Mirtazapine
 | |
 | |
| Names | |
|---|---|
| Trade names | Remeron, Mirataz, others |
| Other names | Mepirzapine; 6-azamianserin; ORG-3770[1][2] |
| |
| Clinical data | |
| Drug class | Tetracyclic antidepressant (TeCA)[3] |
| Main uses | depression[4][3] |
| Side effects | Increased weight, sleepiness, dizziness[3] |
| Pregnancy category | |
| Routes of use | By mouth (tablets), Topical |
| Defined daily dose | 30 mg[6] |
| External links | |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a697009 |
| Legal | |
| License data |
|
| Legal status | |
| Pharmacokinetics | |
| Bioavailability | 50%[7][8][9][10] |
| Protein binding | 85%[7][8][9][10] |
| Metabolism | Liver (CYP1A2, CYP2D6, CYP3A4)[7][8][9][10][4] |
| Metabolites | Desmethylmirtazapine (contributes 3–10% of activity)[4] |
| Elimination half-life | 20–40 hours[7][8][9][10] |
| Excretion | Urine: 75%[7] Feces: 15%[7][8][9][10] |
| Chemical and physical data | |
| Formula | C17H19N3 |
| Molar mass | 265.360 g·mol−1 |
| 3D model (JSmol) | |
| Chirality | Racemic mixture |
| Density | 1.22 g/cm3 |
| Melting point | 114 to 116 °C (237 to 241 °F) |
| Boiling point | 432 °C (810 °F) |
| Solubility in water | Soluble in methanol and chloroform mg/mL (20 °C) |
| |
| |
Mirtazapine, sold under the brand name Remeron among others, is an antidepressant primarily used to treat depression.[4][3] Its full effect may take more than four weeks to occur, with some benefit possibly as early as one to two weeks.[11][3] Often it is used in depression complicated by anxiety or trouble sleeping.[4][12] Effectiveness is similar to other antidepressants.[13] It is taken by mouth.[3]
Common side effects include increased weight, sleepiness, and dizziness.[3] Serious side effects may include mania, low white blood count, and increased suicide among children.[3] Withdrawal symptoms may occur with stopping.[14] It is not recommended together with an MAO inhibitor.[3] It is unclear if use during pregnancy is safe.[3] How it works is not clear, but it may involve blocking certain adrenergic and serotonin receptors.[4][3] Chemically, it is a tetracyclic antidepressant (TeCA).[3] It also has strong antihistamine effects.[4][3]
Mirtazapine came into medical use in the United States in 1996.[3] The patent expired in 2004, and generic versions are available.[15][3] In the United States the wholesale cost as of 2018 is about US$3 per month.[16] In the United Kingdom a month supply costs the NHS about £1.60 per month as of 2018.[17] In 2017, it was the 119th most commonly prescribed medication in the United States, with more than six million prescriptions.[18][19]
Medical uses
Depression
Mirtazapine is primarily used for major depressive disorder and other mood disorders.[20][21] Onset of action appears faster than some selective serotonin reuptake inhibitors (SSRI) and similar to tricyclic antidepressants.[22][11]
In 2010 NICE recommended generic SSRIs as first line choices, as they are "equally effective as other antidepressants and have a favourable risk–benefit ratio."[23] With respect to mirtazapine, it found: "There is no difference between mirtazapine and other antidepressants on any efficacy measure, although in terms of achieving remission mirtazapine appears to have a statistical though not clinical advantage. In addition, mirtazapine has a statistical advantage over selective serotonin reuptake inhibitors (SSRI) in terms of reducing symptoms of depression, but the difference is not clinically important. However, there is strong evidence that patients taking mirtazapine are less likely to leave treatment early because of side effects, although this is not the case for patients reporting side effects or leaving treatment early for any reason."[24]
A 2011 Cochrane review that compared mirtazapine to other antidepressants found that, while it appears to have a faster onset in people for whom it works (measured at two weeks), its efficacy is about the same as other antidepressants after six weeks' use.[11]
A 2012 review focused on antidepressants and sleep found that in many people with sleep disorders caused by depression, mirtazapine reduces the time it takes to fall asleep and increases the quality of sleep, but that in some people it can disturb sleep, especially at higher doses, causing restless leg syndrome in 8 to 28% of people and in rare cases causes REM sleep behavior disorder.[25]
A 2018 analysis of 21 antidepressants found them to be fairly similar overall.[26] It found tentative evidence for mirtazapine being in the more effective group and middle in tolerability.[26]
After one week of usage, mirtazapine was found to have an earlier onset of action compared to SSRIs.[22][27]
Other
There is also some tentative evidence supporting its use in treating the following conditions, for which it is sometimes prescribed off-label:
Dosage
The defined daily dose is 30 mg by mouth.[6] Higher doses do not result in greater benefit yet significantly increases side effects.[13]
Side effects
A 2011 Cochrane review found that compared with other antidepressants, it is more likely to cause weight gain and sleepiness, but it is less likely to cause tremor than tricyclic antidepressants, and less likely to cause nausea and sexual dysfunction than SSRIs.[11]
Very common (≥10% incidence) adverse effects include constipation, dry mouth, sleepiness, increased appetite (17%) and weight gain (>7% increase in <50% of children).[8][9][10][41][42][43][44][45][46]
Common (1–10% incidence) adverse effects include weakness, confusion, dizziness, fasciculations, peripheral edema, and negative lab results like elevated transaminases, elevated serum triglycerides, and elevated total cholesterol.[10]
Mirtazapine is not considered to have a risk of many of the side effects often associated with other antidepressants like the SSRIs, and may actually improve certain ones when taken in conjunction with them.[4][47] (Those adverse effects include decreased appetite, weight loss, insomnia, nausea and vomiting, diarrhoea, urinary retention, increased body temperature, excessive sweating, pupil dilation and sexual dysfunction.[4][47])
In general, some antidepressants, especially selective serotonin reuptake inhibitors (SSRI), can paradoxically exacerbate some peoples' depression or anxiety or cause suicidal ideation.[48] Despite its sedating action, mirtazapine is also believed to be capable of this, so in the United States and certain other countries, it carries a black box label warning of these potential effects, especially for people under the age of 25.[3]
A case report published in 2000 noted an instance in which mirtazapine counteracted the action of clonidine, causing a dangerous rise in blood pressure.[49]
Discontinuation syndrome
Mirtazapine and other antidepressants may cause a discontinuation syndrome upon cessation.[4][50][51] A gradual and slow reduction in dose is recommended to minimize discontinuation symptoms.[52] Effects of sudden cessation of treatment with mirtazapine may include depression, anxiety, tinnitus, panic attacks, vertigo, restlessness, irritability, decreased appetite, insomnia, diarrhea, nausea, vomiting, flu-like symptoms such as allergies and pruritus, headaches and sometimes hypomania or mania.[50][53][54][55][56]
Overdose
Mirtazapine is considered to be relatively safe in the event of an overdose,[27] although it is considered slightly more toxic in overdose than most of the SSRIs (except citalopram).[57] Unlike the tricyclic antidepressants, mirtazapine showed no significant cardiovascular adverse effects at 7 to 22 times the maximum recommended dose.[47] Case reports of overdose with as much as 30 to 50 times the standard dose described the drug as relatively nontoxic, compared to tricyclic antidepressants.[58][59]
Twelve reported fatalities have been attributed to mirtazapine overdose.[60][61] The fatal toxicity index (deaths per million prescriptions) for mirtazapine is 3.1 (95% CI: 0.1 to 17.2). This is similar to that observed with SSRIs.[62]
Interactions
Concurrent use with inhibitors or inducers of the cytochrome (CYP) P450 isoenzymes CYP1A2, CYP2D6, and/or CYP3A4 can result in altered concentrations of mirtazapine, as these are the main enzymes responsible for its metabolism.[7][4] As examples, fluoxetine and paroxetine, inhibitors of these enzymes, are known to modestly increase mirtazapine levels, while carbamazepine, an inducer, considerably decreases them.[7] Liver impairment and moderate chronic kidney disease have been reported to decrease the oral clearance of mirtazapine by about 30%; severe kidney disease decreases it by 50%.[7]
Mirtazapine in combination with an SSRI, SNRI, or TCA as an augmentation strategy is considered to be relatively safe and is often employed therapeutically,[47] with a combination of venlafaxine and mirtazapine, sometimes referred to as "California rocket fuel".[63][64] Several case reports document serotonin syndrome induced by the combination of mirtazapine with other agents (olanzapine,[65] quetiapine,[66] tramadol and venlafaxine[67]).
According to information from the manufacturers, mirtazapine should not be started within two weeks of any monoamine oxidase inhibitor (MAOI) usage; likewise, MAOIs should not be administered within two weeks of discontinuing mirtazapine.[3]
The addition of mirtazapine to an monoamine oxidase inhibitor (MAOI), while potentially having typical or idiosyncratic (unique to the individual) reactions not herein described, does not appear to cause serotonin syndrome.[68] This is in accordance with the fact that the 5-HT2A receptor is the predominant serotonin receptor thought to be involved in the pathophysiology of serotonin syndrome (with the 5-HT1A receptor seeming to be protective).[69][68] Mirtazapine is a potent 5-HT2A receptor antagonist, and cyproheptadine, a drug that shares this property, mediates recovery from serotonin syndrome and is an antidote against it.[69][70]
Pharmacology
Pharmacodynamics
| Ki (nM) | Species | Ref | |
|---|---|---|---|
| SERT | >10,000 | Human | [72][73] |
| NET | ≥4,600 | Human | [74][72] |
| DAT | >10,000 | Human | [72][73] |
| 5-HT1A | 3,330–5,010 | Human | [4][73] |
| 5-HT1B | 3,534–12,600 | Human | [4][73] |
| 5-HT1D | 794–5,010 | Human | [4][73] |
| 5-HT1E | 728 | Human | [73] |
| 5-HT1F | 583 | Human | [73] |
| 5-HT2A | 6.3–69 | Human | [4][73] |
| 5-HT2B | 200 | Human | [4] |
| 5-HT2C | 8.9–39 | Human | [4][73] |
| 5-HT3 | 8.1 | Human | [75] |
| 5-HT4L | >10,000 | Human | [73] |
| 5-HT5A | 670 | Human | [73] |
| 5-HT6 | ND | ND | ND[73] |
| 5-HT7 | 265 | Human | [73] |
| α1A | 1,815 | Human | [73] |
| α2A | 20 | Human | [73] |
| α2B | 88 | Human | [73] |
| α2C | 18 | Human | [73] |
| β | >10,000 | Human | [73] |
| D1 | 4,167 | Rat | |
| D2 | >5,454 | Human | [73] |
| D3 | 5,723 | Human | [73] |
| D4 | 2,518 | Human | [73] |
| H1 | 0.14–1.6 | Human | [76][4][73] |
| H2 | >10,000 | Rat | [77][76] |
| H3 | 83,200 | Human | [76] |
| H4 | >100,000 | Human | [76] |
| mACh | 670 | Human | [4][74] |
| VGSC | 6,905 | Rat | [73] |
| VDCC | >10,000 | Rat | [73] |
| Values are Ki (nM). The smaller the value, the more strongly the drug binds to the site. | |||
Mirtazapine is sometimes described as a noradrenergic and specific serotonergic antidepressant (NaSSA),[4] although the actual evidence in support of this label has been regarded as poor.[69] It is a tetracyclic piperazine-azepine.[78]
Mirtazapine has antihistamine, α2-blocker, and antiserotonergic activity.[4][79] It is specifically a potent antagonist or inverse agonist of the α2A-, α2B-, and α2C-adrenergic receptors, the serotonin 5-HT2A, 5-HT2C, and the histamine H1 receptor.[4][79] Unlike many other antidepressants, it does not inhibit the reuptake of serotonin, norepinephrine, or dopamine,[4][79] nor does it inhibit monoamine oxidase.[80] Similarly, mirtazapine has weak or no activity as an anticholinergic or blocker of sodium or calcium channels, in contrast to most TCAs.[4][73][79] In accordance, it has better tolerability and low toxicity in overdose.[4][81] As an H1 receptor antagonist, mirtazapine is extremely potent, and is in fact the most potent of all the TCAs and TeCAs.[74][82][83] Antagonism of the H1 receptor is by far the strongest activity of mirtazapine, with the drug acting as a selective H1 receptor antagonist at low concentrations.[4][73]
The (S)-(+) enantiomer of mirtazapine is responsible for antagonism of the serotonin 5-HT2A and 5-HT2C receptors,[84] while the (R)-(–) enantiomer is responsible for antagonism of the 5-HT3 receptor.[84] Both enantiomers are involved in antagonism of the H1 and α2-adrenergic receptors,[9][84] although the (S)-(+) enantiomer is the stronger antihistamine.[85]
Although not clinically relevant, mirtazapine has been found to act as a partial agonist of the κ-opioid receptor at high concentrations (EC50 = 7.2 μM).[86]
α2-Adrenergic receptor
Antagonism of the α2-adrenergic receptors, which function largely as inhibitory autoreceptors and heteroreceptors, enhances adrenergic and serotonergic neurotransmission, notably central 5-HT1A receptor mediated transmission in the dorsal raphe nucleus and hippocampus; hence, mirtazapine's classification as a NaSSA. Indirect α1 adrenoceptor-mediated enhancement of serotonin cell firing and direct blockade of inhibitory α2 heteroreceptors located on serotonin terminals are held responsible for the increase in extracellular serotonin.[4][20][87][88][89] Because of this, mirtazapine has been said to be a functional "indirect agonist" of the 5-HT1A receptor.[88] Increased activation of the central 5-HT1A receptor is thought to be a major mediator of efficacy of most antidepressant drugs.[90]
5-HT2 receptor
Antagonism of the 5-HT2 subfamily of receptors and inverse agonism of the 5-HT2C receptor appears to be in part responsible for mirtazapine's efficacy in the treatment of depressive states.[91][92] Mirtazapine increases dopamine release in the prefrontal cortex.[93][94] Accordingly, it was shown that by blocking the α2-adrenergic receptors and 5-HT2C receptors mirtazapine disinhibited dopamine and norepinephrine activity in these areas in rats.[95] In addition, mirtazapine's antagonism of 5-HT2A receptors has beneficial effects on anxiety, sleep and appetite, as well as sexual function regarding the latter receptor.[4][47] Mirtazapine has been shown to lower drug seeking behaviour in various human and animal studies.[96][97][98] It is also being investigated in substance abuse disorders to reduce withdrawal effects and improve remission rates.[96][99][100][101]
Mirtazapine significantly improves pre-existing symptoms of nausea, vomiting, diarrhea, and irritable bowel syndrome in afflicted individuals.[102] Mirtazapine may be used as an inexpensive antiemetic alternative to ondansetron.[36] In conjunction with substance abuse counseling, mirtazapine has been investigated for the purpose of reducing methamphetamine use in dependent individuals with success.[97][99][100][101] In contrast to mirtazapine, the selective serotonin reuptake inhibitors (SSRI), serotonin–norepinephrine reuptake inhibitors (SNRI), Monoamine oxidase inhibitors (MAOI), and some Tricyclic antidepressants (TCA) increase the general activity of the 5-HT2A, 5-HT2C, and 5-HT3 receptors leading to a host of negative changes and side effects, the most prominent of which including anorexia, insomnia, sexual dysfunction (loss of libido and anorgasmia), nausea, and diarrhea, among others. As a result, it is often combined with these drugs to reduce their side-effect profile and to produce a stronger antidepressant effect.[47][103]
Mirtazapine does not have serotonergic activity and does not cause serotonergic side effects or serotonin syndrome.[69][68] This is in accordance with the fact that it is not a serotonin reuptake inhibitor or monoamine oxidase inhibitor (MAOI), nor a serotonin receptor agonist.[69][68] There are no reports of serotonin syndrome in association with mirtazapine alone, and mirtazapine has not been found to cause serotonin syndrome in overdose.[69][68][104] However, there are a handful of case reports of serotonin syndrome occurring with mirtazapine in combination with serotonergic drugs like SSRIs, although such reports are very rare, and do not necessarily implicate mirtazapine as causative.[69][105][106][107]
5-HT3 receptor
It is a potent 5-HT3 blocker. It may relieve chemotherapy-related and advanced cancer-related nausea.[108]
H1 receptor
Mirtazapine is a very strong H1 receptor inverse agonist and, as a result, it can cause powerful sedative and hypnotic effects.[4] A single 15 mg dose of mirtazapine to healthy volunteers has been found to result in over 80% occupancy of the H1 receptor and to induce intense sleepiness.[85] After a short period of chronic treatment, however, the H1 receptor tends to desensitize and the antihistamine effects become more tolerable. Many patients may also dose at night to avoid the effects, and this appears to be an effective strategy for combating them. Blockade of the H1 receptor may improve pre-existing allergies, pruritus, nausea, and insomnia in afflicted individuals. It may also contribute to weight gain, however. In contrast to the H1 receptor, mirtazapine has only low affinity for the muscarinic acetylcholine receptors, although anticholinergic side effects like dry mouth, constipation, and mydriasis are still sometimes seen in clinical practice.[109]
Pharmacokinetics
The oral bioavailability of mirtazapine is about 50%. It is found mostly bound to plasma proteins, about 85%. It is metabolized primarily in the liver by demethylation and hydroxylation via cytochrome P450 enzymes, CYP1A2, CYP2D6, CYP3A4.[110] One of its major metabolites is desmethylmirtazapine. The overall elimination half-life is 20–40 hours. It is conjugated in the kidney for excretion in the urine, where 75% of the drug is excreted,[111] and about 15% is eliminated in feces.[112]: 430
Chemistry
Mirtazapine is a tetracyclic piperazinoazepine; mianserin was developed by the same team of organic chemists and mirtazapine differs from it via addition of a nitrogen atom in one of the rings.[112]: 429 [113][114] It is a racemic mixture of enantiomers. The (S)-(+)-enantiomer is known as esmirtazapine.
Analogues of mirtazapine include mianserin, setiptiline, and aptazapine.
Synthesis
A chemical synthesis of mirtazapine has been published. The first step of synthesis is a condensation reaction between the molecule 2-chloro 3-cyanopyridine and the molecule 1-methyl-3-phenylpiperazine.[115]
History
Mirtazapine was first synthesized at Organon and published in 1989, was first approved for use in major depressive disorder in the Netherlands in 1994, and was introduced in the United States in 1996 under the brand name Remeron.[112]: 429 [116][117]
Society and culture

Generic names
Mirtazapine is the English and French generic name of the drug and its INN, USAN, USP, BAN, DCF, and JAN.[1][2][118] Its generic name in Spanish is mirtazapina and in German is Mirtazapin.[1][2]
Brand names
Mirtazapine is marketed under many brand names worldwide, including Adco-Mirteron, Afloyan, Amirel, Arintapin Smelt, Avanza, Axit, Azapin, Beron, Bilanz, Calixta, Ciblex, Combar, Comenter, Depreram, Divaril, Esprital, Maz, Menelat, Mepirzapine, Merdaten, Meronin, Mi Er Ning, Milivin, Minelza, Minivane, Mirastad, Mirazep, Miro, Miron, Mirrador, Mirt, Mirta, Mirtabene, Mirtadepi, Mirtagamma, Mirtagen, Mirtalan, Mirtamor, Mirtamylan, Mirtan, Mirtaneo, Mirtapax, Mirtapil, Mirtapine, Mirtaron, Mirtastad, Mirtax, Mirtaz, Mirtazap, Mirtazapin, Mirtazapina, Mirtazapine, Mirtazapinum, Mirtazelon, Mirtazon, Mirtazonal, Mirtel, Mirtimash, Mirtin, Mirtine, Mirzapine, Mirzaten, Mirzest, Mitaprex, Mitaxind, Mitocent, Mitrazin, Mizapin, Motofen, Mytra, Norset, Noxibel, Pharmataz, Promyrtil, Rapizapine, Ramure, Razapina, Redepra, Reflex, Remergil, Remergon, Remeron, Remirta, Rexer, Saxib, Sinmaron, Smilon, Tazepin, Tazimed, Tetrazic, Tifona, U-Mirtaron, U-zepine, Valdren, Vastat, Velorin, Yarocen, Zania, Zapex, Zestat, Zismirt, Zispin, Zuleptan, and Zulin.[2]
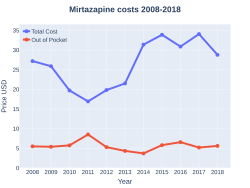
Cost
In the United States the wholesale cost as of 2018 is about US$3 per month.[16] In the United Kingdom a month supply costs the NHS about £1.60 per month as of 2018.[17] In 2017, it was the 119th most commonly prescribed medication in the United States, with more than six million prescriptions.[18][19]
-
Mirtazapine costs (US)
-
Mirtazapine prescriptions (US)
Research
The use of mirtazapine has been explored in several additional conditions:
- Sleep apnea/hypopnea[119][120]
- Inappropriate sexual behaviour and other secondary symptoms of autistic spectrum conditions and other pervasive developmental disorders[121][122][123][124]
- Antipsychotic-induced akathisia.[125][126]
- Drug withdrawal, dependence and detoxification[127]
- Negative, depressive and cognitive symptoms of schizophrenia (as an adjunct)[128][129]
- A case report has been published in which mirtazapine reduced visual hallucinations in a patient with Parkinson's disease psychosis (PDP).[130] This is in alignment with recent findings that inverse agonists at the 5-HT2A receptors are efficacious in attenuating the symptoms of Parkinson's disease psychosis. As is supported by the common practice of prescribing low-dose quetiapine and clozapine for PDP at doses too low to antagonize the D2 receptor, but sufficiently high doses to inversely agonize the 5-HT2A receptors.[27]
- Eight case reports have been reported in five papers on the use of mirtazapine in the treatment of hives as of 2017.[131]
Veterinary use
Mirtazapine also has some veterinary use in cats and dogs. Mirtazapine is sometimes prescribed as an appetite stimulant for cats or dogs experiencing anorexia due to medical conditions such as chronic kidney disease. It is especially useful for treating combined poor appetite and nausea in cats and dogs.[132][133][134]
Mirtazapine is indicated for bodyweight gain in cats experiencing poor appetite and weight loss resulting from chronic medical conditions.[135][136] It is an ointment applied topically to the inner pinna (inner surface of the ear).[135][136]
The most common side effects include signs of local irritation or inflammation at the site where the ointment is applied and behavioural changes (increased meowing, hyperactivity, disoriented state or inability to co-ordinate muscle movements, lack of energy/weakness, attention seeking and aggression).[135][136]
References
- ↑ 1.0 1.1 1.2 Index Nominum 2000: International Drug Directory. Taylor & Francis. 2000. pp. 696–. ISBN 978-3-88763-075-1.
- ↑ 2.0 2.1 2.2 2.3 "Mirtazapine - Drugs.com". Archived from the original on 17 November 2018. Retrieved 26 August 2016.
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 3.13 3.14 3.15 3.16 "Mirtazapine Monograph for Professionals". Drugs.com. American Society of Health-System Pharmacists. Archived from the original on 10 January 2021. Retrieved 20 November 2018.
- ↑ 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 4.10 4.11 4.12 4.13 4.14 4.15 4.16 4.17 4.18 4.19 4.20 4.21 4.22 4.23 4.24 4.25 4.26 4.27 4.28 4.29 Anttila SA, Leinonen EV (2001). "A review of the pharmacological and clinical profile of mirtazapine". CNS Drug Rev. 7 (3): 249–64. doi:10.1111/j.1527-3458.2001.tb00198.x. PMC 6494141. PMID 11607047.
- ↑ 5.0 5.1 "Mirtazapine Use During Pregnancy". Drugs.com. 23 September 2019. Archived from the original on 22 August 2020. Retrieved 4 March 2020.
- ↑ 6.0 6.1 "WHOCC - ATC/DDD Index". www.whocc.no. Archived from the original on 20 September 2020. Retrieved 9 September 2020.
- ↑ 7.0 7.1 7.2 7.3 7.4 7.5 7.6 7.7 7.8 Timmer CJ, Sitsen JM, Delbressine LP (June 2000). "Clinical pharmacokinetics of mirtazapine". Clinical Pharmacokinetics. 38 (6): 461–74. doi:10.2165/00003088-200038060-00001. PMID 10885584.
- ↑ 8.0 8.1 8.2 8.3 8.4 8.5 "REMERON (mirtazapine) tablet, film coated [Organon Pharmaceuticals USA]". DailyMed. Organon Pharmaceuticals USA. October 2012. Archived from the original on 10 January 2021. Retrieved 24 October 2013.
- ↑ 9.0 9.1 9.2 9.3 9.4 9.5 9.6 "Axit Mirtazapine PRODUCT INFORMATION". TGA eBusiness Services. alphapharm. 25 October 2011. Archived from the original on 20 September 2020. Retrieved 15 October 2013.
- ↑ 10.0 10.1 10.2 10.3 10.4 10.5 10.6 "Mirtazapine 30 mg Tablets – Summary of Product Characteristics". electronic Medicines Compendium. Sandoz Limited. 20 March 2013. Archived from the original (PDF) on 31 July 2017. Retrieved 24 October 2013.
- ↑ 11.0 11.1 11.2 11.3 Watanabe N, Omori IM, Nakagawa A, Cipriani A, Barbui C, Churchill R, Furukawa TA (December 2011). "Mirtazapine versus other antidepressive agents for depression". The Cochrane Database of Systematic Reviews (12): CD006528. doi:10.1002/14651858.CD006528.pub2. PMC 4158430. PMID 22161405.
- ↑ 12.0 12.1 Nutt DJ (2002). "Tolerability and safety aspects of mirtazapine". Hum Psychopharmacol. 17 Suppl 1: S37–41. doi:10.1002/hup.388. PMID 12404669.
- ↑ 13.0 13.1 "[129] Mirtazapine: Update on efficacy, safety, dose response". www.ti.ubc.ca. Archived from the original on 7 May 2021. Retrieved 8 May 2021.
- ↑ British national formulary : BNF 74 (74 ed.). British Medical Association. 2017. p. 354. ISBN 978-0857112989.
- ↑ Schatzberg AF, Cole JO, DeBattista C (2010). "3". Manual of Clinical Psychopharmacology (7th ed.). Arlington, VA: American Psychiatric Publishing. ISBN 978-1-58562-377-8.
- ↑ 16.0 16.1 "NADAC as of 2018-11-21". Centers for Medicare and Medicaid Services. Archived from the original on 1 June 2019. Retrieved 21 November 2018.
- ↑ 17.0 17.1 British national formulary : BNF 76 (76 ed.). Pharmaceutical Press. 2018. p. 369. ISBN 9780857113382.
- ↑ 18.0 18.1 "The Top 300 of 2020". ClinCalc. Archived from the original on 12 February 2021. Retrieved 11 April 2020.
- ↑ 19.0 19.1 "Mirtazapine - Drug Usage Statistics". ClinCalc. Archived from the original on 20 October 2020. Retrieved 11 April 2020.
- ↑ 20.0 20.1 Gorman JM (1999). "Mirtazapine: clinical overview". The Journal of Clinical Psychiatry. 60 Suppl 17: 9–13, discussion 46–8. PMID 10446735.
- ↑ Benjamin S, Doraiswamy PM (July 2011). "Review of the use of mirtazapine in the treatment of depression". Expert Opinion on Pharmacotherapy. 12 (10): 1623–32. doi:10.1517/14656566.2011.585459. PMID 21644844.
- ↑ 22.0 22.1 Thompson C (June 2002). "Onset of action of antidepressants: results of different analyses". Human Psychopharmacology. 17 Suppl 1: S27–32. doi:10.1002/hup.386. PMID 12404667.
- ↑ Pharmacological Interventions: 10.14. Clinical Practice Recommendations. National Collaborating Centre for Mental Health/British Psychological Society. 2010. Archived from the original on 6 September 2020. Retrieved 4 July 2017.
- ↑ Pharmacological Interventions: Third-Generation Antidepressants: 10.8.3. Mirtazapine. National Collaborating Centre for Mental Health/British Psychological Society. 2010. Archived from the original on 6 September 2020. Retrieved 4 July 2017.
- ↑ Wichniak A, Wierzbicka A, Jernajczyk W (2012). "Sleep and antidepressant treatment". Current Pharmaceutical Design. 18 (36): 5802–17. doi:10.2174/138161212803523608. PMID 22681161.
- ↑ 26.0 26.1 Cipriani A, Furukawa TA, Salanti G, Chaimani A, Atkinson LZ, Ogawa Y, Leucht S, Ruhe HG, Turner EH, Higgins JP, Egger M, Takeshima N, Hayasaka Y, Imai H, Shinohara K, Tajika A, Ioannidis JP, Geddes JR (April 2018). "Comparative efficacy and acceptability of 21 antidepressant drugs for the acute treatment of adults with major depressive disorder: a systematic review and network meta-analysis". Lancet. 391 (10128): 1357–1366. doi:10.1016/S0140-6736(17)32802-7. PMC 5889788. PMID 29477251.
- ↑ 27.0 27.1 27.2 Taylor D, Paton C, Shitij K (2012). Maudsley Prescribing Guidelines in Psychiatry (11th ed.). West Sussex: Wiley-Blackwell. ISBN 978-0-47-097948-8.
- ↑ Goodnick PJ, Puig A, DeVane CL, Freund BV (July 1999). "Mirtazapine in major depression with comorbid generalized anxiety disorder". The Journal of Clinical Psychiatry. 60 (7): 446–8. doi:10.4088/JCP.v60n0705. PMID 10453798.
- ↑ 29.0 29.1 29.2 29.3 Croom KF, Perry CM, Plosker GL (2009). "Mirtazapine: a review of its use in major depression and other psychiatric disorders". CNS Drugs. 23 (5): 427–52. doi:10.2165/00023210-200923050-00006. PMID 19453203.
- ↑ Landowski J (2002). "[Mirtazapine—an antidepressant]". Psychiatria Polska (in Polish). 36 (6 Suppl): 125–30. PMID 12647431.
{{cite journal}}: CS1 maint: unrecognized language (link) - ↑ Chinuck RS, Fortnum H, Baldwin DR (December 2007). "Appetite stimulants in cystic fibrosis: a systematic review". Journal of Human Nutrition and Dietetics. 20 (6): 526–37. doi:10.1111/j.1365-277X.2007.00824.x. PMID 18001374. Archived from the original on 28 August 2021. Retrieved 22 November 2019.
- ↑ Davis MP, Khawam E, Pozuelo L, Lagman R (August 2002). "Management of symptoms associated with advanced cancer: olanzapine and mirtazapine. A World Health Organization project". Expert Review of Anticancer Therapy. 2 (4): 365–76. doi:10.1586/14737140.2.4.365. PMID 12647979.
- ↑ Clark MS, Smith PO, Jamieson B (November 2011). "FPIN's clinical inquiries: Antidepressants for the treatment of insomnia in patients with depression" (PDF). American Family Physician. 84 (9): 1–2. PMID 22164891. Archived (PDF) from the original on 9 July 2020. Retrieved 11 July 2017.
- ↑ "The Effects of Antidepressants on Sleep | Psychiatric Times". www.psychiatrictimes.com. Archived from the original on 10 June 2020. Retrieved 11 July 2017.
- ↑ 35.0 35.1 Li TC, Shiah IS, Sun CJ, Tzang RF, Huang KC, Lee WK (June 2011). "Mirtazapine relieves post-electroconvulsive therapy headaches and nausea: a case series and review of the literature". The Journal of ECT. 27 (2): 165–7. doi:10.1097/YCT.0b013e3181e63346. PMID 21602639.
- ↑ 36.0 36.1 Kast RE, Foley KF (July 2007). "Cancer chemotherapy and cachexia: mirtazapine and olanzapine are 5-HT3 antagonists with good antinausea effects". European Journal of Cancer Care. 16 (4): 351–4. doi:10.1111/j.1365-2354.2006.00760.x. PMID 17587360.
- ↑ Twycross R, Greaves MW, Handwerker H, Jones EA, Libretto SE, Szepietowski JC, Zylicz Z (January 2003). "Itch: scratching more than the surface". QJM. 96 (1): 7–26. doi:10.1093/qjmed/hcg002. PMID 12509645. Archived from the original on 14 January 2021. Retrieved 13 May 2012.
- ↑ Greaves MW (2005). "Itch in systemic disease: therapeutic options". Dermatologic Therapy. 18 (4): 323–7. doi:10.1111/j.1529-8019.2005.00036.x. PMID 16297004.
- ↑ Colombo B, Annovazzi PO, Comi G (October 2004). "Therapy of primary headaches: the role of antidepressants". Neurological Sciences. 25 Suppl 3: S171–5. doi:10.1007/s10072-004-0280-x. PMID 15549531.
- ↑ Tajti J, Almási J (June 2006). "Effects of mirtazapine in patients with chronic tension-type headache. Literature review". Neuropsychopharmacologia Hungarica (in Hungarian). 8 (2): 67–72. PMID 17073214.
{{cite journal}}: CS1 maint: unrecognized language (link) - ↑ "mirtazapine (Rx) – Remeron, Remeron SolTab". Medscape. WebMD. Archived from the original on 29 October 2013. Retrieved 24 October 2013.
- ↑ "Australian Medicines Handbook". Australian Medicines Handbook Pty Ltd. 2013. Archived from the original on 27 September 2011. Retrieved 14 March 2022.
- ↑ British National Formulary (BNF) (65th ed.). Pharmaceutical Press. 2013. p. 1120. ISBN 978-0857110848.
- ↑ "Remeron (Mirtazapine) Drug Information". RxList. Archived from the original on 4 May 2017. Retrieved 28 March 2016.
- ↑ Hummel J, Westphal S, Weber-Hamann B, Gilles M, Lederbogen F, Angermeier T, Luley C, Deuschle M, Kopf D (July 2011). "Serum lipoproteins improve after successful pharmacologic antidepressant treatment: a randomized open-label prospective trial". The Journal of Clinical Psychiatry. 72 (7): 885–91. doi:10.4088/JCP.09m05853blu. PMID 21294998.
- ↑ McIntyre RS, Soczynska JK, Konarski JZ, Kennedy SH (July 2006). "The effect of antidepressants on lipid homeostasis: a cardiac safety concern?". Expert Opinion on Drug Safety. 5 (4): 523–37. doi:10.1517/14740338.5.4.523. PMID 16774491.
- ↑ 47.0 47.1 47.2 47.3 47.4 47.5 Fawcett J, Barkin RL (December 1998). "Review of the results from clinical studies on the efficacy, safety and tolerability of mirtazapine for the treatment of patients with major depression". Journal of Affective Disorders. 51 (3): 267–85. doi:10.1016/S0165-0327(98)00224-9. PMID 10333982.
- ↑ Möller HJ (December 2006). "Is there evidence for negative effects of antidepressants on suicidality in depressive patients? A systematic review". European Archives of Psychiatry and Clinical Neuroscience. 256 (8): 476–96. doi:10.1007/s00406-006-0689-8. PMID 17143567.
- ↑ Abo-Zena RA, Bobek MB, Dweik RA (April 2000). "Hypertensive urgency induced by an interaction of mirtazapine and clonidine". Pharmacotherapy. 20 (4): 476–8. doi:10.1592/phco.20.5.476.35061. PMID 10772378.
- ↑ 50.0 50.1 Benazzi F (June 1998). "Mirtazapine withdrawal symptoms". Canadian Journal of Psychiatry. 43 (5): 525. PMID 9653542.[unreliable medical source?]
- ↑ Blier P (2001). "Pharmacology of rapid-onset antidepressant treatment strategies". The Journal of Clinical Psychiatry. 62 Suppl 15: 12–7. PMID 11444761.
- ↑ Vlaminck JJ, van Vliet IM, Zitman FG (March 2005). "[Withdrawal symptoms of antidepressants]". Nederlands Tijdschrift voor Geneeskunde (in Nederlands). 149 (13): 698–701. PMID 15819135.
- ↑ Berigan TR (June 2001). "Mirtazapine-Associated Withdrawal Symptoms: A Case Report". Primary Care Companion to the Journal of Clinical Psychiatry. 3 (3): 143. doi:10.4088/PCC.v03n0307a. PMC 181176. PMID 15014614.[unreliable medical source?]
- ↑ Klesmer J, Sarcevic A, Fomari V (August 2000). "Panic attacks during discontinuation of mirtazepine". Canadian Journal of Psychiatry. 45 (6): 570–1. PMID 10986577.[unreliable medical source?]
- ↑ MacCall C, Callender J (October 1999). "Mirtazapine withdrawal causing hypomania". The British Journal of Psychiatry. 175 (4): 390. doi:10.1192/bjp.175.4.390a. PMID 10789310.[unreliable medical source?]
- ↑ Ali S, Milev R (May 2003). "Switch to mania upon discontinuation of antidepressants in patients with mood disorders: a review of the literature". Canadian Journal of Psychiatry. 48 (4): 258–64. doi:10.1177/070674370304800410. PMID 12776393.
- ↑ White N, Litovitz T, Clancy C (December 2008). "Suicidal antidepressant overdoses: a comparative analysis by antidepressant type". Journal of Medical Toxicology. 4 (4): 238–50. doi:10.1007/bf03161207. PMC 3550116. PMID 19031375.
- ↑ Holzbach R, Jahn H, Pajonk FG, Mähne C (November 1998). "Suicide attempts with mirtazapine overdose without complications". Biological Psychiatry. 44 (9): 925–6. doi:10.1016/S0006-3223(98)00081-X. PMID 9807651.[unreliable medical source?]
- ↑ Retz W, Maier S, Maris F, Rösler M (November 1998). "Non-fatal mirtazapine overdose". International Clinical Psychopharmacology. 13 (6): 277–9. doi:10.1097/00004850-199811000-00007. PMID 9861579.[unreliable medical source?]
- ↑ Nikolaou P, Dona A, Papoutsis I, Spiliopoulou C, Maravelias C. "Death Due to Mirtazapine Overdose".
{{cite journal}}: Cite journal requires|journal=(help) in "Abstracts of the XXIX International Congress of the European Association of Poison Centres and Clinical Toxicologists, May 12–15, 2009, Stockholm, Sweden". Clinical Toxicology. 47 (5): 436–510. 2009. doi:10.1080/15563650902952273. - ↑ Baselt, RC (2008). Disposition of Toxic Drugs and Chemicals in Man (8th ed.). Foster City, CA: Biomedical Publications. pp. 1045–7. ISBN 978-0-9626523-7-0.
- ↑ Buckley NA, McManus PR (December 2002). "Fatal toxicity of serotoninergic and other antidepressant drugs: analysis of United Kingdom mortality data". BMJ. 325 (7376): 1332–3. doi:10.1136/bmj.325.7376.1332. PMC 137809. PMID 12468481.[unreliable medical source?]
- ↑ Stahl SM (2008). Stahl's Essential Psychopharmacology Online: Print and Online. Cambridge, UK: Cambridge University Press. ISBN 978-0-521-74609-0. Archived from the original on 19 June 2020. Retrieved 21 January 2012.
- ↑ Silva J, Mota J, Azevedo P (March 2016). "California rocket fuel: And what about being a first line treatment?". European Psychiatry. 33: S551. doi:10.1016/j.eurpsy.2016.01.2033.
- ↑ Wu, Chi-Shun; Tong, Show-Hwa; Ong, Cheung-Ter; Sung, Sheng-Feng (December 2015). "Serotonin Syndrome Induced by Combined Use of Mirtazapine and Olanzapine Complicated with Rhabdomyolysis, Acute Renal Failure, and Acute Pulmonary Edema-A Case Report". Acta Neurologica Taiwanica. 24 (4): 117–121. ISSN 1028-768X. PMID 27333965.
- ↑ Saguin, Emeric; Keou, S.; Ratnam, C.; Mennessier, C.; Delacour, H.; Lahutte, B. (May 2018). "Severe rhabdomyolysis induced by quetiapine and mirtazapine in a French military soldier". Journal of the Royal Army Medical Corps. 164 (2): 127–129. doi:10.1136/jramc-2018-000939. ISSN 0035-8665. PMID 29632134.
- ↑ Houlihan, David J. (March 2004). "Serotonin syndrome resulting from coadministration of tramadol, venlafaxine, and mirtazapine". The Annals of Pharmacotherapy. 38 (3): 411–413. doi:10.1345/aph.1D344. ISSN 1060-0280. PMID 14970364.
- ↑ 68.0 68.1 68.2 68.3 68.4 Gillman PK (June 2006). "A review of serotonin toxicity data: implications for the mechanisms of antidepressant drug action". Biological Psychiatry. 59 (11): 1046–51. doi:10.1016/j.biopsych.2005.11.016. PMID 16460699.
- ↑ 69.0 69.1 69.2 69.3 69.4 69.5 69.6 Gillman PK (2006). "A systematic review of the serotonergic effects of mirtazapine in humans: implications for its dual action status". Hum Psychopharmacol. 21 (2): 117–25. doi:10.1002/hup.750. PMID 16342227.
- ↑ Iqbal MM, Basil MJ, Kaplan J, Iqbal MT (2012). "Overview of serotonin syndrome". Ann Clin Psychiatry. 24 (4): 310–8. PMID 23145389.
- ↑ Roth, BL; Driscol, J. "PDSP Ki Database". Psychoactive Drug Screening Program (PDSP). University of North Carolina at Chapel Hill and the United States National Institute of Mental Health. Archived from the original on 28 August 2021. Retrieved 14 August 2017.
- ↑ 72.0 72.1 72.2 Tatsumi M, Groshan K, Blakely RD, Richelson E (1997). "Pharmacological profile of antidepressants and related compounds at human monoamine transporters". Eur. J. Pharmacol. 340 (2–3): 249–58. doi:10.1016/s0014-2999(97)01393-9. PMID 9537821.
- ↑ 73.00 73.01 73.02 73.03 73.04 73.05 73.06 73.07 73.08 73.09 73.10 73.11 73.12 73.13 73.14 73.15 73.16 73.17 73.18 73.19 73.20 73.21 73.22 73.23 73.24 73.25 Van der Mey M, Windhorst AD, Klok RP, Herscheid JD, Kennis LE, Bischoff F, Bakker M, Langlois X, Heylen L, Jurzak M, Leysen JE (2006). "Synthesis and biodistribution of [11C]R107474, a new radiolabeled alpha2-adrenoceptor antagonist". Bioorg. Med. Chem. 14 (13): 4526–34. doi:10.1016/j.bmc.2006.02.029. PMID 16517171.
- ↑ 74.0 74.1 74.2 Gillman PK (2007). "Tricyclic antidepressant pharmacology and therapeutic drug interactions updated". Br. J. Pharmacol. 151 (6): 737–48. doi:10.1038/sj.bjp.0707253. PMC 2014120. PMID 17471183.
- ↑ Anttila, Sami A. K.; Leinonen, Esa V. J. (2001). "A Review of the Pharmacological and Clinical Profile of Mirtazapine". CNS Drug Reviews. 7 (3): 249–264. doi:10.1111/j.1527-3458.2001.tb00198.x. ISSN 1527-3458. PMC 6494141. PMID 11607047. Archived from the original on 7 May 2021. Retrieved 14 May 2020.
- ↑ 76.0 76.1 76.2 76.3 Appl H, Holzammer T, Dove S, Haen E, Strasser A, Seifert R (2012). "Interactions of recombinant human histamine H₁R, H₂R, H₃R, and H₄R receptors with 34 antidepressants and antipsychotics". Naunyn Schmiedebergs Arch. Pharmacol. 385 (2): 145–70. doi:10.1007/s00210-011-0704-0. PMID 22033803.
- ↑ de Boer TH, Maura G, Raiteri M, de Vos CJ, Wieringa J, Pinder RM (April 1988). "Neurochemical and autonomic pharmacological profiles of the 6-aza-analogue of mianserin, Org 3770 and its enantiomers". Neuropharmacology. 27 (4): 399–408. doi:10.1016/0028-3908(88)90149-9. PMID 3419539.
- ↑ "Mirtazapine". Drugbank. Archived from the original on 19 August 2020. Retrieved 16 January 2020.
- ↑ 79.0 79.1 79.2 79.3 Frazer A (1997). "Pharmacology of antidepressants". J Clin Psychopharmacol. 17 Suppl 1: 2S–18S. doi:10.1097/00004714-199704001-00002. PMID 9090573.
- ↑ Fisar Z, Hroudová J, Raboch J (2010). "Inhibition of monoamine oxidase activity by antidepressants and mood stabilizers". Neuro Endocrinology Letters. 31 (5): 645–56. PMID 21200377.
- ↑ Richelson E (2001). "Pharmacology of antidepressants". Mayo Clin. Proc. 76 (5): 511–27. doi:10.4065/76.5.511. PMID 11357798.
- ↑ Laurence Brunton; Bruce A. Chabner; Bjorn Knollman (14 January 2011). Goodman and Gilman's The Pharmacological Basis of Therapeutics, Twelfth Edition. McGraw Hill Professional. p. 410. ISBN 978-0-07-176939-6. Archived from the original on 14 January 2021. Retrieved 14 August 2017.
- ↑ Alan F. Schatzberg; Charles B. Nemeroff (10 May 2017). The American Psychiatric Association Publishing Textbook of Psychopharmacology. American Psychiatric Pub. pp. 322–. ISBN 978-1-61537-122-8. Archived from the original on 14 January 2021. Retrieved 14 August 2017.
- ↑ 84.0 84.1 84.2 Brayfield, A, ed. (30 January 2013). Mirtazapine. Martindale: The Complete Drug Reference. The Royal Pharmaceutical Society of Great Britain. Archived from the original on 14 January 2021. Retrieved 3 November 2013.
- ↑ 85.0 85.1 Sato H, Ito C, Tashiro M, Hiraoka K, Shibuya K, Funaki Y, Iwata R, Matsuoka H, Yanai K (2013). "Histamine H₁ receptor occupancy by the new-generation antidepressants fluvoxamine and mirtazapine: a positron emission tomography study in healthy volunteers". Psychopharmacology. 230 (2): 227–34. doi:10.1007/s00213-013-3146-1. PMID 23728612.
- ↑ Olianas MC, Dedoni S, Onali P (November 2012). "The atypical antidepressant mianserin exhibits agonist activity at κ-opioid receptors". British Journal of Pharmacology. 167 (6): 1329–41. doi:10.1111/j.1476-5381.2012.02078.x. PMC 3504997. PMID 22708686.
- ↑ De Boer T, Nefkens F, Van Helvoirt A (February 1994). "The alpha 2-adrenoceptor antagonist Org 3770 enhances serotonin transmission in vivo". European Journal of Pharmacology. 253 (1–2): R5–6. doi:10.1016/0014-2999(94)90778-1. PMID 7912194.[unreliable medical source?]
- ↑ 88.0 88.1 Berendsen HH, Broekkamp CL (October 1997). "Indirect in vivo 5-HT1A-agonistic effects of the new antidepressant mirtazapine". Psychopharmacology. 133 (3): 275–82. doi:10.1007/s002130050402. PMID 9361334.
- ↑ Nakayama K, Sakurai T, Katsu H (April 2004). "Mirtazapine increases dopamine release in prefrontal cortex by 5-HT1A receptor activation". Brain Research Bulletin. 63 (3): 237–41. doi:10.1016/j.brainresbull.2004.02.007. PMID 15145142.[unreliable medical source?]
- ↑ Blier P, Abbott FV (January 2001). "Putative mechanisms of action of antidepressant drugs in affective and anxiety disorders and pain" (PDF). Journal of Psychiatry & Neuroscience. 26 (1): 37–43. PMC 1408043. PMID 11212592. Archived from the original (PDF) on 6 March 2016. Retrieved 20 June 2009.
- ↑ Millan MJ (2005). "Serotonin 5-HT2C receptors as a target for the treatment of depressive and anxious states: focus on novel therapeutic strategies". Thérapie. 60 (5): 441–60. doi:10.2515/therapie:2005065. PMID 16433010.
- ↑ Dekeyne A, Millan MJ (April 2009). "Discriminative stimulus properties of the atypical antidepressant, mirtazapine, in rats: a pharmacological characterization". Psychopharmacology. 203 (2): 329–41. doi:10.1007/s00213-008-1259-8. PMID 18709360.
- ↑ "Mirtazapine increases dopamine release in prefrontal cortex by 5-HT1A receptor activation" (PDF). Archived from the original (PDF) on 9 January 2018. Retrieved 8 January 2018.
- ↑ Millan MJ, Gobert A, Rivet JM, et al. (March 2000). "Mirtazapine enhances frontocortical dopaminergic and corticolimbic adrenergic, but not serotonergic, transmission by blockade of α2-adrenergic and serotonin2C receptors: a comparison with citalopram". Eur. J. Neurosci. 12 (3): 1079–95. doi:10.1046/j.1460-9568.2000.00982.x. PMID 10762339.
- ↑ Millan MJ, Gobert A, Rivet JM, Adhumeau-Auclair A, Cussac D, Newman-Tancredi A, Dekeyne A, Nicolas JP, Lejeune F (March 2000). "Mirtazapine enhances frontocortical dopaminergic and corticolimbic adrenergic, but not serotonergic, transmission by blockade of alpha2-adrenergic and serotonin2C receptors: a comparison with citalopram". The European Journal of Neuroscience. 12 (3): 1079–95. doi:10.1046/j.1460-9568.2000.00982.x. PMID 10762339.
- ↑ 96.0 96.1 Graves SM, Napier TC (June 2012). "SB 206553, a putative 5-HT2C inverse agonist, attenuates methamphetamine-seeking in rats". BMC Neuroscience. 13 (1): 65. doi:10.1186/1471-2202-13-65. PMC 3441362. PMID 22697313.
- ↑ 97.0 97.1 Colfax GN, Santos GM, Das M, Santos DM, Matheson T, Gasper J, Shoptaw S, Vittinghoff E (November 2011). "Mirtazapine to reduce methamphetamine use: a randomized controlled trial". Archives of General Psychiatry. 68 (11): 1168–75. doi:10.1001/archgenpsychiatry.2011.124. PMC 3437988. PMID 22065532.
- ↑ Herrold AA, Shen F, Graham MP, Harper LK, Specio SE, Tedford CE, Napier TC (January 2009). "Mirtazapine treatment after conditioning with methamphetamine alters subsequent expression of place preference". Drug and Alcohol Dependence. 99 (1–3): 231–9. doi:10.1016/j.drugalcdep.2008.08.005. PMID 18945553.
- ↑ 99.0 99.1 Rose ME, Grant JE (2008). "Pharmacotherapy for methamphetamine dependence: a review of the pathophysiology of methamphetamine addiction and the theoretical basis and efficacy of pharmacotherapeutic interventions". Annals of Clinical Psychiatry. 20 (3): 145–55. doi:10.1080/10401230802177656. PMID 18633741.
- ↑ 100.0 100.1 Brackins T, Brahm NC, Kissack JC (December 2011). "Treatments for methamphetamine abuse: a literature review for the clinician". Journal of Pharmacy Practice. 24 (6): 541–50. doi:10.1177/0897190011426557. PMID 22095579.
- ↑ 101.0 101.1 Brensilver M, Heinzerling KG, Shoptaw S (September 2013). "Pharmacotherapy of amphetamine-type stimulant dependence: an update". Drug and Alcohol Review. 32 (5): 449–60. doi:10.1111/dar.12048. PMC 4251965. PMID 23617468.
- ↑ Kast RE (September 2001). "Mirtazapine may be useful in treating nausea and insomnia of cancer chemotherapy". Supportive Care in Cancer. 9 (6): 469–70. doi:10.1007/s005200000215. PMID 11585276.
- ↑ Caldis EV, Gair RD (October 2004). "Mirtazapine for treatment of nausea induced by selective serotonin reuptake inhibitors". Canadian Journal of Psychiatry. 49 (10): 707. doi:10.1177/070674370404901014. PMID 15560319.
- ↑ Berling I, Isbister GK (2014). "Mirtazapine overdose is unlikely to cause major toxicity". Clin Toxicol. 52 (1): 20–4. doi:10.3109/15563650.2013.859264. PMC 3894718. PMID 24228948.
- ↑ Freijo Guerrero J, Tardón Ruiz de Gauna L, Gómez JJ, Aguilera Celorrio L (2009). "[Serotonin syndrome after administration of mirtazapine in a critical care unit]". Rev Esp Anestesiol Reanim (in Spanish). 56 (8): 515–6. doi:10.1016/s0034-9356(09)70444-x. PMID 19994622.
{{cite journal}}: CS1 maint: unrecognized language (link) - ↑ Butler MC, Di Battista M, Warden M (2010). "Sertraline-induced serotonin syndrome followed by mirtazapine reaction". Prog. Neuropsychopharmacol. Biol. Psychiatry. 34 (6): 1128–9. doi:10.1016/j.pnpbp.2010.04.015. PMID 20430060.
- ↑ Decoutere L, De Winter S, Vander Weyden L, Spriet I, Schrooten M, Tournoy J, Fagard K (2012). "A venlafaxine and mirtazapine-induced serotonin syndrome confirmed by de- and re-challenge". Int J Clin Pharm. 34 (5): 686–8. doi:10.1007/s11096-012-9666-7. PMID 22752315.
- ↑ Kast, R.E.; Foley, K.F. (July 2007). "Cancer chemotherapy and cachexia: mirtazapine and olanzapine are 5-HT3 antagonists with good antinausea effects". European Journal of Cancer Care. 16 (4): 351–354. doi:10.1111/j.1365-2354.2006.00760.x. ISSN 0961-5423. PMID 17587360. Archived from the original on 28 August 2021. Retrieved 14 May 2020.
- ↑ Burrows GD, Kremer CM (April 1997). "Mirtazapine: clinical advantages in the treatment of depression". Journal of Clinical Psychopharmacology. 17 Suppl 1: 34S–39S. doi:10.1097/00004714-199704001-00005. PMID 9090576.
- ↑ Anttila, SA; Leinonen, EV (2001). "A review of the pharmacological and clinical profile of mirtazapine". CNS Drug Reviews. 7 (3): 249–64. doi:10.1111/j.1527-3458.2001.tb00198.x. PMC 6494141. PMID 11607047.
- ↑ Al-Majed, Abdulrahman; Bakheit, Ahmed H.; Alharbi, Raed M.; Abdel Aziz, Hatem A. (1 January 2018). Chapter Two - Mirtazapine. Profiles of Drug Substances, Excipients and Related Methodology. Vol. 43. pp. 209–254. doi:10.1016/bs.podrm.2018.01.002. ISBN 9780128151259. PMID 29678261.
- ↑ 112.0 112.1 112.2 Schatzberg, Alan F. (2009). "Chapter 21: Mirtazapine". In Schatzberg, Alan F.; Nemeroff, Charles B. (eds.). The American Psychiatric Publishing Textbook of Psychopharmacology (4th ed.). Washington, D.C.: American Psychiatric Pub. ISBN 9781585623099.
- ↑ "Mirtazapine label – Australia". GuildLink, a wholly owned subsidiary company of the Pharmacy Guild of Australia. 27 May 2016. Archived from the original on 21 November 2018. Retrieved 22 July 2017.
- ↑ Kelder, J; Funke, C; De Boer, T; Delbressine, L; Leysen, D; Nickolson, V (April 1997). "A comparison of the physicochemical and biological properties of mirtazapine and mianserin". The Journal of Pharmacy and Pharmacology. 49 (4): 403–11. doi:10.1111/j.2042-7158.1997.tb06814.x. PMID 9232538.
- ↑ Srinivasa Rao, D. V. N; Dandala, R; Handa, V. K; Sivakumaran, M; Raghava Reddy, A. V; Naidu, A (2007). "Improved Synthesis of Mirtazapine". Organic Preparations and Procedures International. 39 (4): 399. doi:10.1080/00304940709458595.
- ↑ Kaspersen, Frans M.; Van Rooij, Fons A. M.; Sperling, Eric G. M.; Wieringa, Joop H. (September 1989). "The synthesis of org 3770 labelled with 3H, 13C AND 14C". Journal of Labelled Compounds and Radiopharmaceuticals. 27 (9): 1055–1068. doi:10.1002/jlcr.2580270911.
- ↑ "Remeron New FDA Drug Approvalh". Centerwatch. Archived from the original on 5 August 2019. Retrieved 26 August 2016.
- ↑ I.K. Morton; Judith M. Hall (6 December 2012). Concise Dictionary of Pharmacological Agents: Properties and Synonyms. Springer Science & Business Media. p. 183. ISBN 978-94-011-4439-1. Archived from the original on 28 April 2021. Retrieved 14 August 2017.
- ↑ Kohler M, Bloch KE, Stradling JR (May 2009). "Pharmacological approaches to the treatment of obstructive sleep apnoea" (PDF). Expert Opinion on Investigational Drugs. 18 (5): 647–56. doi:10.1517/13543780902877674. PMID 19388881. Archived (PDF) from the original on 24 September 2017. Retrieved 14 November 2018.
- ↑ Marshall NS, Yee BJ, Desai AV, Buchanan PR, Wong KK, Crompton R, Melehan KL, Zack N, Rao SG, Gendreau RM, Kranzler J, Grunstein RR (June 2008). "Two randomized placebo-controlled trials to evaluate the efficacy and tolerability of mirtazapine for the treatment of obstructive sleep apnea". Sleep. 31 (6): 824–31. doi:10.1093/sleep/31.6.824. PMC 2442407. PMID 18548827.
- ↑ Masi G (2004). "Pharmacotherapy of pervasive developmental disorders in children and adolescents". CNS Drugs. 18 (14): 1031–52. doi:10.2165/00023210-200418140-00006. PMID 15584771.
- ↑ Marek GJ, Carpenter LL, McDougle CJ, Price LH (February 2003). "Synergistic action of 5-HT2A antagonists and selective serotonin reuptake inhibitors in neuropsychiatric disorders". Neuropsychopharmacology. 28 (2): 402–12. doi:10.1038/sj.npp.1300057. PMID 12589395.
- ↑ Posey DJ, Guenin KD, Kohn AE, Swiezy NB, McDougle CJ (2001). "A naturalistic open-label study of mirtazapine in autistic and other pervasive developmental disorders". Journal of Child and Adolescent Psychopharmacology. 11 (3): 267–77. doi:10.1089/10445460152595586. PMID 11642476.
- ↑ Coskun M, Karakoc S, Kircelli F, Mukaddes NM (April 2009). "Effectiveness of mirtazapine in the treatment of inappropriate sexual behaviors in individuals with autistic disorder". Journal of Child and Adolescent Psychopharmacology. 19 (2): 203–6. doi:10.1089/cap.2008.020. PMID 19364298.
- ↑ Kumar R, Sachdev PS (May 2009). "Akathisia and second-generation antipsychotic drugs". Current Opinion in Psychiatry. 22 (3): 293–99. doi:10.1097/YCO.0b013e32832a16da. PMID 19378382.
- ↑ Hieber R, Dellenbaugh T, Nelson LA (June 2008). "Role of mirtazapine in the treatment of antipsychotic-induced akathisia". The Annals of Pharmacotherapy. 42 (6): 841–6. doi:10.1345/aph.1K672. PMID 18460588.
- ↑ Graves SM, Rafeyan R, Watts J, Napier TC (December 2012). "Mirtazapine, and mirtazapine-like compounds as possible pharmacotherapy for substance abuse disorders: evidence from the bench and the bedside". Pharmacology & Therapeutics. 136 (3): 343–53. doi:10.1016/j.pharmthera.2012.08.013. PMC 3483434. PMID 22960395.
- ↑ Ritsner, MS (2013). Ritsner, Michael S (ed.). Polypharmacy in Psychiatry Practice, Volume I. Springer Science+Business Media Dordrecht. doi:10.1007/978-94-007-5805-6. ISBN 9789400758056.
- ↑ Vidal C, Reese C, Fischer BA, Chiapelli J, Himelhoch S (July 2015). "Meta-Analysis of Efficacy of Mirtazapine as an Adjunctive Treatment of Negative Symptoms in Schizophrenia". Clinical Schizophrenia & Related Psychoses. 9 (2): 88–95. doi:10.3371/CSRP.VIRE.030813. PMID 23491969.
- ↑ Tagai K, Nagata T, Shinagawa S, Tsuno N, Ozone M, Nakayama K (June 2013). "Mirtazapine improves visual hallucinations in Parkinson's disease: a case report". Psychogeriatrics. 13 (2): 103–7. doi:10.1111/j.1479-8301.2012.00432.x. PMID 23909968.
- ↑ Eskeland, Shirin; Halvorsen, Jon Anders; Tanum, Lars (17 May 2017). "Antidepressants have Anti-inflammatory Effects that may be Relevant to Dermatology: A Systematic Review" (PDF). Acta Dermato-Venereologica. 97 (8): 897–905. doi:10.2340/00015555-2702. ISSN 1651-2057. PMID 28512664. Archived (PDF) from the original on 11 March 2020. Retrieved 5 September 2019.
- ↑ "Remeron for Cats". Archived from the original on 26 June 2015. Retrieved 12 January 2013.
- ↑ Roger Gfeller, D. V. M.; Michael Thomas, D. V. M.; Mayo, Isaac (8 August 2017). "Mirtazapine (Remeron)". Vin.com. Archived from the original on 6 December 2010. Retrieved 12 January 2013.
- ↑ Agnew, W; Korman, R (September 2014). "Pharmacological appetite stimulation: rational choices in the inappetent cat". Journal of Feline Medicine and Surgery. 16 (9): 749–56. doi:10.1177/1098612X14545273. PMID 25146662.
- ↑ 135.0 135.1 135.2 "Mirataz EPAR". European Medicines Agency. 11 October 2019. Archived from the original on 29 October 2020. Retrieved 12 July 2020. Text was copied from this source, which is © European Medicines Agency, 2020. Reproduction is authorised provided the source is acknowledged.
- ↑ 136.0 136.1 136.2 "Mirataz- mirtazapine ointment". DailyMed. 8 May 2020. Archived from the original on 12 July 2020. Retrieved 12 July 2020.
External links
| External sites: | |
|---|---|
| Identifiers: |
|
- Pages using duplicate arguments in template calls
- CS1: long volume value
- CS1 maint: unrecognized language
- All articles lacking reliable references
- Articles lacking reliable references from October 2011
- Articles with invalid date parameter in template
- CS1 Nederlands-language sources (nl)
- CS1 errors: missing periodical
- Use dmy dates from August 2017
- Drugs with non-standard legal status
- Chemical articles with unknown parameter in Infobox drug
- Chemical articles without CAS registry number
- Articles without EBI source
- Chemical pages without ChemSpiderID
- Chemical pages without DrugBank identifier
- Articles without KEGG source
- Articles without UNII source
- Drugs missing an ATC code
- Drugboxes which contain changes to verified fields
- Drugboxes which contain changes to watched fields
- Articles with hatnote templates targeting a nonexistent page
- Alpha-2 blockers
- Antiemetics
- Anxiolytics
- Schering-Plough brands
- Merck & Co. brands
- Appetite stimulants
- H1 receptor antagonists
- Kappa agonists
- Noradrenergic and specific serotonergic antidepressants
- Oneirogens
- Sedatives
- Serotonin antagonists
- Tetracyclic antidepressants
- RTT