Arteriovenous malformation
| Arteriovenous malformation | |
|---|---|
| Other names: AVM | |
 | |
| Micrograph of an arteriovenous malformation in the brain. HPS stain. | |
| Specialty | Neurosurgery |
| Symptoms | None, pain, seizures, stroke symptoms[1] |
| Complications | Bleeding, steal syndrome, heart failure[2][1] |
| Causes | Unknown[1] |
| Diagnostic method | Medical imaging[1] |
| Differential diagnosis | Cavernous malformations, capillary telangiectasias, infantile hemangioma, capillary malformations, arteriovenous fistula[2][1] |
| Treatment | Surgical removal, endovascular embolization, stereotactic radiosurgery[2][1] |
Arteriovenous malformation is an abnormal connection between an artery and vein, without intervening capillaries.[2] Often no symptoms are present, though sometimes pain, seizures, or stroke symptoms may occur.[1] Complications may include bleeding (~4% of cases), steal syndrome, or heart failure.[2][1]
Types include AVMs of the brain and spinal cord, though any part of the body may be involved.[2][1] The cause in most cases is unclear.[1] Risk factors for brain AVMs include hereditary hemorrhagic telangiectasia.[2] Diagnosis is usually confirmed by medical imaging.[1]
AVMs may be treated with surgical removal, endovascular embolization, or stereotactic radiosurgery.[2][1] If issues have not occurred by the age of 50, they are unlikely to occur.[1] Cerebral AVMs newly occur in about 1.3 people per 100,000 per years.[2] Males and females are affected equally.[3] Death occurs as a result, in about 1% of those affected.[1] AVMs were first described in the mid-1800s.[4]
Signs and symptoms
Symptoms of AVM vary according to the location of the malformation.
Brain
Roughly 88%[5] of people with an AVM are asymptomatic; often the malformation is discovered as part of an autopsy or during treatment of an unrelated disorder (called in medicine an "incidental finding"); in rare cases, its expansion or a micro-bleed from an AVM in the brain can cause epilepsy, neurological deficit, or pain.
The most general symptoms of a cerebral AVM include headaches and epileptic seizures, with more specific symptoms occurring that normally depend on the location of the malformation and the individual. Such possible symptoms include:[6]
- Difficulties with movement coordination, including muscle weakness and even paralysis;
- Vertigo (dizziness);
- Difficulties of speech (dysarthria) and communication, such as aphasia;
- Difficulties with everyday activities, such as apraxia;
- Abnormal sensations (numbness, tingling, or spontaneous pain);
- Memory and thought-related problems, such as confusion, dementia or hallucinations.
Cerebral AVMs may present themselves in a number of different ways:
- Bleeding (45% of cases)
- Acute onset of severe headache. May be described as the worst headache of the patient's life. Depending on the location of bleeding, may be associated with new fixed neurologic deficit. In unruptured brain AVMs, the risk of spontaneous bleeding may be as low as 1% per year. After a first rupture, the annual bleeding risk may increase to more than 5%.[7]
- Seizure or brain seizure (46%) Depending on the place of the AVM, it can cause loss of vision in one place.
- Headache (34%)
- Progressive neurologic deficit (21%)
- May be caused by mass effect or venous dilatations. Presence and nature of the deficit depend on location of lesion and the draining veins.[8]
- Pediatric patients
- Heart failure
- Macrocephaly
- Prominent scalp veins
Lungs
Pulmonary arteriovenous malformations are abnormal communications between the veins and arteries of the pulmonary circulation, leading to a right-to-left blood shunt.[9][10] They have no symptoms in up to 29% of all cases,[11] however they can give rise to serious complications including hemorrhage, and infection.[9] They are most commonly associated with hereditary hemorrhagic telangiectasia.[10]
Genetics
Can occur due to autosomal dominant diseases, such as hereditary hemorrhagic telangiectasia.[citation needed]
Pathophysiology
Arteries and veins are part of the vascular system. Arteries carry blood away from the heart to the lungs or the rest of the body, where the blood passes through capillaries, and veins return the blood to the heart. An AVM interferes with this process by forming a direct connection of the arteries and veins. AVMs can cause intense pain and lead to serious medical problems. Although AVMs are often associated with the brain and spinal cord, they can develop in any part of the body.
Normally, the arteries in the vascular system carry oxygen-rich blood, except in the case of the pulmonary artery. Structurally, arteries divide and sub-divide repeatedly, eventually forming a sponge-like capillary bed. Blood moves through the capillaries, giving up oxygen and taking up waste products, including CO
2, from the surrounding cells. Capillaries in turn successively join together to form veins that carry blood away. The heart acts to pump blood through arteries and uptake the venous blood.
As an AVM lacks the dampening effect of capillaries on the blood flow, the AVM can get progressively larger over time as the amount of blood flowing through it increases, forcing the heart to work harder to keep up with the extra blood flow. It also causes the surrounding area to be deprived of the functions of the capillaries—removal of CO
2 and delivery of nutrients to the cells. The resulting tangle of blood vessels, often called a nidus (Latin for "nest"), has no capillaries. It can be extremely fragile and prone to bleeding because of the abnormally direct connections between high-pressure arteries and low-pressure veins. The resultant sign, audible via stethoscope, is a rhythmic, whooshing sound caused by excessively rapid blood flow through the arteries and veins. It has been given the term "bruit", French for noise. On some occasions, a patient with a brain AVM may become aware of the noise, which can compromise hearing and interfere with sleep in addition to causing psychological distress.
Diagnosis

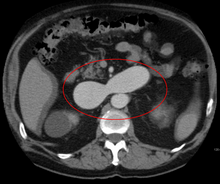
AVMs are diagnosed primarily by the following imaging methods:
- Computerized tomography (CT) scan is a noninvasive X-ray to view the anatomical structures within the brain to detect blood in or around the brain. A newer technology called CT angiography involves the injection of contrast into the blood stream to view the arteries of the brain. This type of test provides the best pictures of blood vessels through angiography and soft tissues through CT.
- Magnetic resonance imaging (MRI) scan is a noninvasive test, which uses a magnetic field and radio-frequency waves to give a detailed view of the soft tissues of the brain.
- Magnetic resonance angiography (MRA) – scans created using magnetic resonance imaging to specifically image the blood vessels and structures of the brain. A magnetic resonance angiogram can be an invasive procedure, involving the introduction of contrast dyes (e.g., gadolinium MR contrast agents) into the vasculature of a patient using a catheter inserted into an artery and passed through the blood vessels to the brain. Once the catheter is in place, the contrast dye is injected into the bloodstream and the MR images are taken. Additionally or alternatively, flow-dependent or other contrast-free magnetic resonance imaging techniques can be used to determine the location and other properties of the vasculature.
AVMs can occur in various parts of the body:
- brain (cerebral AV malformation)
- spleen[12]
- lung[13][14]
- kidney[15]
- spinal cord[16]
- liver[17]
- intercostal space[18]
- iris[19]
- spermatic cord[20]
- extremities – arm, shoulder, etc.
AVMs may occur in isolation or as a part of another disease (for example, Von Hippel-Lindau disease or hereditary hemorrhagic telangiectasia).
AVMs have been shown to be associated with aortic stenosis.[21]
Bleeding from an AVM can be relatively mild or devastating. It can cause severe and less often fatal strokes. If a cerebral AVM is detected before a stroke occurs, usually the arteries feeding blood into the nidus can be closed off to avert the danger. However, interventional therapy may also be relatively risky.
Treatment
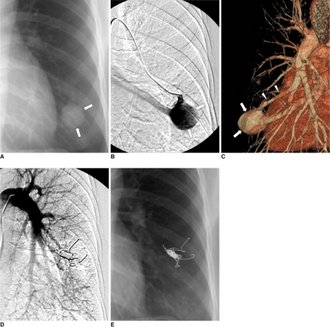
Treatment for brain AVMs can be symptomatic, and patients should be followed by a neurologist for any seizures, headaches, or focal neurologic deficits. AVM-specific treatment may also involve endovascular embolization, neurosurgery or radiosurgery.[6] Embolization, that is, cutting off the blood supply to the AVM with coils, particles, acrylates, or polymers introduced by a radiographically guided catheter, may be used in addition to neurosurgery or radiosurgery, but is rarely successful in isolation except in smaller AVMs.[22] Gamma knife may also be used.[23]
Treatment of lung AVMs is typically performed with endovascular embolization alone, which is considered the standard of care. [24]
Epidemiology
The estimated detection rate of AVM in the US general population is 1.4/100,000 per year.[25] This is approximately one fifth to one seventh the incidence of intracranial aneurysms. An estimated 300,000 Americans have AVMs, of whom 12% (approximately 36,000) will exhibit symptoms of greatly varying severity.[6]
History
Luschka (1820–1875) and Virchow (1821–1902) first described arteriovenous malformations in the mid-1800s. Olivecrona (1891–1980) performed the first surgical excision of an intracranial AVM in 1932.
Notable cases
- Indonesian actress Egidia Savitri died from complications of AVM on November 29, 2013.[26]
- Phoenix Suns point guard AJ Price nearly died from AVM in 2004 while a student at the University of Connecticut.
- On December 13, 2006, Senator Tim Johnson of South Dakota was diagnosed with AVM and treated at George Washington University Hospital.[27]
- On August 3, 2011, Mike Patterson of the Philadelphia Eagles collapsed on the field and suffered a seizure during a practice, leading to him being diagnosed with AVM.[28]
- Actor Ricardo Montalbán was born with spinal AVM.[29] During the filming of the 1951 film Across the Wide Missouri, Montalbán was thrown from his horse, knocked unconscious, and trampled by another horse which aggravated his AVM and resulted in a painful back injury that never healed. The pain increased as he aged, and in 1993, Montalbán underwent 9½ hours of spinal surgery which left him paralyzed below the waist and using a wheelchair.[30]
- Actor/comedian T. J. Miller was diagnosed with AVM after filming Yogi Bear in New Zealand in 2010; Miller described his experience with the disease on the Pete Holmes podcast You Made It Weird on October 28, 2011, shedding his comedian side for a moment and becoming more philosophical, narrating his behaviors and inability to sleep during that time. He suffered a seizure upon return to Los Angeles and successfully underwent surgery that had a mortality rate of ten percent.[31]
- Jazz guitarist Pat Martino experienced an AVM and subsequently developed amnesia and manic depression. He eventually re-learned to play the guitar by listening to his own recordings from before the aneurysm. He still records and performs to this day.[32]
- YouTube vlogger Nikki Lilly (Nikki Christou), winner of the 2016 season of Junior Bake Off was born with AVM, which has resulted in some facial disfigurement.[33]
- Composer and lyricist William Finn was diagnosed with AVM and underwent Gamma Knife surgery in September 1992, soon after he won the 1992 Tony Award for best musical, awarded to "Falsettos". [34] Finn wrote the 1998 Off-Broadway musical A New Brain about the experience.
- Former Florida Gators and Oakland Raiders linebacker Neiron Ball was diagnosed with AVM in 2011 while playing for Florida, but recovered and was cleared to play. On September 16, 2018, Ball was placed in a medically induced coma due to complications of the disease, which lasted until his death on September 10, 2019.[35]
- Country music singer Drake White was diagnosed with AVM in January 2019, and is undergoing treatment.
Research
Despite many years of research, the central question of whether to treat AVMs has not been answered. All treatments, whether involving surgery, radiation, or drugs, have risks and side-effects. Therefore, it might be better in some cases to avoid treatment altogether and simply accept a small risk of coming to harm from the AVM itself. This question is currently being addressed in clinical trials.[36]
See also
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 "Arteriovenous Malformations". www.hopkinsmedicine.org. Archived from the original on 3 March 2021. Retrieved 27 February 2021.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 2.8 Zyck, S; Sampath, R (January 2020). "Arteriovenous Malformations". PMID 30285374.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ "Arteriovenous Malformation". NORD (National Organization for Rare Disorders). Archived from the original on 28 January 2021. Retrieved 27 February 2021.
- ↑ Dieter, Robert S.; Jr, Raymond A. Dieter (2013). Endovascular Interventions: A Case-Based Approach. Springer Science & Business Media. p. 39. ISBN 978-1-4614-7312-1. Archived from the original on 2021-08-27. Retrieved 2021-02-27.
- ↑ "National Institute of Neurological Disorders and Stroke". nih.gov. Archived from the original on 5 December 2016. Retrieved 17 March 2018.
- ↑ 6.0 6.1 6.2 Arteriovenous Malformation Information Page at NINDS
- ↑ Stapf, C.; Mast, H.; Sciacca, R. R.; Choi, J. H.; Khaw, A. V.; Connolly, E. S.; Pile-Spellman, J.; Mohr, J. P. (2006). "Predictors of hemorrhage in patients with untreated brain arteriovenous malformation". Neurology. 66 (9): 1350–5. doi:10.1212/01.wnl.0000210524.68507.87. PMID 16682666.
- ↑ Choi, J.H.; Mast, H.; Hartmann, A.; Marshall, R.S.; Pile-Spellman, J.; Mohr, J.P.; Stapf, C. (2009). "Clinical and morphological determinants of focal neurological deficits in patients with unruptured brain arteriovenous malformation". Journal of the Neurological Sciences. 287 (1–2): 126–30. doi:10.1016/j.jns.2009.08.011. PMC 2783734. PMID 19729171.
- ↑ 9.0 9.1 Reichert, M; Kerber, S; Alkoudmani, I; Bodner, J (April 2016). "Management of a solitary pulmonary arteriovenous malformation by video-assisted thoracoscopic surgery and anatomic lingula resection: video and review". Surgical Endoscopy. 30 (4): 1667–9. doi:10.1007/s00464-015-4337-0. PMID 26156615.
- ↑ 10.0 10.1 Tellapuri, S; Park, HS; Kalva, SP (August 2019). "Pulmonary arteriovenous malformations". The international journal of cardiovascular imaging. 35 (8): 1421–1428. doi:10.1007/s10554-018-1479-x. PMID 30386957.
- ↑ Goodenberger DM (2008). "Chapter 84 Pulmonary arteriovenous malformations". Fishman's Pulmonary Diseases and Disorders (4th ed.). McGraw-Hill. p. 1470. ISBN 978-0-07-145739-2.
- ↑ Agrawal, Aditya; Whitehouse, Richard; Johnson, Robert W.; Augustine, Titus (2006). "Giant splenic artery aneurysm associated with arteriovenous malformation". Journal of Vascular Surgery. 44 (6): 1345–9. doi:10.1016/j.jvs.2006.06.049. PMID 17145440.
- ↑ Chowdhury, Ujjwal K.; Kothari, Shyam S.; Bishnoi, Arvind K.; Gupta, Ruchika; Mittal, Chander M.; Reddy, Srikrishna (2009). "Successful Lobectomy for Pulmonary Arteriovenous Malformation Causing Recurrent Massive Haemoptysis". Heart, Lung and Circulation. 18 (2): 135–9. doi:10.1016/j.hlc.2007.11.142. PMID 18294908.
- ↑ Cusumano, Lucas R.; Duckwiler, Gary R.; Roberts, Dustin G.; McWilliams, Justin P. (2019-08-30). "Treatment of Recurrent Pulmonary Arteriovenous Malformations: Comparison of Proximal Versus Distal Embolization Technique". Cardiovascular and Interventional Radiology. doi:10.1007/s00270-019-02328-0. ISSN 1432-086X. PMID 31471718.
- ↑ Barley, Fay L.; Kessel, David; Nicholson, Tony; Robertson, Iain (2006). "Selective Embolization of Large Symptomatic Iatrogenic Renal Transplant Arteriovenous Fistula". CardioVascular and Interventional Radiology. 29 (6): 1084–7. doi:10.1007/s00270-005-0265-z. PMID 16794894.
- ↑ Kishi, K; Shirai, S; Sonomura, T; Sato, M (2005). "Selective conformal radiotherapy for arteriovenous malformation involving the spinal cord". The British Journal of Radiology. 78 (927): 252–4. doi:10.1259/bjr/50653404. PMID 15730991.
- ↑ Bauer, Tilman; Britton, Peter; Lomas, David; Wight, Derek G.D.; Friend, Peter J.; Alexander, Graeme J.M. (1995). "Liver transplantation for hepatic arteriovenous malformation in hereditary haemorrhagic telangiectasia". Journal of Hepatology. 22 (5): 586–90. doi:10.1016/0168-8278(95)80455-2. PMID 7650340.
- ↑ Rivera, Peter P.; Kole, Max K.; Pelz, David M.; Gulka, Irene B.; McKenzie, F. Neil; Lownie, Stephen P. (2006). "Congenital Intercostal Arteriovenous Malformation". American Journal of Roentgenology. 187 (5): W503–6. doi:10.2214/AJR.05.0367. PMID 17056881.
- ↑ Shields, Jerry A.; Streicher, Theodor F. E.; Spirkova, Jane H. J.; Stubna, Michal; Shields, Carol L. (2006). "Arteriovenous Malformation of the Iris in 14 Cases". Archives of Ophthalmology. 124 (3): 370–5. doi:10.1001/archopht.124.3.370. PMID 16534057.
- ↑ Sountoulides, Petros; Bantis, Athanasios; Asouhidou, Irene; Aggelonidou, Hellen (2007). "Arteriovenous malformation of the spermatic cord as the cause of acute scrotal pain: a case report". Journal of Medical Case Reports. 1: 110. doi:10.1186/1752-1947-1-110. PMC 2194703. PMID 17939869.
- ↑ Batur, Pelin; Stewart, William J.; Isaacson, J. Harry (2003). "Increased Prevalence of Aortic Stenosis in Patients With Arteriovenous Malformations of the Gastrointestinal Tract in Heyde Syndrome". Archives of Internal Medicine. 163 (15): 1821–4. doi:10.1001/archinte.163.15.1821. PMID 12912718.
- ↑ Jafar, Jafar J.; Davis, Adam J.; Berenstein, Alejandro; Choi, In Sup; Kupersmith, Mark J. (1993-01-01). "The effect of embolization with N-butyl cyanoacrylate prior to surgical resection of cerebral arteriovenous malformations". Journal of Neurosurgery. 78 (1): 60–69. doi:10.3171/jns.1993.78.1.0060. ISSN 0022-3085. PMID 8416244.
- ↑ "Conditions We Treat". Macquarie University Hospital. Archived from the original on 2013-06-13.
- ↑ Cusumano, Lucas R.; Duckwiler, Gary R.; Roberts, Dustin G.; McWilliams, Justin P. (2019-08-30). "Treatment of Recurrent Pulmonary Arteriovenous Malformations: Comparison of Proximal Versus Distal Embolization Technique". Cardiovascular and Interventional Radiology. doi:10.1007/s00270-019-02328-0. ISSN 1432-086X. PMID 31471718.
- ↑ Stapf, C.; Mast, H.; Sciacca, R.R.; Berenstein, A.; Nelson, P.K.; Gobin, Y.P.; Pile-Spellman, J.; Mohr, J.P. (2003). "The New York Islands AVM Study: Design, Study Progress, and Initial Results". Stroke. 34 (5): e29–33. doi:10.1161/01.STR.0000068784.36838.19. PMID 12690217.
- ↑ Suhendra, Ichsan. "Pesinetron Egidia Savitri Telah Pergi". KOMPAS.com (in Bahasa Indonesia). Kompas Cyber Media. Archived from the original on 15 May 2019. Retrieved 15 May 2019.
- ↑ "Sen. Johnson recovering after brain surgery". AP. December 14, 2006. Archived from the original on November 22, 2015. Retrieved November 17, 2019.
- ↑ "Mike Patterson's Collapse Reportedly Related To Brain AVM". sbnation.com. 2011-08-04. Archived from the original on 2018-03-18. Retrieved 17 March 2018.
- ↑ "Ricardo Montalban tribute" Archived 2019-09-01 at the Wayback Machine YouTube, acceptance speech video of Easter Seals Lifetime Achievement Award
- ↑ "Inside". mahalo.com. Archived from the original on 5 September 2008. Retrieved 17 March 2018.
- ↑ Pete Holmes (October 27, 2011). "You Made It Weird with Pete Holmes". You Made It Weird #2: TJ Miller (Podcast). Nerdist Industries. Event occurs at 37:45. Archived from the original on February 12, 2013. Retrieved December 5, 2012.
- ↑ Vida, Vendela. Confidence, or the Appearance of Confidence: The Best of the Believer Music Interviews. No ed. San Francisco, Calif.: Believer, a Tiny Division of McSweeney's Which Is Also Tiny, 2014. Print.
- ↑ "Junior Bake Off 2016 Winner announced". BBC Media Centre. BBC Online. 25 November 2016. Archived from the original on 26 May 2017. Retrieved 9 April 2017.
- ↑ Pall, Ellen (14 June 1998). "The Long-Running Musical of William Finn's Life". The New York Times. Archived from the original on 1 March 2020. Retrieved 17 March 2018.
- ↑ "Neiron Ball, former Raiders LB, in medically induced coma after aneurysm". ESPN. September 26, 2018. Archived from the original on July 18, 2019. Retrieved July 18, 2019.
- ↑ Research trials in arterio-venous malformations; Rustam Al-Shahi Salman Archived February 17, 2012, at the Wayback Machine
Further reading
| Classification | |
|---|---|
| External resources |
- Pages with script errors
- CS1 errors: missing periodical
- CS1 Bahasa Indonesia-language sources (id)
- Webarchive template wayback links
- All articles with unsourced statements
- Articles with unsourced statements from August 2012
- Articles with invalid date parameter in template
- Congenital vascular defects
- Gross pathology
- RASopathies
- RTT