acetazolamide.[1] Some have tried massage of the eye and thrombolysis is being studied.[1][3] Some degree of permanent vision loss in the effected eye often results.[1]
CRAO occurs in about 1 in 50,000 people a year.[3] It occurs more commonly in older people; with more than 90% of cases occurring in people over the age of 40.[3][4] Males are affected more often than females.[4] The condition was first described in 1859 by von Graefe.[4]
Signs and symptoms
[[File:|thumb|390x390px||alt=]] Central retinal artery occlusion is characterized by painless, acute vision loss in one eye.[5] Upon fundoscopic exam, one would expect to find: cherry-red spot (90%) (a morphologic description in which the normally red background of the choroid is sharply outlined by the swollen opaque retina in the central retina), retinal opacity in the posterior pole (58%), pallor (39%), retinal arterial attenuation (32%), and optic disk edema (22%).[5] During later stages of onset, one may also find plaques, emboli, and optic atrophy.[5]
Causes
CRAO can be classified based on it pathogenesis, as arteritic versus non-arteritic.[6][5][7] Non-arteritic CRAO is most commonly caused by an embolus and occlusion at the narrowest part of the carotid retinal artery due to plaques in the carotid artery resulting in carotid retinal artery atherosclerosis.[5][6][7] Further causes of non-arteritic CRAO may include vasculitis and chronic systemic autoimmune diseases.[6] Arteritic CRAO is most commonly caused by giant cell arteritis.[6][7] Other causes can include dissecting aneurysms and arterial spasms, and as a complication of patient positioning causing external compression of the eye compressing flow to the central retinal artery (e.g. in spine surgeries in the prone position).[8]
Risk factors include : being over 50 years of age, male gender, smoking, hypertension, tranexamic acid, diabetes mellitus, dyslipidemia, angina, valvular disease, transient hemiparesis, cancer, hypercoagulable blood conditions, lupus, or a family history of cerebrovascular or cardiovascular issues.[9][10] Additional risk factors include endocarditis, atrial myxoma, inflammatory diseases of the blood vessels, and predisposition to forming blood clots.
Mechanism
The ophthalmic artery branches off into the central retinal artery which travels with the optic nerve until it enters the eye.[11] This central retinal artery provides nutrients to the retina of the eye, more specifically the inner retina and the surface of the optic nerve.[11] Variations, such as branch retinal artery occlusion, can also occur.[11] Central retinal artery occlusion is most often due to emboli blocking the artery and therefore prevents the artery from delivering nutrients to most of the retina.[12] These emboli originate from the carotid arteries most of the time but in 25% of cases, this is due to plaque build-up in the ophthalmic artery.[12] The most frequent site of blockage is at the most narrow part of the artery which is where the artery pierces the dura covering the optic nerve.[12] Some people have cilioretinal arterial branches, which may or may not be included in the blocked portion.[12]
Diagnosis
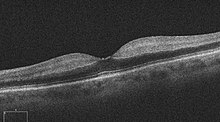
One diagnostic method for the confirmation of CRAO is fluorescein angiography, it is used to examine the retinal artery filling time after the fluorescein dye is injected into the peripheral venous system.[13] In an eye with CRAO some branches of the retinal artery may not fill or the time it takes for the branches of the retinal artery to fill will be increased, which is visualized by the leading edge of the fluorescein moving slower than normal through the retinal artery branches to the edges of the retina.[13] Fluorescein angiography can also be used to determine the extent of the occlusion as well as classify it into one of four types non-arteritic CRAO, non-arteritic CRAO with cilioretinal artery sparing, transient non-arteritic CRAO and arteritic CRAO.[14] Optical coherence tomography (OCT) may also be used to confirm the diagnosis of CRAO.[15]
-
Cherry-red spot with retinal pallor typical of central retinal artery occlusion
-
Fluorescein angiogram of a person with central retinal artery occlusion
-
Ocular coherence tomogram (OCT) of a person with central retinal artery occlusion
Treatment
While no treatment has clearly been demonstrated to be of benefit, the following have been tried:[16]
- Lowering intraocular pressure;
- Dilating the CRA;
- Increasing oxygenation;
- Isovolemic hemodilution;
- Anticoagulation;
- Dislodging or fragmenting thrombus or embolus;
- Thrombolysis; and
- Hyperbaric oxygen.
To achieve the best outcome for a person with CRAO, it is important to identify the condition in a timely manner and to refer to the appropriate specialist.[16]
Prognosis
The artery can re-canalize over time and the edema can clear. However, optic atrophy leads to permanent loss of vision. Irreversible damage to neural tissue can occur after approximately 15 minutes of complete blockage to the central retinal artery, but this time may vary between people.[17] Two thirds of people experience 20/400 vision while only one in six will experience 20/40 vision or better.[18]
Epidemiology
CRAO occurs in approximately 1 in 100,000 people.[9]
See also
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 "Central Retinal Artery Occlusion and Branch Retinal Artery Occlusion - Eye Disorders". Merck Manuals Professional Edition. Archived from the original on 30 October 2021. Retrieved 23 January 2022.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 Farris, William; Waymack, James R. (2022). "Central Retinal Artery Occlusion". StatPearls. StatPearls Publishing. Archived from the original on 23 January 2022. Retrieved 23 January 2022.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 Mac Grory, Brian; Lavin, Patrick; Kirshner, Howard; Schrag, Matthew (February 2020). "Thrombolytic Therapy for Acute Central Retinal Artery Occlusion". Stroke. 51 (2): 687–695. doi:10.1161/STROKEAHA.119.027478.
- ↑ 4.0 4.1 4.2 Wilkinson, Charles P.; Hinton, David R.; Sadda, SriniVas R.; Wiedemann, Peter (17 April 2017). Ryan's Retina E-Book. Elsevier Health Sciences. p. 1136. ISBN 978-0-323-40198-2. Archived from the original on 23 January 2022. Retrieved 23 January 2022.
- ↑ 5.0 5.1 5.2 5.3 5.4 Varma DD, Cugati S, Lee AW, Chen CS (June 2013). "A review of central retinal artery occlusion: clinical presentation and management". Eye. 27 (6): 688–97. doi:10.1038/eye.2013.25. PMC 3682348. PMID 23470793.
- ↑ 6.0 6.1 6.2 6.3 Hayreh SS (December 2018). "Central retinal artery occlusion". Indian Journal of Ophthalmology. 66 (12): 1684–1694. doi:10.4103/ijo.IJO_1446_18. PMC 6256872. PMID 30451166.
- ↑ 7.0 7.1 7.2 Dattilo M, Biousse V, Newman NJ (February 2017). "Update on the Management of Central Retinal Artery Occlusion". Neurologic Clinics. Neuro-Ophthalmology. 35 (1): 83–100. doi:10.1016/j.ncl.2016.08.013. PMID 27886897.
- ↑ Central and branch retinal artery occlusion. Uptodate.com. Mar 14, 2012.
- ↑ 9.0 9.1 Farris W, Waymack JR (2019). "Central Retinal Artery Occlusion". StatPearls. StatPearls Publishing. PMID 29262124. Archived from the original on 2022-01-23. Retrieved 2019-11-25.
- ↑ Limaye K, Wall M, Uwaydat S, Ali S, Shaban A, Al Kasab S, Adams H (October 2018). "Is Management of Central Retinal Artery Occlusion the Next Frontier in Cerebrovascular Diseases?". Journal of Stroke and Cerebrovascular Diseases. 27 (10): 2781–2791. doi:10.1016/j.jstrokecerebrovasdis.2018.06.006. PMID 30060907. Archived from the original on 2022-01-23. Retrieved 2021-10-03.
- ↑ 11.0 11.1 11.2 Louw L (July 2015). "Different ophthalmic artery origins: Embryology and clinical significance". Clinical Anatomy. 28 (5): 576–83. doi:10.1002/ca.22470. PMID 25255996. S2CID 28263732.
- ↑ 12.0 12.1 12.2 12.3 Michalinos A, Zogana S, Kotsiomitis E, Mazarakis A, Troupis T (2015). "Anatomy of the Ophthalmic Artery: A Review concerning Its Modern Surgical and Clinical Applications". Anatomy Research International. 2015: 591961. doi:10.1155/2015/591961. PMC 4655262. PMID 26635976.
- ↑ 13.0 13.1 "Retinal Artery Occlusion - EyeWiki". eyewiki.aao.org. Archived from the original on 2020-08-11. Retrieved 2019-11-25.
- ↑ Hayreh SS (December 2018). "Central retinal artery occlusion". Indian Journal of Ophthalmology. 66 (12): 1684–1694. doi:10.4103/ijo.IJO_1446_18. PMC 6256872. PMID 30451166.
- ↑ Coady, Patrick A.; Cunningham, Emmett T.; Vora, Robin A.; McDonald, H. Richard; Johnson, Robert N.; Jumper, J. Michael; Fu, Arthur D.; Haug, Sara J.; Williams, Steven L.; Lujan, Brandon J. (2015). "Spectral domain optical coherence tomography findings in eyes with acute ischaemic retinal whitening". The British Journal of Ophthalmology. 99 (5): 586–592. doi:10.1136/bjophthalmol-2014-304900. ISSN 1468-2079. PMID 24993106. S2CID 40051575.
- ↑ 16.0 16.1 Chronopoulos A, Schutz JS (2019). "Central retinal artery occlusion-A new, provisional treatment approach". Survey of Ophthalmology. 64 (4): 443–451. doi:10.1016/j.survophthal.2019.01.011. PMID 30707925.
- ↑ Tobalem S, Schutz JS, Chronopoulos A (April 2018). "Central retinal artery occlusion - rethinking retinal survival time". BMC Ophthalmology. 18 (1): 101. doi:10.1186/s12886-018-0768-4. PMC 5907384. PMID 29669523.
- ↑ Kunimoto, Dr., Lecture, Vascular diseases of the retina, AT Still University SOMA, October 2012
External links
| External resources |
|---|