Acute prostatitis
| Acute prostatitis | |
|---|---|
| Other names: Acute bacterial prostatitis[1] | |
 | |
| Specialty | Urology |
| Symptoms | Sudden onset pelvic pain, fever, pain with urination[2] |
| Complications | Urinary retention, prostate abscess, sepsis, chronic prostatitis[2][3] |
| Usual onset | 20s or 30s[1] |
| Causes | Bacterial infection[2] |
| Risk factors | Urinary tract infection, urinary catheter, prostate biopsy, sexually transmitted infection, anal sex[2] |
| Diagnostic method | Based on symptoms, examination, urine testing[1] |
| Differential diagnosis | Pyelonephritis, urethritis, prostate cancer[3] |
| Treatment | Antibiotics, pain medication[2] |
| Frequency | Rare[3] |
Acute prostatitis is a type of prostatitis which is sudden in onset.[2] Symptoms may include significant pelvic or lower back pain, fever, and pain with urination.[2] Complications may include urinary retention, prostate abscess, sepsis, and chronic prostatitis.[2][3]
Acute prostatitis is usually due to a bacterial infection of the prostate gland.[2] While various types of bacteria may be involved, E. coli is most common.[1] Risk factors include urinary tract infections, urinary catheters, prostate biopsy, sexually transmitted infections, and anal sex.[2] Diagnosis is generally based on symptoms, examination and urine testing.[1] Doing a prostate massage during the exam is not recommended.[1]
Treatment is generally with antibiotics for two to four weeks.[2] Pain medications may also be required.[2] A urinary catheter may be placed if retention is present.[2] Alpha blockers and NSAIDs may be useful to decrease the swelling.[1] Outcomes are usually good with treatment.[2]
Acute prostatitis is rare.[3] It makes up about 5 to 10% of prostatitis cases.[3] Those in their 20s and 30s are most commonly affected.[1] Prostatitis was first described by Verdies in 1838.[4]
Signs and symptoms
Men with acute prostatitis often have chills, fever, pain in the lower back, perineum, or genital area, urinary frequency and urgency often at night, burning or painful urination, body aches, and a demonstrable infection of the urinary tract, as evidenced by white blood cells and bacteria in the urine. Acute prostatitis may be a complication of prostate biopsy.[5] Often, the prostate gland is very tender to palpation through the rectum.[6]
Diagnosis
Acute prostatitis is relatively easy to diagnose due to its symptoms that suggest infection. The organism may be found in blood or urine, and sometimes in both.[5] Common bacteria are Escherichia coli, Klebsiella, Proteus, Pseudomonas, Enterobacter, Enterococcus, Serratia, and Staphylococcus aureus. This can be a medical emergency in some patients and hospitalization with intravenous antibiotics may be required. A complete blood count reveals increased white blood cells. Sepsis from prostatitis is very rare, but may occur in immunocompromised patients; high fever and malaise generally prompt blood cultures, which are often positive in sepsis. A prostate massage should never be done in a patient with suspected acute prostatitis, since it may induce sepsis. Since bacteria causing the prostatitis is easily recoverable from the urine, prostate massage is not required to make the diagnosis. Rectal palpation usually reveals an enlarged, exquisitely tender, swollen prostate gland, which is firm, warm, and, occasionally, irregular to the touch. C-reactive protein is elevated in most cases.[7]
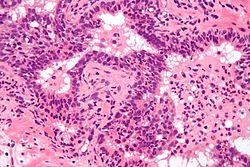
Prostate biopsies are not indicated as the (clinical) features (described above) are diagnostic. The histologic correlate of acute prostatitis is a neutrophilic infiltration of the prostate gland.[citation needed]
Acute prostatitis is associated with a transiently elevated PSA, i.e., the PSA is increased during an episode of acute prostatitis and then decreases again after it has resolved. PSA testing is not indicated in the context of uncomplicated acute prostatitis. Other diagnostic methods include ultrasound.[citation needed]
-
Abscess of the prostate (red arrow) resulting in urinary retention (blue arrow)
-
Abscess of the prostate (red arrow) resulting in urinary retention (blue arrow)
-
Micrograph showing a neutrophilic infiltration of prostatic glands - the histologic correlate of acute prostatitis.
Differential diagnosis
It should be distinguished from other forms of prostatitis such as chronic bacterial prostatitis and chronic pelvic pain syndrome (CPPS).
Treatment
Antibiotics are the first line of treatment in acute prostatitis. Antibiotics usually resolve acute prostatitis infections in a very short time, however a minimum of two to four weeks of therapy is recommended to eradicate the offending organism completely.[8] Appropriate antibiotics should be used, based on the microbe causing the infection. Some antibiotics have very poor penetration of the prostatic capsule, others, such as ciprofloxacin, trimethoprim/sulfamethoxazole, and tetracyclines such as doxycycline penetrate prostatic tissue well. In acute prostatitis, penetration of the prostate is not as important as for category II because the intense inflammation disrupts the prostate-blood barrier. It is more important to choose a bactericidal antibiotic (kills bacteria, e.g., a fluoroquinolone antibiotic) rather than a bacteriostatic antibiotic (slows bacterial growth, e.g. tetracycline) for acute potentially life-threatening infections.[9]
People who are severely ill may need hospitalization, while others can be treated at home with bed rest, analgesics, stool softeners, and hydration. Men with acute prostatitis complicated by urinary retention are best managed with a suprapubic catheter or intermittent catheterization. Lack of response to antibiotics should raise the suspicion of an prostate abscess and prompt an imaging study such as a transrectal ultrasound (TRUS).[10]
Prognosis
Full recovery without sequelae is usual.[citation needed]
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 Khan, FU; Ihsan, AU; Khan, HU; Jana, R; Wazir, J; Khongorzul, P; Waqar, M; Zhou, X (October 2017). "Comprehensive overview of prostatitis". Biomedicine & pharmacotherapy = Biomedecine & pharmacotherapie. 94: 1064–1076. doi:10.1016/j.biopha.2017.08.016. PMID 28813783.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 2.13 "Prostatitis". nhs.uk. 19 October 2017. Archived from the original on 17 October 2017. Retrieved 7 November 2020.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 Davis, NG; Silberman, M (January 2020). "Bacterial Acute Prostatitis". PMID 29083799.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ Partin, Alan W.; Wein, Alan J.; Kavoussi, Louis R.; Peters, Craig A.; Dmochowski, Roger R. (2020). Campbell Walsh Wein Urology, E-Book. Elsevier Health Sciences. p. 1202. ISBN 978-0-323-67227-6. Archived from the original on 2021-08-27. Retrieved 2020-11-08.
- ↑ 5.0 5.1 Stoica G, Cariou G, Colau A, et al. (2007). "[Epidemiology and treatment of acute prostatitis after prostatic biopsy]". Prog. Urol. (in French). 17 (5): 960–3. doi:10.1016/S1166-7087(07)92397-0. PMID 17969797.
{{cite journal}}: CS1 maint: unrecognized language (link) - ↑ Goldman, Lee (2011). Goldman's Cecil Medicine (24th ed.). Philadelphia: Elsevier Saunders. p. 808. ISBN 978-1437727883.
- ↑ Auzanneau C, Manunta A, Vincendeau S, Patard JJ, Guillé F, Lobel B (2005). "[Management of acute prostatitis, based on a series of 100 cases]". Prog. Urol. (in French). 15 (1): 40–4. PMID 15822390.
{{cite journal}}: CS1 maint: unrecognized language (link) - ↑ Easley, Susan K.; Stevermer, James J. (2000-05-15). "Treatment of Prostatitis". American Family Physician. 61 (10): 3015–3022. PMID 10839552. Archived from the original on 2018-03-14. Retrieved 2013-05-08.AAFP Prostatitis Treatment Article
- ↑ Hua VN, Schaeffer AJ (2004). "Acute and chronic prostatitis". Med. Clin. North Am. 88 (2): 483–94. doi:10.1016/S0025-7125(03)00169-X. PMID 15049589.
- ↑ Göğüş C, Ozden E, Karaboğa R, Yağci C (2004). "The value of transrectal ultrasound guided needle aspiration in treatment of prostatic abscess". European Journal of Radiology. 52 (1): 94–8. doi:10.1016/S0720-048X(03)00231-6. PMID 15380852.
External links
| Classification | |
|---|---|
| External resources |
- Pages with script errors
- CS1 errors: missing periodical
- CS1 maint: unrecognized language
- All articles with unsourced statements
- Articles with unsourced statements from September 2020
- Articles with invalid date parameter in template
- Articles with Curlie links
- Bacterial diseases
- Sexually transmitted diseases and infections
- Medical emergencies
- Inflammatory prostate disorders
- RTT