Alopecia areata
| Alopecia areata | |
|---|---|
| Other names: Alopecia Celsi, vitiligo capitis, Jonston's alopecia[1] | |
 | |
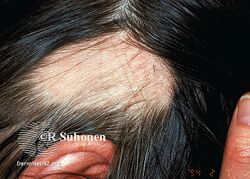
| Alopecia areata seen on the back of the scalp | |
| Pronunciation |
|
| Specialty | Dermatology |
| Symptoms | Areas of hair loss, usually on the scalp[2] |
| Usual onset | Childhood[2] |
| Causes | Autoimmune[2] |
| Risk factors | Family history, rheumatoid arthritis, type 1 diabetes, celiac disease[2][3] |
| Differential diagnosis | Trichotillomania, alopecia mucinosa, postpartum alopecia[1] |
| Treatment | Sunscreen, head coverings to protect from sun and cold[2] |
| Medication | Cortisone injections[1] |
| Prognosis | Does not affect life expectancy[2][1] |
| Frequency | ~2% (US)[2] |
Alopecia areata, also known as spot baldness, is a condition in which hair is lost from some or all areas of the body.[1] Often it results in a few bald spots on the scalp, each about the size of a coin.[2] Psychological stress may result.[2] People are generally otherwise healthy.[2] In a few cases, all the hair on the scalp or all body hair is lost and loss can be permanent.[2][1]
Alopecia areata is believed to be an autoimmune disease resulting from a breach in the immune privilege of the hair follicles.[4] Risk factors include a family history of the condition.[2] Among identical twins, if one is affected, the other has about a 50% chance of also being affected.[2] The underlying mechanism involves failure by the body to recognize its own cells with subsequent immune mediated destruction of the hair follicle.[2]
No cure for the condition is known.[2] Efforts may be used to try to speed hair regrowth such as cortisone injections.[2][1] Sunscreen, head coverings to protect from cold and sun, and glasses if the eyelashes are missing are recommended.[2] In some cases, the hair regrows and the condition does not reoccur.[2] In others, hair loss and regrowth occurs over years.[2] Among those in whom all body hair is lost, less than 10% recover.[5]
About 0.15% of people are affected at any one time and 2% of people are affected at some point in time.[2][5] Onset is usually in childhood.[2] Males and females have the condition in equal numbers.[1] The condition does not affect a person's life expectancy.[2]
Signs and symptoms
Typical first symptoms of alopecia areata are small bald patches. The underlying skin is unscarred and looks superficially normal. Although these patches can take many shapes, they are usually round or oval.[6] Alopecia areata most often affects the scalp and beard, but may occur on any part of the body with hair.[7] Different areas of the skin may exhibit hair loss and regrowth at the same time. The disease may also go into remission for a time, or may be permanent. It is common in children.[citation needed]
The area of hair loss may tingle or be painful.[8] The hair tends to fall out over a short period of time, with the loss commonly occurring more on one side of the scalp than the other.[9]
Exclamation point hairs, narrower along the length of the strand closer to the base, producing a characteristic "exclamation point" appearance, are often present.[9] These hairs are very short (3–4 mm), and can be seen surrounding the bald patches.[10]
When healthy hair is pulled out, at most a few should come out, and ripped hair should not be distributed evenly across the tugged portion of the scalp. In cases of alopecia areata, hair tends to pull out more easily along the edge of the patch where the follicles are already being attacked by the body's immune system than away from the patch where they are still healthy.[11]Nails may have pitting or trachyonychia.[7]
-
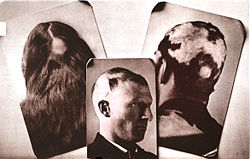
Diffuse alopecia due to severe alopecia areata
-
Alopecia areata
-
Alopecia areata
-
Alopecia areata
Causes

Alopecia areata is thought to be a systemic autoimmune disorder in which the body attacks its own anagen hair follicles and suppresses or stops hair growth.[9] For example, T cell lymphocytes cluster around affected follicles, causing inflammation and subsequent hair loss. Hair follicles in a normal state are thought to be kept secure from the immune system, a phenomenon called immune privilege. A breach in this immune privilege state is considered as the cause of alopecia areata.[4] A few cases of babies being born with congenital alopecia areata have been reported.[12]
Alopecia areata is not contagious.[9] It occurs more frequently in people who have affected family members, suggesting heredity may be a factor.[9] Strong evidence of genetic association with increased risk for alopecia areata was found by studying families with two or more affected members. This study identified at least four regions in the genome that are likely to contain these genes.[13] In addition, alopecia areata shares genetic risk factors with other autoimmune diseases, including rheumatoid arthritis, type 1 diabetes, and celiac disease.[3] It may be the only manifestation of celiac disease.[14][15]
Endogenous retinoids metabolic defect is a key part of the pathogenesis of the alopecia areata.[16]
In 2010, a genome-wide association study was completed that identified 129 single nucleotide polymorphisms that were associated with alopecia areata. The genes that were identified include those involved in controlling the activation and proliferation of regulatory T cells, cytotoxic T lymphocyte-associated antigen 4, interleukin-2, interleukin-2 receptor A, and Eos (also known as Ikaros family zinc finger 4), as well as the human leukocyte antigen. The study also identified two genes, PRDX5 and STX17, that are expressed in the hair follicle.[17]
Diagnosis
Alopecia areata is usually diagnosed based on clinical features.
Trichoscopy may aid in establishing the diagnosis. In alopecia areata, trichoscopy shows regularly distributed "yellow dots" (hyperkeratotic plugs), small exclamation-mark hairs, and "black dots" (destroyed hairs in the hair follicle opening).[18]
Oftentimes, however, discrete areas of hair loss surrounded by exclamation mark hairs is sufficient for clinical diagnosis of alopecia areata. Sometimes, reddening of the skin, erythema, may also be present in the balding area.[5]
A biopsy is rarely needed to make the diagnosis or aid in the management of alopecia areata. Histologic findings may include peribulbar lymphocytic infiltration resembling a "swarm of bees", a shift in the anagen-to-telogen ratio towards telogen, and dilated follicular infundibulae.[3] Other helpful findings can include pigment incontinence in the hair bulb and follicular stelae. Occasionally, in inactive alopecia areata, no inflammatory infiltrates are found.[citation needed]
Classification
Commonly, alopecia areata involves hair loss in one or more round spots on the scalp.[9][19]
- Hair may also be lost more diffusely over the whole scalp, in which case the condition is called diffuse alopecia areata.[9]
- Alopecia areata monolocularis describes baldness in only one spot. It may occur anywhere on the head.
- Alopecia areata multilocularis refers to multiple areas of hair loss.
- Ophiasis refers to hair loss in the shape of a wave at the circumference of the head.
- The disease may be limited only to the beard, in which case it is called alopecia areata barbae.[9]
- If the person loses all the hair on the scalp, the disease is then called alopecia areata totalis.[2]
- If all body hair, including pubic hair, is lost, the diagnosis then becomes alopecia areata universalis.[2]
Alopecia areata totalis and universalis are rare.[20]
Treatment
The objective assessment of treatment efficacy is very difficult and spontaneous remission is unpredictable, but if the affected area is patched, the hair may regrow spontaneously in many cases.[21] None of the existing therapeutic options are curative or preventive.[21]
In cases of severe hair loss, limited success has been achieved by using the corticosteroid medications clobetasol or fluocinonide, corticosteroid injections, or cream. Application of corticosteroid creams to the affected skin is less effective and takes longer to produce results. Steroid injections are commonly used in sites where the areas of hair loss on the head are small or especially where eyebrow hair has been lost. Whether they are effective is uncertain.[citation needed] Some other medications that have been used are minoxidil, Elocon (mometasone) ointment (steroid cream), irritants (anthralin or topical coal tar), and topical immunotherapy ciclosporin, sometimes in different combinations. Topical corticosteroids frequently fail to enter the skin deeply enough to affect the hair bulbs, which are the treatment target,[7] and small lesions typically also regrow spontaneously. Oral corticosteroids may decrease the hair loss, but only for the period during which they are taken, and these medications can cause serious side effects.[7] No one treatment is effective in all cases, and some individuals may show no response to any treatment.[22] Few treatments have been well evaluated. A 2008 meta-analysis of oral and topical corticosteroids, topical ciclosporin, photodynamic therapy, and topical minoxidil showed no benefit of hair growth compared with placebo, especially with regard to long-term benefits.[23]
When alopecia areata is associated with celiac disease, treatment with a gluten-free diet allows for complete and permanent regrowth of scalp and other body hair in many people, but in others, remissions and recurrences are seen.[14] This improvement is probably due to the normalization of the immune response as a result of gluten withdrawal from the diet.[14]
Prognosis
In most cases that begin with a small number of patches of hair loss, hair grows back after a few months to a year.[8] In cases with a greater number of patches, hair can either grow back or progress to alopecia areata totalis or, in rare cases, alopecia areata universalis.[8]
No loss of body function occurs, and the effects of alopecia areata are psychological (loss of self-image due to hair loss), although these can be severe. Loss of hair also means the scalp burns more easily in the sun. Patients may also have aberrant nail formation because keratin forms both hair and nails.[citation needed]
Hair may grow back and then fall out again later. This may not indicate a recurrence of the condition, but rather a natural cycle of growth-and-shedding from a relatively synchronised start; such a pattern will fade over time. Episodes of alopecia areata before puberty predispose to chronic recurrence of the condition.[7]
Alopecia can be the cause of psychological stress. Because hair loss can lead to significant changes in appearance, individuals with it may experience social phobia, anxiety, and depression.[24]
Epidemiology
The condition affects 0.1%–0.2% of the population,[25] and occurs equally in both males and females. Alopecia areata occurs in people who are otherwise healthy and have no other skin disorders.[7] Initial presentation most commonly occurs in the early childhood, late teenage years, or young adulthood, but can happen at any ages.[9] Patients also tend to have a slightly higher incidence of conditions related to the immune system, such as asthma, allergies, atopic dermatitis, and hypothyroidism.
Research
Many medications are being studied.[26] Some of these medications are approved for other diseases, others are not available outside of studies.
In 2014, preliminary findings showing that oral ruxolitinib, a drug approved by the US Food and Drug Administration (FDA) for bone marrow disorder myelofibrosis, restored hair growth in three individuals with long-standing and severe disease.[27] The medicine costs almost US$10,000 a month.[28]
History
Alopecia areata and alopecia barbae have been identified by some as the biblical nethek condition that is part of the greater tzaraath family of skin disorders; the said disorders are purported to being discussed in the Book of Leviticus, chapter 13.[29]
See also
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 "Alopecia Areata - NORD (National Organization for Rare Disorders)". NORD (National Organization for Rare Disorders). 2004. Archived from the original on 21 February 2017. Retrieved 10 July 2017.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 2.13 2.14 2.15 2.16 2.17 2.18 2.19 2.20 2.21 2.22 2.23 2.24 Liaison, Ray Fleming, Office of Communications and Public (May 2016). "Questions and Answers About Alopecia Areata". NIAMS. Archived from the original on 4 July 2017. Retrieved 10 July 2017.
- ↑ 3.0 3.1 3.2 Hordinsky M, Junqueira AL (June 2015). "Alopecia areata update". Seminars in Cutaneous Medicine and Surgery (Review). 34 (2): 72–5. doi:10.12788/j.sder.2015.0160. PMID 26176283.

- ↑ 4.0 4.1 Rajabi, F.; Drake, L.A.; Senna, M.M.; Rezaei, N. (2018). "Alopecia areata: A review of disease pathogenesis". British Journal of Dermatology. 179 (5): 1033–1048. doi:10.1111/bjd.16808. PMID 29791718. S2CID 43940520.
- ↑ 5.0 5.1 5.2 Beigi, Pooya Khan Mohammad (2018). Alopecia Areata: A Clinician's Guide. Springer. p. 14. ISBN 9783319721347. Archived from the original on 2021-08-29. Retrieved 2020-10-01.
- ↑ Freedberg IM, Fitzpatrick TB (2003). Fitzpatrick's dermatology in medicine. New York: McGraw-Hill, Medical Pub. Division. ISBN 978-0-07-138076-8.[page needed]
- ↑ 7.0 7.1 7.2 7.3 7.4 7.5 Alopecia Areata at Merck Manual of Diagnosis and Therapy Professional Edition
- ↑ 8.0 8.1 8.2 American Osteopathic College of Dermatology. Alopecia Areata. Archived 2007-12-13 at the Wayback Machine Dermatologic Disease Database. Aocd.org. Retrieved on December 3, 2007.
- ↑ 9.0 9.1 9.2 9.3 9.4 9.5 9.6 9.7 9.8 Zoe Diana Draelos (August 30, 2007), Alopecia Areata Archived 2007-12-08 at the Wayback Machine. MedicineNet.com. Retrieved on December 2, 2007
- ↑ Donovan, Dr. Jeff. "Exclamation mark hairs in Alopecia Areata are located at the periphary". Donovan Hair Clinic. Archived from the original on 2018-06-21. Retrieved 2018-06-21.
- ↑ Wasserman D, Guzman-Sanchez DA, Scott K, McMichael A (February 2007). "Alopecia areata". International Journal of Dermatology. 46 (2): 121–31. doi:10.1111/j.1365-4632.2007.03193.x. PMID 17269961. S2CID 57279630.
- ↑ Lenane P, Pope E, Krafchik B (February 2005). "Congenital alopecia areata". Journal of the American Academy of Dermatology (Case Reports. Review). 52 (2 Suppl 1): 8–11. doi:10.1016/j.jaad.2004.06.024. PMID 15692503.
We believe AA should be classified not only as an acquired, but also a congenital form of nonscarring hair loss. It may well be more common than is thought because of lack of recognition
- ↑ Martinez-Mir A, Zlotogorski A, Gordon D, Petukhova L, Mo J, Gilliam TC, Londono D, Haynes C, Ott J, Hordinsky M, Nanova K, Norris D, Price V, Duvic M, Christiano AM (February 2007). "Genomewide scan for linkage reveals evidence of several susceptibility loci for alopecia areata". American Journal of Human Genetics. 80 (2): 316–28. doi:10.1086/511442. PMC 1785354. PMID 17236136.
- ↑ 14.0 14.1 14.2 Caproni M, Bonciolini V, D'Errico A, Antiga E, Fabbri P (2012). "Celiac disease and dermatologic manifestations: many skin clue to unfold gluten-sensitive enteropathy". Gastroenterology Research and Practice (Review). 2012: 1–12. doi:10.1155/2012/952753. PMC 3369470. PMID 22693492.
- ↑ Tack GJ, Verbeek WH, Schreurs MW, Mulder CJ (April 2010). "The spectrum of celiac disease: epidemiology, clinical aspects and treatment". Nature Reviews. Gastroenterology & Hepatology (Review). 7 (4): 204–13. doi:10.1038/nrgastro.2010.23. PMID 20212505. S2CID 7951660.
- ↑ Duncan FJ, Silva KA, Johnson CJ, King BL, Szatkiewicz JP, Kamdar SP, Ong DE, Napoli JL, Wang J, King LE, Whiting DA, McElwee KJ, Sundberg JP, Everts HB (February 2013). "Endogenous retinoids in the pathogenesis of alopecia areata". The Journal of Investigative Dermatology. 133 (2): 334–43. doi:10.1038/jid.2012.344. PMC 3546144. PMID 23014334.
- ↑ Petukhova L, Duvic M, Hordinsky M, Norris D, Price V, Shimomura Y, Kim H, Singh P, Lee A, Chen WV, Meyer KC, Paus R, Jahoda CA, Amos CI, Gregersen PK, Christiano AM (July 2010). "Genome-wide association study in alopecia areata implicates both innate and adaptive immunity". Nature. 466 (7302): 113–7. Bibcode:2010Natur.466..113P. doi:10.1038/nature09114. PMC 2921172. PMID 20596022.
- ↑ Rudnicka L, Olszewska M, Rakowska A, Kowalska-Oledzka E, Slowinska M (July 2008). "Trichoscopy: a new method for diagnosing hair loss". Journal of Drugs in Dermatology. 7 (7): 651–4. PMID 18664157. Archived from the original on 2015-09-04.
- ↑ Marks JG, Miller J (2006). Lookingbill and Marks' Principles of Dermatology (4th ed.). Elsevier Inc. ISBN 978-1-4160-3185-7..[page needed]
- ↑ Skin Conditions: Alopecia Areata Archived 2007-12-17 at the Wayback Machine. WebMD. Retrieved on December 2, 2007.
- ↑ 21.0 21.1 Shapiro J (December 2013). "Current treatment of alopecia areata". The Journal of Investigative Dermatology. Symposium Proceedings (Review). 16 (1): S42–4. doi:10.1038/jidsymp.2013.14. PMID 24326551.

- ↑ Alsantali A (2011-07-22). "Alopecia areata: a new treatment plan". Clinical, Cosmetic and Investigational Dermatology. 4: 107–15. doi:10.2147/CCID.S22767. PMC 3149478. PMID 21833161.
- ↑ Delamere, Finola M; Sladden, Michael J; Dobbins, Helen M; Leonardi-Bee, Jo (2008-04-23). "Interventions for alopecia areata". Cochrane Database of Systematic Reviews (2): CD004413. doi:10.1002/14651858.CD004413.pub2. ISSN 1465-1858. PMID 18425901. Archived from the original on 2018-06-12. Retrieved 2018-06-12.
- ↑ Hunt N, McHale S (October 2005). "The psychological impact of alopecia". BMJ (Review). 331 (7522): 951–3. doi:10.1136/bmj.331.7522.951. PMC 1261195. PMID 16239692.
- ↑ Safavi KH, Muller SA, Suman VJ, Moshell AN, Melton LJ (July 1995). "Incidence of alopecia areata in Olmsted County, Minnesota, 1975 through 1989". Mayo Clinic Proceedings. 70 (7): 628–33. doi:10.4065/70.7.628. PMID 7791384.
- ↑ "Search - clinicaltrials.gov for alopecia areata". clinicaltrials.gov. National Institutes of Health. Archived from the original on 8 September 2017. Retrieved 5 April 2016.
- ↑ Mohammadi D (2016). "A ray of hope for alopecia areata patients". The Pharmaceutical Journal. 296 (7889). doi:10.1211/PJ.2016.20201092.
- ↑ Vary JC (November 2015). "Selected Disorders of Skin Appendages--Acne, Alopecia, Hyperhidrosis". The Medical Clinics of North America. 99 (6): 1195–211. doi:10.1016/j.mcna.2015.07.003. PMID 26476248.
- ↑ Rivkin P (September 2016). Alopecia Areata: Jewish Answers to a Modern Disease. pp. 18–33. ISBN 978-1-5375-2975-2.
External links
- National Institute of Arthritis and Musculoskeletal and Skin Diseases Archived 2006-08-21 at the Wayback Machine at NIH
- DermAtlas 42
| Classification | |
|---|---|
| External resources |
- Pages with script errors
- Wikipedia articles needing page number citations from September 2010
- Articles with invalid date parameter in template
- Webarchive template wayback links
- Wikipedia articles needing page number citations from March 2015
- All articles with unsourced statements
- Articles with unsourced statements from August 2020
- Articles with unsourced statements from March 2015
- Articles with unsourced statements from June 2018
- Autoimmune diseases
- Conditions of the skin appendages
- Human hair
- Hair diseases
- RTT
- WHRTT