Acute fatty liver of pregnancy
| Acute fatty liver of pregnancy | |
|---|---|
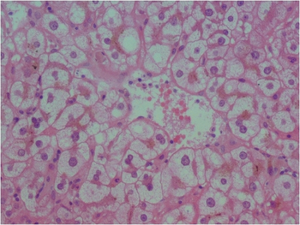 | |
| Liver biopsy in acute fatty liver of pregnancy showing microvesicular fatty infiltration of the hepatocytes | |
| Specialty | Obstetrics, hepatology |
| Symptoms | Early: Nausea, loss of appetite, abdominal pain, high blood pressure[1] Later: Yellow skin, bleeding problems, confusion[1] |
| Complications | Low blood sugar, disseminated intravascular coagulation[1] |
| Usual onset | Third trimester[2] |
| Risk factors | Certain genetic mutations, preeclampsia, male baby or more than one baby, previously being affected[1][3] |
| Diagnostic method | Generally based on symptoms and blood, liver biopsy rarely needed[1] |
| Differential diagnosis | Preeclampsia (HELLP syndrome), viral hepatitis, cholestasis of pregnancy, paracetamol toxicity[2][1] |
| Treatment | Delivery, supportive care[1] |
| Frequency | 1 in 12,500 pregnancies[2] |
| Deaths | 4% (mother),[1] 15% (baby)[3] |
Acute fatty liver of pregnancy (AFLP) is a complication of pregnancy that results in liver failure.[1] Early symptoms may include nausea, loss of appetite, abdominal pain, and high blood pressure.[1] Later symptoms may include yellow skin, bleeding problems, and confusion.[1] Onset is in the third trimester or shortly after delivery.[2]
Risk factors include certain genetic mutations, preeclampsia, a male baby or more than one baby, obesity, diabetes, and previously being affected.[1][3] The underlying mechanism is not entirely clear but may involve long-chain 3-hydroxyacyl-coenzyme A dehydrogenase deficiency or carnitine palmitoyltransferase I deficiency which leads to fat build up in the liver.[1][3] Diagnosis can generally be made based on symptoms and blood tests, without the need for a liver biopsy.[1][3]
Treatment involves supportive care and delivery of the baby.[1] Correction of low blood sugar and electrolyte problems may be required.[1] Delivery may occur by induction or C-section.[1] Rarely liver transplantation is required.[1] With early and rapid treatment, the risk of death for the mother is about 4% and that for the baby is about 15%.[1][3] Problems generally begin resolving a few days after delivery.[3]
Acute fatty liver of pregnancy occurs in about 1 in 12,500 pregnancies.[2] Rates appear to be similar in different cultures.[2] It was mentioned in an obstetrics textbook by John Whitridge Williams in 1903 and described in a case report in 1934.[3][4] Recognition as a separate disease occurred in 1940 when Harold Leeming Sheehan referred to as “acute yellow atrophy of the liver”.[4][2][5]
Signs and symptoms
Acute fatty liver of pregnancy (or hepatic lipidosis of pregnancy) usually manifests in the third trimester of pregnancy, but may occur any time in the second half of pregnancy, or in the puerperium, the period immediately after delivery.[2] On average, the disease presents during the 35th or 36th week of pregnancy.[6] The usual symptoms in the mother are non-specific including nausea, vomiting, anorexia (or lack of desire to eat) and abdominal pain; excessive thirst may be the earliest symptom without overlap with otherwise considered normal pregnancy symptoms;[6] however, jaundice and fever may occur in as many as 70% of patients.[2][7]
In more severe disease, pre-eclampsia may occur, which involves elevation of blood pressure and accumulation of fluid (termed oedema).[6] This may progress to involvement of additional systems, including acute kidney failure,[8] hepatic encephalopathy,[9] and pancreatitis.[10] There have also been reports of diabetes insipidus complicating this condition.[11]
Many laboratory abnormalities are seen. Liver enzymes are elevated, with the AST and ALT enzymes ranging from minimal elevation to 1000 IU/L, but usually staying in the 300-500 range.[2] Bilirubin is almost universally elevated. Alkaline phosphatase is often elevated in pregnancy due to production from the placenta, but may be additionally elevated.[12] Other abnormalities may include an elevated white blood cell count, hypoglycemia, elevated coagulation parameters, including the international normalized ratio, and decreased fibrinogen.[2][12][6] Frank disseminated intravascular coagulation, or DIC, may occur in as many as 70%.[2]
Abdominal ultrasound may show fat deposition in the liver, but, as the hallmark of this condition is microvesicular steatosis, this is not seen on ultrasound.[13] Rarely, the condition can be complicated by rupture or necrosis of the liver, which may be identified by ultrasound.
Pathophysiology

The understanding of the causes of acute fatty liver of pregnancy has been improved by advances in mitochondrial biochemistry. Deficiency of LCHAD (3-hydroxyacyl-CoA dehydrogenase) leads to an accumulation of medium and long chain fatty acids. When this occurs in the foetus, the unmetabolized fatty acids will re-enter the maternal circulation through the placenta, and overwhelm the beta-oxidation enzymes of the mother.[14] The gene responsible for LCHAD has been isolated, and the most common mutation found in acute fatty liver of pregnancy is the E474Q missense mutation.[15] LCHAD deficiency is autosomal recessive in inheritance and mothers are often found to be heterozygous for the affected mutation.[16]
Diagnosis
The diagnosis of acute fatty liver of pregnancy is usually made on clinical grounds by the treating physician, but differentiation from other conditions affecting the liver may be difficult.[2] The diagnosis of acute fatty liver of pregnancy is suggested by jaundice with a lesser elevation of liver enzymes, elevated white blood cell count, disseminated intravascular coagulation, and a clinically unwell patient.[12]
A liver biopsy can provide a definitive diagnosis,[17] but is not always done, due to the increased chance of bleeding in acute fatty liver of pregnancy.[18] Often testing will be done to exclude more common conditions that present in a similar fashion, including viral hepatitis,[19] pre-eclampsia,[6] HELLP syndrome,[12] intrahepatic cholestasis of pregnancy,[2] and autoimmune hepatitis.[20]
Pathology
If a liver biopsy is needed for diagnosis of the condition, the mother should be appropriately stabilized and treated to reduce bleeding related complications. The diagnosis can be made by a frozen-section (as opposed to a specimen in formalin) that is stained with the Oil red O stain, that shows microvesicular steatosis (or small collections of fat within the liver cells). The microvesicular steatosis usually spares zone one of the liver, which is the area closest to the hepatic artery. On the regular trichrome stain, the liver cell cytoplasm shows a foamy appearance due to the prominence of fat. Necrosis is rarely seen. The diagnosis can be enhanced by electron microscopy which can be used to confirm the presence of microvesicular steatosis, and specifically the presence of megamitochondria and paracrystalline inclusions.[21][22] Liver diseases with similar appearances include Reye's syndrome, drug-induced hepatitis from agents with mitochondrial toxicity, including nucleoside reverse transcriptase inhibitors used to treat HIV,[23] and a rare condition known as Jamaican vomiting sickness which is caused by the eating of the unripened Ackee fruit.[24]
Treatment
Acute fatty liver of pregnancy is best treated in a centre with expertise in hepatology, high-risk obstetrics, maternal-fetal medicine and neonatology. The physicians who treat this condition will often consult with experts in liver transplantation in severe cases. Admission to the intensive care unit is recommended.[2]
Initial treatment involves supportive management with intravenous fluids, intravenous glucose and blood products, including fresh frozen plasma and cryoprecipitate to correct DIC. The foetus should be monitored with cardiotocography. After the mother is stabilized, arrangements are usually made for delivery. This may occur vaginally, but, in cases of severe bleeding or compromise of the mother's status, a caesarian section may be needed.[2] Often AFLP is not diagnosed until the mother and baby are in trouble, so it is most likely that an emergency C-section is needed.[citation needed]
The complications of acute fatty liver of pregnancy may require treatment after delivery, especially if pancreatitis occurs.[10] Liver transplantation is rarely required for treatment of the condition, but may be needed for mothers with severe DIC, those with rupture of the liver, or those with severe encephalopathy.[25]
Epidemiology
Acute fatty liver of pregnancy is a rare condition and occurs in approximately one in 7,000 to one in 15,000 pregnancies.[20][22] The mortality from acute fatty liver of pregnancy has been reduced significantly to 18%, and is now related primarily to complications, particularly DIC (Disseminated Intravascular Coagulation) and infections.[2][20] After delivery, most mothers do well, as the stimulus for fatty acid overload is removed. The disease can recur in future pregnancies, with a calculated genetic chance of 25%; the actual rate is lower, however.[14] Mortality of the foetus has also diminished significantly, but still remains 23%,[26] and may be related to the need for premature delivery.[2]
History
The disease was first described in 1940 by H. L. Sheehan as an "acute yellow atrophy" of the liver, then thought to be related to delayed chloroform poisoning.[2][27]
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 1.18 Hadi, Y; Kupec, J (January 2023). "Fatty Liver in Pregnancy". StatPearls. PMID 31424899. Archived from the original on 20 January 2024. Retrieved 18 January 2024.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 2.13 2.14 2.15 2.16 2.17 2.18 Ko H, Yoshida EM (2006). "Acute fatty liver of pregnancy". Canadian Journal of Gastroenterology. 20 (1): 25–30. doi:10.1155/2006/638131. PMC 2538964. PMID 16432556.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 Nelson, DB; Byrne, JJ; Cunningham, FG (1 March 2021). "Acute Fatty Liver of Pregnancy". Obstetrics and gynecology. 137 (3): 535–546. doi:10.1097/AOG.0000000000004289. PMID 33543900.
- ↑ 4.0 4.1 Mandeville, Lisa K.; Troiano, Nan H. (1999). High Risk and Critical Care Intrapartum Nursing. Lippincott Williams & Wilkins. p. 258. ISBN 978-0-397-55467-6. Archived from the original on 20 January 2024. Retrieved 18 January 2024.
- ↑ Weerakkody, Yuranga. "Acute fatty liver of pregnancy | Radiology Reference Article | Radiopaedia.org". Radiopaedia. Archived from the original on 17 December 2023. Retrieved 24 January 2024.
- ↑ 6.0 6.1 6.2 6.3 6.4 Riely CA (1987). "Acute fatty liver of pregnancy". Seminars in Liver Disease. 7 (1): 47–54. doi:10.1055/s-2008-1040563. PMID 3296215.
- ↑ Riely CA, Latham PS, Romero R, Duffy TP (1987). "Acute fatty liver of pregnancy. A reassessment based on observations in nine patients". Annals of Internal Medicine. 106 (5): 703–6. doi:10.7326/0003-4819-106-5-703. PMID 3565968.
- ↑ Koroshi A, Babameto A (2002). "Acute renal failure during acute fatty liver of pregnancy". Nephrology Dialysis Transplantation. 17 (6): 1110–1112. doi:10.1093/ndt/17.6.1110. PMID 12032205.
- ↑ Aggarwal R (2003). "Hepatic encephalopathy in pregnancy". Indian Journal of Gastroenterology. 22 Suppl 2: S78–80. PMID 15025263.
- ↑ 10.0 10.1 Moldenhauer JS, O'brien JM, Barton JR, Sibai B (2004). "Acute fatty liver of pregnancy associated with pancreatitis: a life-threatening complication". American Journal of Obstetrics and Gynecology. 190 (2): 502–505. doi:10.1016/j.ajog.2003.09.022. PMID 14981397.
- ↑ Kennedy S, Hall PM, Seymour AE, Hague WM (1994). "Transient diabetes insipidus and acute fatty liver of pregnancy". BJOG: An International Journal of Obstetrics and Gynaecology. 101 (5): 387–91. doi:10.1111/j.1471-0528.1994.tb11909.x. PMID 8018608. S2CID 11869406.
- ↑ 12.0 12.1 12.2 12.3 Riely CA (1999). "Liver disease in the pregnant patient. American College of Gastroenterology". The American Journal of Gastroenterology. 94 (7): 1728–1732. PMID 10406228.
- ↑ Castro MA, Ouzounian JG, Colletti PM, Shaw KJ, Stein SM, Goodwin TM (1996). "Radiologic studies in acute fatty liver of pregnancy. A review of the literature and 19 new cases". The Journal of Reproductive Medicine. 41 (11): 839–43. PMID 8951135.
- ↑ 14.0 14.1 Tein I (2000). "Metabolic disease in the foetus predisposes to maternal hepatic complications of pregnancy". Pediatric Research. 47 (1): 6–8. doi:10.1203/00006450-200001000-00005. PMID 10625076.
- ↑ IJlst L, Oostheim W, Ruiter JP, Wanders RJ (1997). "Molecular basis of long-chain 3-hydroxyacyl-CoA dehydrogenase deficiency: identification of two new mutations" (PDF). Journal of Inherited Metabolic Disease. 20 (3): 420–422. doi:10.1023/A:1005310903004. PMID 9266371. S2CID 23046057.[permanent dead link]
- ↑ Wanders RJ, Vreken P, den Boer ME, Wijburg FA, van Gennip AH, IJlst L (1999). "Disorders of mitochondrial fatty acyl-CoA beta-oxidation" (PDF). Journal of Inherited Metabolic Disease. 22 (4): 442–487. doi:10.1023/A:1005504223140. PMID 10407780. S2CID 35795159.[permanent dead link]
- ↑ Brunt EM (2000). "Liver biopsy interpretation for the gastroenterologist". Current Gastroenterology Reports. 2 (1): 27–32. doi:10.1007/s11894-000-0048-2. PMID 10981000. S2CID 39207958.
- ↑ Castro MA, Goodwin TM, Shaw KJ, Ouzounian JG, McGehee WG (1996). "Disseminated intravascular coagulation and antithrombin III depression in acute fatty liver of pregnancy". American Journal of Obstetrics and Gynecology. 174 (1 Pt 1): 211–216. doi:10.1016/S0002-9378(96)70396-4. PMID 8572009.
- ↑ Pang WW, Lei CH, Chang DP, Yang TF, Chung YT, Huang MH (1999). "Acute jaundice in pregnancy: acute fatty liver or acute viral hepatitis?". Acta Anaesthesiologica Sinica. 37 (3): 167–70. PMID 10609353.
- ↑ 20.0 20.1 20.2 Mjahed K, Charra B, Hamoudi D, Noun M, Barrou L (2006). "Acute fatty liver of pregnancy". Archives of Gynecology and Obstetrics. 274 (6): 349–353. doi:10.1007/s00404-006-0203-6. PMID 16868757. S2CID 24784165.
- ↑ Bacq Y (1998). "Acute fatty liver of pregnancy". Seminars in Perinatology. 22 (2): 134–140. doi:10.1016/S0146-0005(98)80045-1. PMID 9638907.
- ↑ 22.0 22.1 Reyes H, Sandoval L, Wainstein A, et al. (1994). "Acute fatty liver of pregnancy: a clinical study of 12 episodes in 11 patients". Gut. 35 (1): 101–106. doi:10.1136/gut.35.1.101. PMC 1374642. PMID 8307428.
- ↑ Montessori V, Harris M, Montaner JS (2003). "Hepatotoxicity of nucleoside reverse transcriptase inhibitors". Seminars in Liver Disease. 23 (2): 167–172. doi:10.1055/s-2003-39947. PMID 12800069.
- ↑ Hautekeete ML, Degott C, Benhamou JP (1990). "Microvesicular steatosis of the liver". Acta Clinica Belgica. 45 (5): 311–26. doi:10.1080/17843286.1990.11718105. PMID 2177300.
- ↑ Pereira SP, O'Donohue J, Wendon J, Williams R (1997). "Maternal and perinatal outcome in severe pregnancy-related liver disease". Hepatology. 26 (5): 1258–1262. doi:10.1002/hep.510260525. PMID 9362370.
- ↑ Fesenmeier MF, Coppage KH, Lambers DS, Barton JR, Sibai BM (2005). "Acute fatty liver of pregnancy in 3 tertiary care centers". American Journal of Obstetrics and Gynecology. 192 (5): 1416–1419. doi:10.1016/j.ajog.2004.12.035. PMID 15902124.
- ↑ Sheehan HL (1940). "The pathology of acute yellow atrophy and delayed chloroform poisoning". Journal of Obstetrics and Gynaecology of the British Empire. 47: 49–62. doi:10.1111/j.1471-0528.1940.tb14731.x. S2CID 72493420.
External links
| Classification |
|---|
- Pages with script errors
- CS1: long volume value
- All articles with dead external links
- Articles with dead external links from February 2022
- Articles with invalid date parameter in template
- Articles with permanently dead external links
- All articles with unsourced statements
- Articles with unsourced statements from November 2017
- Diseases of liver
- Autosomal recessive disorders
- Maternal disorders predominantly related to pregnancy
- Fatty-acid metabolism disorders
- RTT
- WHRTT