Blood pressure measurement
| Blood pressure measurement | |
|---|---|
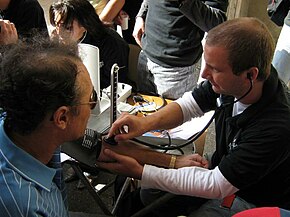 A medical student checking blood pressure using a sphygmomanometer and stethoscope. | |
| Test of | Blood pressure |
| Based on | CNAP vascular unloading technique |
| MedlinePlus | 007490 |
Arterial blood pressure is most commonly measured via a sphygmomanometer, which historically used the height of a column of mercury to reflect the circulating pressure.[1] Blood pressure values are generally reported in millimetres of mercury (mmHg), though aneroid and electronic devices do not contain mercury.
For each heartbeat, blood pressure varies between systolic and diastolic pressures. Systolic pressure is peak pressure in the arteries, which occurs near the end of the cardiac cycle when the ventricles are contracting. Diastolic pressure is minimum pressure in the arteries, which occurs near the beginning of the cardiac cycle when the ventricles are filled with blood. An example of normal measured values for a resting, healthy adult human is 120 mmHg systolic and 80 mmHg diastolic (written as 120/80 mmHg, and spoken as "one-twenty over eighty").
Systolic and diastolic arterial blood pressures are not static but undergo natural variations[2] from one heartbeat to another and throughout the day (in a circadian rhythm). They also change in response to stress, nutritional factors, drugs, disease, exercise, and momentarily from standing up. Sometimes the variations are large. Hypertension refers to arterial pressure being abnormally high, as opposed to hypotension, when it is abnormally low. Along with body temperature, respiratory rate, and pulse rate, blood pressure is one of the four main vital signs routinely monitored by medical professionals and healthcare providers.[3]
Measuring pressure invasively, by penetrating the arterial wall to take the measurement, is much less common and usually restricted to a hospital setting.
Non-invasive
The non-invasive auscultatory and oscillometric measurements are simpler and quicker than invasive measurements, require less expertise, have virtually no complications, are less unpleasant and less painful for the patient. However, non-invasive methods may yield somewhat lower accuracy and small systematic differences in numerical results. Non-invasive measurement methods are more commonly used for routine examinations and monitoring. New non-invasive and continuous technologies based on the CNAP vascular unloading technique, are making non-invasive measurement of blood pressure and further advanced hemodynamic parameters more applicable in general anesthesia and surgery where periods of hypotension might be missed by intermittent measurements.[4]
Palpation
A minimum systolic value can be roughly estimated by palpation, most often used in emergency situations, but should be used with caution.[5] It has been estimated that, using 50% percentiles, carotid, femoral and radial pulses are present in patients with a systolic blood pressure > 70 mmHg, carotid and femoral pulses alone in patients with systolic blood pressure of > 50 mmHg, and only a carotid pulse in patients with a systolic blood pressure of > 40 mmHg.[5]
A more accurate value of systolic blood pressure can be obtained with a sphygmomanometer and palpating the radial pulse.[6] Methods using constitutive models have been proposed to measure blood pressure from radial artery pulse.[citation needed] The diastolic blood pressure cannot be estimated by this method. The American Heart Association recommends that palpation be used to get an estimate before using the auscultatory method.
Auscultatory



The auscultatory method (from the Latin word for "listening") uses a stethoscope and a sphygmomanometer. This comprises an inflatable (Riva-Rocci) cuff placed around the upper arm at roughly the same vertical height as the heart, attached to a mercury or aneroid manometer. The mercury manometer, considered the gold standard, measures the height of a column of mercury, giving an absolute result without need for calibration and, consequently, not subject to the errors and drift of calibration which affect other methods. The use of mercury manometers is often required in clinical trials and for the clinical measurement of hypertension in high-risk patients, such as pregnant women.
A cuff of the appropriate size[7] is fitted smoothly and also snugly, then inflated manually by repeatedly squeezing a rubber bulb until the artery is completely occluded. It is important that the cuff size is correct: undersized cuffs record too high a pressure; oversized cuffs may yield too low a pressure.[8] Usually three or four cuff sizes should be available to allow measurements in arms of different size.[8] Listening with the stethoscope to the brachial artery at the antecubital area of the elbow, the examiner slowly releases the pressure in the cuff. When blood just starts to flow in the artery, the turbulent flow creates a "whooshing" or pounding (first Korotkoff sound).[9] The pressure at which this sound is first heard is the systolic blood pressure. The cuff pressure is further released until no sound can be heard (fifth Korotkoff sound), at the diastolic arterial pressure.
The auscultatory method is the predominant method of clinical measurement.[10]
Oscillometric
The oscillometric method was first demonstrated in 1876 and involves the observation of oscillations in the sphygmomanometer cuff pressure[11] which are caused by the oscillations of blood flow, i.e., the pulse.[12] The electronic version of this method is sometimes used in long-term measurements and general practice. The first fully automated oscillometric blood pressure cuff called the Dinamap 825, an acronym for "Device for Indirect Non-invasive Mean Arterial Pressure", was made available in 1976.[13] It was replaced in 1978 by the Dinamap 845 which could also measure systolic and diastolic blood pressure, as well as heart rate.[14]
The oscillometric method uses a sphygmomanometer cuff, like the auscultatory method, but with an electronic pressure sensor (transducer) to observe cuff pressure oscillations, electronics to automatically interpret them, and automatic inflation and deflation of the cuff. The pressure sensor should be calibrated periodically to maintain accuracy.[15] Oscillometric measurement requires less skill than the auscultatory technique and may be suitable for use by untrained staff and for automated patient home monitoring. As for the auscultatory technique it is important that the cuff size is appropriate for the arm. There are some single cuff devices that may be used for arms of differing sizes, although experience with these is limited.[8]
The cuff is inflated to a pressure initially in excess of the systolic arterial pressure and then reduced to below diastolic pressure over a period of about 30 seconds. When blood flow is nil (cuff pressure exceeding systolic pressure) or unimpeded (cuff pressure below diastolic pressure), cuff pressure will be essentially constant. When blood flow is present, but restricted, the cuff pressure, which is monitored by the pressure sensor, will vary periodically in synchrony with the cyclic expansion and contraction of the brachial artery, i.e., it will oscillate.
Over the deflation period, the recorded pressure waveform forms a signal known as the cuff deflation curve. A bandpass filter is utilized to extract the oscillometric pulses from the cuff deflation curve. Over the deflation period, the extracted oscillometric pulses form a signal known as the oscillometric waveform (OMW). The amplitude of the oscillometric pulses increases to a maximum and then decreases with further deflation. A variety of analysis algorithms can be employed in order to estimate the systolic, diastolic, and mean arterial pressure.
Oscillometric monitors may produce inaccurate readings in patients with heart and circulation problems, which include arteriosclerosis, arrhythmia, preeclampsia, pulsus alternans, and pulsus paradoxus.[8][16]
In practice the different methods do not give identical results; an algorithm and experimentally obtained coefficients are used to adjust the oscillometric results to give readings which match the auscultatory results as well as possible. Some equipment uses computer-aided analysis of the instantaneous arterial pressure waveform to determine the systolic, mean, and diastolic points. Since many oscillometric devices have not been validated, caution must be given as most are not suitable in clinical and acute care settings.
Recently, several coefficient-free oscillometric algorithms have developed for estimation of blood pressure.[15] These algorithms do not rely on experimentally obtained coefficients and have been shown to provide more accurate and robust estimation of blood pressure. These algorithms are based on finding the fundamental relationship between the oscillometric waveform and the blood pressure using modeling[17] and learning[18] approaches. Pulse transit time measurements have been also used to improve oscillometric blood pressure estimates.[19]
The term NIBP, for non-invasive blood pressure, is often used to describe oscillometric monitoring equipment.
Continuous noninvasive techniques
Continuous Noninvasive Arterial Pressure (CNAP) is the method of measuring beat-to-beat arterial blood pressure in real-time without any interruptions and without cannulating the human body. CNAP combines the advantages of the two clinical gold standards: it measures blood pressure continuously in real-time like the invasive arterial catheter system and it is noninvasive like the standard upper arm sphygmomanometer. Latest developments in this field show promising results in terms of accuracy, ease of use and clinical acceptance. An advanced hemodynamic monitoring system incorporating the CNAP method is the NICCI technology of the company Pulsion Medical Systems. The system uses photoplethysmography to detect the blood flow in the patient's fingers and pressure cuffs to create a constant flow. The resulting pressure in the finger sensor corresponds to the real arterial pressure. Based on the vascular unloading technique, the NICCI Technology provides continuous and noninvasive hemodynamic parameters during surgeries. The measurement results are comparable to invasive arterial line measurements in terms of continuity, accuracy and waveform dynamics.
Pulse wave velocity
Since the 1990s a novel family of techniques based on the so-called pulse wave velocity (PWV) principle have been developed. These techniques rely on the fact that the velocity at which an arterial pressure pulse travels along the arterial tree depends, among others, on the underlying blood pressure.[20] Accordingly, after a calibration maneuver, these techniques provide indirect estimates of blood pressure by translating PWV values into blood pressure values.[21] The main advantage of these techniques is that it is possible to measure PWV values of a subject continuously (beat-by-beat), without medical supervision, and without the need of continuously inflating brachial cuffs.[22]
Ambulatory and home monitoring
Ambulatory blood pressure devices take readings regularly (e.g. every half-hour throughout the day and night). They have been used to exclude measurement problems like white-coat hypertension and provide more reliable estimates of usual blood pressure and cardiovascular risk. Blood pressure readings outside of a clinical setting are usually slightly lower in the majority of people; however studies that quantified the risks from hypertension and the benefits of lowering blood pressure have mostly been based on readings in a clinical environment. Use of ambulatory measurements is not widespread but guidelines developed by the UK National Institute for Health and Care Excellence and the British Hypertension Society recommended that 24-hour ambulatory blood pressure monitoring should be used for diagnosis of hypertension.[23] Health economic analysis suggested that this approach would be cost effective compared with repeated clinic measurements.[24] Not all home blood pressure machines are accurate,[25] and "wide range" (one-size fits all) home blood pressure monitoring units do not have adequate evidence to support their use.[26] In addition, health care professionals are recommending that people validate their home devices before relying on the results.[27]
Home monitoring is a cheap and simple alternative to ambulatory blood pressure monitoring, although it does not usually allow assessment of blood pressure during sleep which may be a disadvantage.[28][29] Automatic self-contained blood pressure monitors are available at reasonable prices, however measurements may not be accurate in patients with atrial fibrillation or other arrhythmias such as frequent ectopic beats.[28][29] Home monitoring may be used to improve hypertension management and to monitor the effects of lifestyle changes and medication related to blood pressure.[30] Compared to ambulatory blood pressure measurements, home monitoring has been found to be an effective and lower cost alternative,[28][31][32] but ambulatory monitoring is more accurate than both clinic and home monitoring in diagnosing hypertension.
When measuring blood pressure in the home, an accurate reading requires that one not drink coffee, smoke cigarettes, or engage in strenuous exercise for 30 minutes before taking the reading. A full bladder may have a small effect on blood pressure readings; if the urge to urinate arises, one should do so before the reading. For 5 minutes before the reading, one should sit upright in a chair with one's feet flat on the floor and with limbs uncrossed. The blood pressure cuff should always be against bare skin, as readings taken over a shirt sleeve are less accurate. The same arm should be used for all measurements. During the reading, the arm that is used should be relaxed and kept at heart level, for example by resting it on a table.[33]
Since blood pressure varies throughout the day, home measurements should be taken at the same time of day. A Joint Scientific Statement From the American Heart Association, American Society of Hypertension, and Preventive Cardiovascular Nurses Association on home monitoring in 2008[29] recommended that 2 to 3 readings should be taken in the morning (after awakening, before washing/dressing, taking breakfast/drink or taking medication) and another 2 to 3 readings at night, each day over a period of 1 week. It was also recommended that the readings from the first day should be discarded and that a total of ≥12 readings (i.e. at least two readings per day for the remaining 6 days of the week) should be used for making clinical decisions.
Observer error
There are many factors that can play a role in the blood pressure reading by physician, such as hearing problem, auditory perception of the physician. Karimi Hosseini et al. evaluated the interobserver differences among specialists without any auditory impairment, and reported 68% of observers recorded systolic blood pressure in a range of 9.4 mmHg, diastolic blood pressure in a range of 20.5 mmHg and mean blood pressure in a range of 16.1mmHg.[citation needed] Neufeld et al. reported standard deviations for both systolic and diastolic readings were roughly 3.5 to 5.5 mm Hg. In general standard deviation for the diastolic pressure would be greater because of the difficulty in judging when the sounds disappear.[34]
White-coat hypertension
For some patients, blood pressure measurements taken in a doctor's office may not correctly characterize their typical blood pressure.[35] In up to 25% of patients, the office measurement is higher than their typical blood pressure. This type of error is called white-coat hypertension (WCH) and can result from anxiety related to an examination by a health care professional.[36] White coat hypertension can also occur because, in a clinical setting, patients are seldom given the opportunity to rest for five minutes before blood pressure readings are taken. The misdiagnosis of hypertension for these patients can result in needless and possibly harmful medication. WCH can be reduced (but not eliminated) with automated blood pressure measurements over 15 to 20 minutes in a quiet part of the office or clinic.[37] In some cases a lower blood pressure reading occurs at the doctor's - this has been termed 'masked hypertension'.[38]
Alternative settings, such as pharmacies, have been proposed as alternatives to office blood pressure. The threshold for blood pressure from pharmacy readings is 135/85 mmHg, suggesting a reduced white coat effect, similar to daytime ambulatory measurements.[39][clarification needed]
Invasive
Arterial blood pressure is most accurately measured invasively through an arterial line. Invasive arterial pressure measurement with intravascular cannulae involves direct measurement of arterial pressure by placing a cannula needle in an artery (usually radial, femoral, dorsalis pedis or brachial). The cannula is inserted either via palpation or with the use of ultrasound guidance.[40]
The cannula must be connected to a sterile, fluid-filled system, which is connected to an electronic pressure transducer. The advantage of this system is that pressure is constantly monitored beat-by-beat, and a waveform (a graph of pressure against time) can be displayed. This invasive technique is regularly employed in human and veterinary intensive care medicine, anesthesiology, and for research purposes.
Cannulation for invasive vascular pressure monitoring is infrequently associated with complications such as thrombosis, infection, and bleeding. Patients with invasive arterial monitoring require very close supervision, as there is a danger of severe bleeding if the line becomes disconnected. It is generally reserved for patients where rapid variations in arterial pressure are anticipated.
Invasive vascular pressure monitors are pressure monitoring systems designed to acquire pressure information for display and processing. There are a variety of invasive vascular pressure monitors for trauma, critical care, and operating room applications. These include single pressure, dual pressure, and multi-parameter (i.e. pressure / temperature). The monitors can be used for measurement and follow-up of arterial, central venous, pulmonary arterial, left atrial, right atrial, femoral arterial, umbilical venous, umbilical arterial, and intracranial pressures.
References
- ^ Booth J (1977). "A short history of blood pressure measurement". Proceedings of the Royal Society of Medicine. 70 (11): 793–799. doi:10.1177/003591577707001112. PMC 1543468. PMID 341169.
- ^ "Blood pressure measurement: MedlinePlus Medical Encyclopedia". medlineplus.gov. Retrieved 2020-04-30.
- ^ "Vital Signs (Body Temperature, Pulse Rate, Respiration Rate, Blood Pressure)". OHSU Health Information. Oregon Health & Science University. Retrieved 2014-04-16.
- ^ Solà, Josep; Proença, Martin; Braun, Fabian; Pierrel, Nicolas; Degiorgis, Yan; Verjus, Christophe; Lemay, Mathieu; Bertschi, Mattia; Schoettker, Patrick (1 September 2016). "Continuous non-invasive monitoring of blood pressure in the operating room: a cuffless optical technology at the fingertip". Current Directions in Biomedical Engineering. 2 (1): 267–271. doi:10.1515/cdbme-2016-0060.
- ^ a b Deakin CD, Low JL (September 2000). "Accuracy of the advanced trauma life support guidelines for predicting systolic blood pressure using carotid, femoral, and radial pulses: observational study". BMJ. 321 (7262): 673–674. doi:10.1136/bmj.321.7262.673. PMC 27481. PMID 10987771.
- ^ Interpretation – Blood Pressure – Vitals Archived 2012-07-02 at archive.today, University of Florida, accessed 2008-03-18
- ^ M.M. Chiappa, Y. Ostchega (2013). "Mean mid-arm circumference and blood pressure cuff sizes for U.S. adults: National Health and Nutrition Examination Survey, 1999-2010". Blood Pressure Monitoring. 18 (3): 138–143. doi:10.1097/MBP.0b013e3283617606. PMC 9681024. PMID 23604196. S2CID 45820114.
- ^ a b c d O'Brien E, Asmar R, Beilin L, Imai Y, Mallion JM, Mancia G, Mengden T, Myers M, Padfield P, Palatini P, Parati G, Pickering T, Redon J, Staessen J, Stergiou G, Verdecchia P (2003). "European Society of Hypertension recommendations for conventional, ambulatory and home blood pressure measurement". J. Hypertens. 21 (5): 821–848. doi:10.1097/00004872-200305000-00001. PMID 12714851. S2CID 3952069.
- ^ Audio recordings of Korotkoff sounds. Slide seven of twenty-two, Cardiff University/Prfysgol Caerdydd. Accessed 27 September 2016
- ^ (Pickering et al. 2005, p. 146) See Blood Pressure Measurement Methods.
- ^ (Pickering et al. 2005, p. 147) See The Oscillometric Technique.
- ^ Laurent, P (2003-09-28). "Blood Pressure & Hypertension". Retrieved 2009-10-05.
- ^ "Dinamap 1045". The Wood Library-Museum. Retrieved 14 December 2020.
- ^ Westhorpe, R.N. (May 2009). "Blood Pressure Monitoring – Automated Non-invasive Blood Pressure Monitors". Anaesthesia and Intensive Care. 37 (3): 343. doi:10.1177/0310057X0903700321. PMID 19499853.
- ^ a b Forouzanfar, M.; Dajani, H. R.; Groza, V. Z.; Bolic, M.; Rajan, S.; Batkin, I. (2015-01-01). "Oscillometric Blood Pressure Estimation: Past, Present, and Future". IEEE Reviews in Biomedical Engineering. 8: 44–63. doi:10.1109/RBME.2015.2434215. ISSN 1937-3333. PMID 25993705. S2CID 8940215.
- ^ Hamzaoui O, Monnet X, Teboul JL (2013). "Pulsus paradoxus". Eur. Respir. J. 42 (6): 1696–1705. doi:10.1183/09031936.00138912. PMID 23222878. S2CID 35428633.
- ^ Forouzanfar M (2014). "Ratio-independent blood pressure estimation by modeling the oscillometric waveform envelope". IEEE Trans. Instrum. Meas. 63 (10): 2501–2503. Bibcode:2014ITIM...63.2501F. doi:10.1109/tim.2014.2332239. S2CID 7494219.
- ^ Forouzanfar, M.; Dajani, H. R.; Groza, V. Z.; Bolic, M.; Rajan, S. (August 2011). "Feature-Based Neural Network Approach for Oscillometric Blood Pressure Estimation". IEEE Transactions on Instrumentation and Measurement. 60 (8): 2786–2796. Bibcode:2011ITIM...60.2786F. doi:10.1109/TIM.2011.2123210. S2CID 7614742.
- ^ Forouzanfar, M.; Ahmad, S.; Batkin, I.; Dajani, H. R.; Groza, V. Z.; Bolic, M. (2013-07-01). "Coefficient-Free Blood Pressure Estimation Based on Pulse Transit Time #x2013;Cuff Pressure Dependence". IEEE Transactions on Biomedical Engineering. 60 (7): 1814–1824. doi:10.1109/TBME.2013.2243148. ISSN 0018-9294. PMID 23372068. S2CID 1578853.
- ^ Asmar, Roland (1999). Arterial Stiffness and Pulse Wave Velocity. Paris: Elsevier. ISBN 978-2-84299-148-7.
- ^ Solà, Josep (2011). Continuous non-invasive blood pressure estimation (PDF). Zurich: ETHZ PhD dissertation.
- ^ Solà, Josep; Delgado-Gonzalo, Ricard (2019). The Handbook of Cuffless Blood Pressure Monitoring. Springer International Publishing. ISBN 978-3-030-24701-0.
- ^ Hypertension Guideline 2011 [CG127] Produced in a collaboration between the British Hypertension Society and NICE. http://guidance.nice.org.uk/CG127/NICEGuidance/pdf/English
- ^ Lovibond K, Jowett S, Barton P, Caulfield M, Heneghan C, Hobbs FD, Hodgkinson J, Mant J, Martin U, Williams B, Wonderling D, McManus RJ (2011). "Cost-effectiveness of options for the diagnosis of high blood pressure in primary care: a modelling study". Lancet. 378 (9798): 1219–1230. doi:10.1016/S0140-6736(11)61184-7. PMID 21868086. S2CID 5151024.
- ^ O'Brien, Eoin; Stergiou, George S.; Turner, Martin J. (2018). "The quest for accuracy of blood pressure measuring devices". Journal of Clinical Hypertension. 20 (7): 1092–1095. doi:10.1111/jch.13279. ISSN 1751-7176. PMC 8031088. PMID 30003703.
- ^ Sprague, Eliott; Padwal, Raj S. (2018). "Adequacy of validation of wide-range cuffs used with home blood pressure monitors: a systematic review". Blood Pressure Monitoring. 23 (5): 219–224. doi:10.1097/MBP.0000000000000344. ISSN 1473-5725. PMID 30074520. S2CID 51908913.
- ^ Ruzicka, Marcel; Hiremath, Swapnil (2017-07-01). "Accuracy-Limiting Factor of Home Blood Pressure Monitors?". American Journal of Hypertension. 30 (7): 661–664. doi:10.1093/ajh/hpx056. ISSN 1941-7225. PMID 28430845.
- ^ a b c Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G, Grassi G, Heagerty AM, Kjeldsen SE, Laurent S, Narkiewicz K, Ruilope L, Rynkiewicz A, Schmieder RE, Struijker Boudier HA, Zanchetti A, Vahanian A, Camm J, De Caterina R, Dean V, Dickstein K, Filippatos G, Funck-Brentano C, Hellemans I, Kristensen SD, McGregor K, Sechtem U, Silber S, Tendera M, Widimsky P, Zamorano JL, Kjeldsen SE, Erdine S, Narkiewicz K, Kiowski W, Agabiti-Rosei E, Ambrosioni E, Cifkova R, Dominiczak A, Fagard R, Heagerty AM, Laurent S, Lindholm LH, Mancia G, Manolis A, Nilsson PM, Redon J, Schmieder RE, Struijker-Boudier HA, Viigimaa M, Filippatos G, Adamopoulos S, Agabiti-Rosei E, Ambrosioni E, Bertomeu V, Clement D, Erdine S, Farsang C, Gaita D, Kiowski W, Lip G, Mallion JM, Manolis AJ, Nilsson PM, O'Brien E, Ponikowski P, Redon J, Ruschitzka F, Tamargo J, van Zwieten P, Viigimaa M, Waeber B, Williams B, Zamorano JL (June 2007). "2007 Guidelines for the management of arterial hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC)". Eur Heart J. 28 (12): 1462–1536. doi:10.1093/eurheartj/ehm236. PMID 17562668.
- ^ a b c Pickering TG, Miller NH, Ogedegbe G, Krakoff LR, Artinian NT, Goff D (2008). "Call to action on use and reimbursement for home blood pressure monitoring: executive summary: a joint scientific statement from the American Heart Association, American Society Of Hypertension, and Preventive Cardiovascular Nurses Association". Hypertension. 52 (1): 1–9. doi:10.1161/HYPERTENSIONAHA.107.189011. PMID 18497371.
- ^ Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jones DW, Materson BJ, Oparil S, Wright JT, Roccella EJ (December 2003). "Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure". Hypertension. 42 (6): 1206–1252. doi:10.1161/01.HYP.0000107251.49515.c2. PMID 14656957.
- ^ Niiranen TJ, Kantola IM, Vesalainen R, Johansson J, Ruuska MJ (2006). "A comparison of home measurement and ambulatory monitoring of blood pressure in the adjustment of antihypertensive treatment". Am J Hypertens. 19 (5): 468–474. doi:10.1016/j.amjhyper.2005.10.017. PMID 16647616.
- ^ Shimbo D, Pickering TG, Spruill TM, Abraham D, Schwartz JE, Gerin W (2007). "The Relative Utility of Home, Ambulatory, and Office Blood Pressures in the Prediction of End-Organ Damage". Am J Hypertens. 20 (5): 476–482. doi:10.1016/j.amjhyper.2006.12.011. PMC 1931502. PMID 17485006.
- ^ "How to prepare for a blood pressure test". National Heart, Lung and Blood Institute. Archived from the original on 2021-04-07.
- ^ Neufeld, PD; Johnson, DL (15 September 1986). "Observer error in blood pressure measurement". Canadian Medical Association Journal. 135 (6): 633–637. PMC 1491295. PMID 3756693.
- ^ Elliot, Victoria Stagg (2007-06-11). "Blood pressure readings often unreliable". American Medical News. American Medical Association. Archived from the original on 2008-11-12. Retrieved 2008-08-16.
- ^ Jhalani J, Goyal T, Clemow L, Schwartz JE, Pickering TG, Gerin W (2005). "Anxiety and outcome expectations predict the white-coat effect". Blood Pressure Monitoring. 10 (6): 317–319. doi:10.1097/00126097-200512000-00006. PMID 16496447. S2CID 2058260.
- ^ (Pickering et al. 2005, p. 145) See White Coat Hypertension or Isolated Office Hypertension.
- ^ (Pickering et al. 2005, p. 146) See Masked Hypertension or Isolated Ambulatory Hypertension.
- ^ Albasri, Ali; OʼSullivan, Jack W.; Roberts, Nia W.; Prinjha, Suman; McManus, Richard J.; Sheppard, James P. (October 2017). "A comparison of blood pressure in community pharmacies with ambulatory, home and general practitioner office readings". Journal of Hypertension. 35 (10): 1919–1928. doi:10.1097/HJH.0000000000001443. PMC 5585128. PMID 28594707.
- ^ White, L; Halpin, A; Turner, M; Wallace, L (22 April 2016). "Ultrasound-guided radial artery cannulation in adult and paediatric populations: a systematic review and meta-analysis". British Journal of Anaesthesia. 116 (5): 610–617. doi:10.1093/bja/aew097. PMID 27106964.
Sources
- Pickering, Thomas G.; Hall, John E.; Appel, Lawrence J.; Falkner, Bonita E.; Graves, John; Hill, Martha N.; Jones, Daniel W.; Kurtz, Theodore; Sheps, Sheldon G.; Roccella, Edward J. (2005). "Recommendations for Blood Pressure Measurement in Humans and Experimental Animals: Part 1: Blood Pressure Measurement in Humans: A Statement for Professionals From the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research". Hypertension. 45 (1): 142–161. doi:10.1161/01.HYP.0000150859.47929.8e. PMID 15611362.